Abstract
Long-term efficacy and safety of the iron chelator deferasirox in SCD patients has been previously reported (Vichinsky et al. BJH 2011). Hydroxyurea (HU), a common treatment for SCD, is associated with adverse events (AEs) such as bone marrow depression. However, long-term data for iron chelation and concomitant HU are limited. This study provides further efficacy and safety data for deferasirox including PK and safety data + HU.
SCD patients aged ≥2 yrs and iron overload from blood transfusions were enrolled and randomized 2:1 to deferasirox (DFX; 20 mg/kg/day) or deferoxamine (DFO; 175 mg/kg/week [wk]) for 24 wks (24-wk DFX or DFO cohort). DFO patients then crossed over to DFX; all patients received DFX up to Wk 52. Patients entered a 52-wk extension receiving DFX (DFX up to 2 yrs cohort). PK sampling was carried out pre- and 2 hrs post-dose in patients on DFX at Wk 12. Plasma concentrations of DFX and iron-complex Fe-[DFX]2 were determined using a validated LC-MS/MS method. Dose adjustments were implemented for changes in patient weight, serum ferritin, serum creatinine, liver function tests and rash. Primary objective was DFX safety compared with DFO during 24 wks. Secondary objectives included DFX safety and efficacy for up to 2 yrs and DFX safety in patients with concomitant HU.
24-weeks, DFX (n=135) vs DFO (n=68).
Patients were severely iron overloaded at baseline (BL); 37% had serum ferritin ≥4000 ng/mL (median 3385 ng/mL). In the DFX and DFO cohorts, respectively, 93 and 78% of patients completed 24 wks of treatment. AEs leading to discontinuation were reported by 0 and 1 (1.8%) patient in the DFX and DFO cohorts, respectively. Investigator-assessed drug-related AEs were reported in 27 and 29% of patients in the DFX vs DFO cohort, respectively; most common (>5%) were gastrointestinal (DFX vs DFO cohort: diarrhea 10.4 vs 3.6%; nausea 5.2 vs 3.6%). Serious AEs (any causality) were reported in 30 and 36% of patients in the DFX vs DFO cohort, respectively. One death occurred in the DFX cohort, not considered drug-related (patient had past history of multi-organ failure). At the 3–6 month timepoint, median change from BL in serum ferritin was –196 (range –4029 to 10,168) and –400 (range –10,001 to 3908) ng/mL for DFX (n=130) and DFO (n=58) cohorts, respectively.
Up to 2 years DFX (n=188).
135 (72%) patients who received DFX completed the study; 5 (3%) patients discontinued due to AEs. Average actual dose was 21.2 ± 3.6 mg/kg/day. Most common investigator-assessed drug-related AEs (>5%) were diarrhea (11.7%), nausea (6.9%) and abdominal pain (5.3%). Drug-related serious AEs were reported in 8 (4.3%) patients; most common were increased aspartate aminotransferase (AST) and abnormal liver function test (n=2, for each). One additional death occurred; not considered drug-related (patient had history of congestive heart failure with worsening pulmonary hypertension). 4 patients had 2 consecutive serum creatinine increases >33% above BL and >upper limit of normal; increases were transient and resolved with dose adjustment or temporary interruption. Mean ± SE change from BL in serum ferritin (per-protocol, adjusted for amount of transfused blood) was –683 ± 205 ng/mL (n=87).
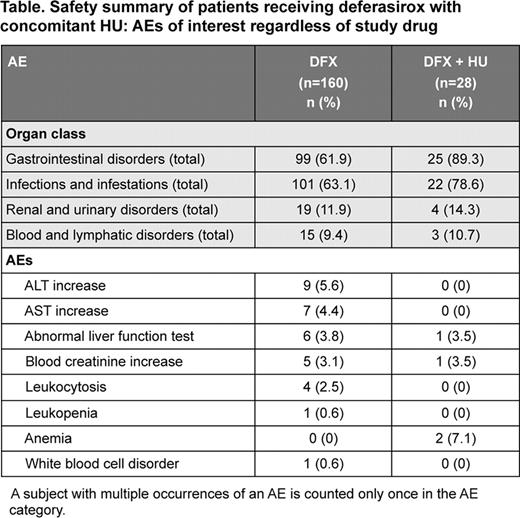
PK, safety and efficacy of DFX + HU (n=28) and DFX (n=160).
Mean DFX concentration (μmol/L) pre- and 2-hr post-dose were similar in patients receiving DFX + HU (n=14) vs DFX (n=81); pre-dose 13.3 vs 19.8, post-dose 74.2 vs 79.4. Mean Fe-[DFX]2 concentration (μmol/L) pre- and post-dose was similar in patients receiving DFX + HU (n=14) vs DFX (n=85); pre-dose 0.9 vs 0.6, post-dose 1.9 vs 1.7. One of 5 patients discontinuing DFX due to AEs was receiving concomitant HU. Overall the type and incidence of AEs in patients receiving DFX + HU vs DFX were similar (Table). At the 21–24 month time-point, mean change in serum ferritin was –593 ng/mL (n=15) and –721 ng/mL (n=81) for DFX + HU vs DFX cohorts, respectively.
Consistent with previous studies, this study confirms that deferasirox has a clinically manageable safety profile, and is comparable overall with DFO in SCD patients, with many AEs related to the underlying condition (eg, sickle cell anemia with crisis, pyrexia, infections). This study confirms the long-term efficacy of deferasirox with clinically meaningful reductions in serum ferritin over 2 years. PK, efficacy and overall safety of deferasirox were not influenced by concomitant HU.
Vichinsky:Novartis: Honoraria, Research Funding. Habr:Novartis: Employment. Lynch:Novartis: Employment. Zhang:Novartis: Employment. Files:Novartis: Speakers Bureau; Medical University of South Carolina: Research contract agreement.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal