Abstract
Abstract 2522
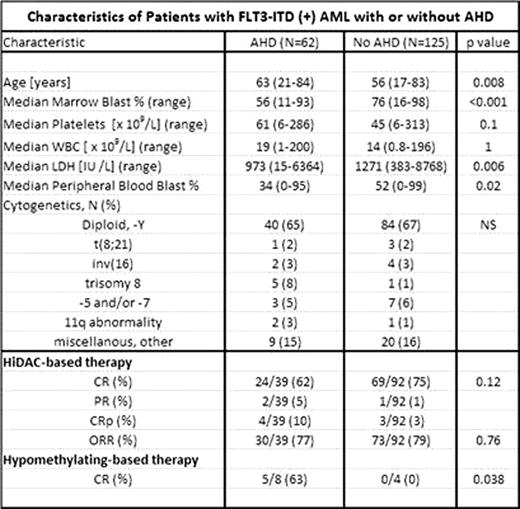
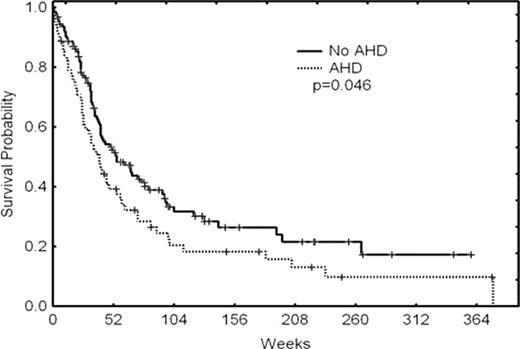
Internal tandem duplication (ITD) mutations in FLT3 (fms-like tyrosine kinase III) are common in acute myeloid leukemia (AML) and are associated with increased relapse risk and adverse outcome. A subset of AML, arising from an antecedent hematologic disorder (AHD) such as myelodysplastic syndrome (MDS), is also associated with an adverse outcome. We sought to review our experience and define the incidence, characteristics, and outcome of FLT3-ITD in AML arising from AHD. We reviewed all cases of newly diagnosed AML, excluding acute promyelocytic leukemia from 2001–2010 at our institution. FLT3-ITD mutational analysis was performed using PCR-based DNA sequencing on 1254 cases. Overall, 187 (15%) patients (pts) had FLT3-ITD mutations. Of the 1254 pts, 545 (43%) were classified as having an AHD and 709 (57%) were not. The incidence of FLT3-ITD in pts with and without AHD was 11% (125/709) and 18% (62/545), respectively (p=0.002). As a separate analysis, among pts who had received any prior chemotherapy or radiation, the incidence of FLT3-ITD was 8% (17/201) vs. 16% (170/1053) in those who had not (p=0.005). Baseline characteristics of the patients with FLT3-ITD positive AML with or without AHD are shown in table 1. The 187 pts with FLT3-ITD were treated with several different therapies as their initial treatment for AML. These included: high dose cytarabine-based (HiDAC) in 131 (70%), conventional dose cytarabine-based in 28 (15%), hypomethylating agents (HMA) in 12 (6%), and other in 16 (9%). The response rates to HiDAC and HMA in each of the two cohorts is shown in table 1. The median overall survival of patients with FLT3-ITD and AHD was 40 weeks vs. 54 weeks in those without AHD (p=0.046, Figure 1). In conclusion, FLT3-ITD is relatively less common in AML arising from AHD and in therapy-related AML compared to de novo AML. AML pts with FLT3-ITD and AHD tend to be older, have a lower bone marrow and peripheral blasts, a lower serum LDH, and significantly shorter overall survival. Compared to those without AHD, the response rate to HiDAC-based therapy in patients with FLT3-ITD and AHD are similar, but the response rates to HMA-based therapy are higher. The role of HMA in the treatment of FLT3-ITD patients with and without AHD should be investigated further.
Figure 1.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2011 by The American Society of Hematology
2011

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal