Abstract
A major issue in immunosuppressive biotherapy is the use of mesenchymal stem cells (MSCs) that harbor regulatory capacity. However, currently used bone marrow-derived MSCs (BM-MSCs) are short-lived and cannot assure long lasting immunoregulatory function both in vitro and in vivo. Consequently, we have generated MSCs from human induced pluripotent stem (IPS-MSCs) cells that share similar properties with embryonic stem cells (ES-MSCs). Herein, we compared the immunoregulatory properties of ES/IPS-MSCs with those of BM-MSCs and showed, for the first time, that IPS-derived MSCs display remarkable inhibition of NK-cell proliferation and cytolytic function in a similar way to ES-MSCs. Both MSCs disrupt NK-cell cytolytic machinery in the same fashion that BM-MSCs, by down-regulating the expression of different activation markers and ERK1/2 signaling, leading to an impairment to form immunologic synapses with target cells and, therefore, secretion of cytotoxic granules. In addition, they are more resistant than adult BM-MSCs to preactivated NK cells. IPS-MSCs could represent an attractive alternative source of immunoregulatory cells, and their capacity to impair NK-cell cytotoxicity constitutes a complex mechanism to prevent allograft rejection.
Introduction
Mesenchymal stem cells (MSCs) are important tools in treating immune disorders and in tissue repair by their multipotency, immunosuppressive properties, and production of cytokines or growth factors, Many sources of MSCs have been described and the main candidates for clinical application are bone marrow and adipocyte tissues widely available and easy to collect by standardized procedures. However, as they have in vitro and in vivo time-limited functions,1,2 several research groups are searching for MSCs with prolonged lifetime and immunoregulatory properties. In the last decade, MSCs have been isolated from fetal or neonatal tissues3-7 and embryonic tissues (ES-MSCs).8-10 At present, no specific markers for the origin of the MSCs have been identified and all types of MSCs are defined by their CD105, CD90, CD73, CD44, CD29, CD146, and CD166 expression. Adult BM-MSCs exhibit immunomodulatory functions on immune cells by both cell–cell contact and soluble factors.2,11-13 Recently, human somatic cells have been successfully reprogrammed into induced pluripotent cells (iPSC)14-19 that exhibit characteristics similar to human ES.20 IPSC hold enormous promise for personalized cell-replacement therapy21 and for research into various human diseases.22,23 Therefore, MSCs derived from iPSC may be a novel source of tolerance induction, though their immunosuppressive activity remains to be explored.
We report that MSCs isolated from diverse human iPS Cell lines (iPS-MSCs) can strongly inhibit the cytotoxic functions of natural killer (NK) cells. Most of these MSC-mediated inhibitory effects are because of a general impairment of NK activation and disruption of the secretory machinery on NK cells. Interestingly, iPS-MSCs and ES-MSCs are more resistant than BM-MSCs to preactivated NK cells. Our current data indicate that iPS-MSCs could represent a promising alternative strategy for the treatment of various immune-mediated diseases.
Methods
Reagents
The antibodies used to assess NK and MSC phenotypes are described in supplemental Table 1 (available on the Blood Web site; see the Supplemental Materials link at the top of the online article). Recombinant human IL-2 was purchased from Immunotools, whereas Mitomycin, Monensin, and Brefaldin were purchased from Sigma-Aldrich. 1-Methyl-tryptophan (1-MT) and NS-398, specific inhibitors for Indoleamine 2,3-dioxygenase (IDO) and Prostaglandin (PGE)–2, respectively, were also purchased from Sigma-Aldrich. 87G antagonist antibody anti–HLA-G was purchased from Exbio.
Pluripotent stem-cell lines
We used 3 human iPS cell lines PB3, PB10, and PB11 provided from the Stem cell Core-Facility (ES Team Paris Sud, University Paris 11, Villejuif, France) that were derived from amniotic fluid cells (AFC-iPS) after amniocentesis (Antoine Béclère Hospital, Clamart France). Their pluripotency was validated by teratoma assay, flow cytometry and RT-PCR and registered into the European Registry Web site (http://www.hescreg.eu). In addition, we derived 2 iPS from human embryonic stem cell–derived MSCs by transducing Oct-4, Sox2, Nanog, and Lin28 transgenes19 using lentiviral vectors. MSCs were generated from 2 ES cell lines H9 (WiCell Research Institute; http://www.wicell.org) and SA-01-ES (Cellartis). Briefly, 1 × 106 infected ES-MSCs were plated on inactivated mouse embryonic fibroblasts (MEF) in a DMEM/F12 culture medium supplemented with 20% knockout serum replacement, 10 ng/mL bFGF, 0.1mM nonessential amino acids, 1mM l-glutamine, 0.1mM ß-mercaptoethanol, and 1× penicillin–streptomycin (all from Invitrogen). After 15-25 days of culture, individual ES-like colonies were manually picked for expansion and characterization. H9-iPS and SA01-iPS stained positively Tra1-60 (BD Biosciences) HESCA-1 and SSEA-4 (Flow Cellect Human ESC Surface Marker Characterization Kit; Millipore) by flow cytometry and formed mature teratoma containing tissues of all 3 germ layers after injection of 5 × 105 to 3 × 106 undifferentiated cells into the hind leg muscle of NOD SCID mice. RT-PCR analysis confirmed a strong endogenous expression of Oct4, Sox 2, Nanog, and a complete extinction of the transgene. All iPS were cultured in α-MEM complete medium supplemented with bFGF (1 ng/mL) at 37°C, in air, with 5% CO2.
Generation of mesenchymal stem cells
MSCs generated from pluripotent stem cells.
Mesenchymal stem cell were obtain from 2 ES cells (H9 and SA-01 and called H9-MSC, SA-01-MSC) and from 5 iPS cells (H9-iPS, SA-01-iPS, PB03, PB10, PB11 and called iPS-MSC) after culture during 4 weeks in DMEM/F12 (Invitrogen) medium, supplemented with 10% heat-inactivated FBS (Hyclone), 1 ng/mL b-FGF, 0.1mM nonessential amino acids, 1mM l-glutamine, 0.1mM ß-mercaptoethanol and 1× penicillin-streptomycin (all from Invitrogen). Adherent cells after 4 weeks of culture were characterized by flow cytometry exploring the expression of CD90, CD105, CD146, CD54 (ICAM-1), CD73, CD34, CD45, HLA class I (HLA-ABC) and class II (HLA-DR), and the pluripotent markers Oct4, Sox2, Nanog, and Lin28. Multipotency of MSCs was tested for differentiation along the osteogenic, chondrogenic, and adipogenic lineages. The adipocytes, chondrocytes and osteocytes lineages were respectively confirmed by immunohistochemistry using polyclonal goat anti–mouse FABP-4, monoclonal goat anti–human Aggrecan and mouse anti–human Osteocalcin antibodies. iPS-MSCs carried normal karyotype in culture at passage 5-10 and were used for the studies of NK-cell cytotoxicity assay.
MSCs derived from adult bone marrow.
BM-MSCs from 3 healthy human donors were provided by Dr Lataillade (CTSA Hôpital Percy, Clamart, France). In this study, BM-MSCs at passage 3 were used as a positive control in the NK-cell cytotoxicity assay.
Isolation of NK cells and cell lines
NK cells were isolated from 2 PBMC donors by negative selection using the RosetteSep method (StemCell Technologies), according to the manufacturer's instructions. Freshly purified CD56+/CD3− (> 95%, as checked by flow cytometry) NK cells were stimulated with IL-2 (250 U/mL) and were used immediately in functional assays. Cells were plated (106 cells/mL) in flat-bottom 96-well tissue-culture plates in the presence or absence of mitomycin-treated (25 μg/mL, 30 minutes at 37°C) IPS-MSCs at a 4:1 ratio of NK/MSC. After 4 days, NK cells were assessed for their cytolytic activity, cytokine production and surface phenotype. The HLA class I- K562 cell line was used as a target in the NK-cell cytotoxicity analysis. In other experiments, NK cells were resuspended in PBS/FCS 5% and labeled with 5μM CFSE (Molecular Probes) for 5 minutes at 37°C to assess their proliferation.
51Chromium-release assay
A NK-sensitive K562 cell line was used as the target cell in a conventional 51Cr-release assay. NK cells were mixed with 51Cr-labeled K562 target cells (2500/well) at different effector-to-target (E/T) ratios. After 4 hours, the supernatants were harvested and transferred to LumaPlate 96-well plates (Perkin–Elmer), and were dried and counted on a Packard's TopCount NXT. The percentage of specific lysis was calculated as follows: percent specific lysis = (counts per million [cpm] sample – cpm spontaneous/cpm max. – cpm spontaneous) × 100. Each point represents the average of triplicate values. Maximal release was obtained with 2% Triton X-100. In other experiments, IL-2–activated NK cells were cultured with 51Cr-labeled–MSCs at different ratios to investigate the susceptibility of MSCs to being killed by NK cells.
Flow cytometry and cytolytic degranulation
For surface-marker expression, cells were stained with saturating concentrations of the appropriate mAbs or isotype-matched control Ab, for 30 minutes at 4°C in the dark. NK cells were also tested for their cytolytic activity against NK susceptible target cells by quantifying surface expression of CD107a, as previously described.24 Monensin (2mM) was added for the last 4 hours to inhibit cytokine secretion. In some experiments, K562 cells and MSCs were stained with anti–Apo2.7-PE to evaluate their apoptosis after coculture with activated NK cells for 4 hours. Cells were analyzed using a FACScan flow cytometer using CellQuest Analysis Version 3.3 software (BD Biosciences).
NK immunologic synapse (NKIS)
K562 or MSCs were mixed with NK cells (ratio NK/target 2:1) and spread onto poly-L-lysine–coated slides (Sigma-Aldrich) for 20 minutes at 37°C. Cells were fixed and treated for 15 minutes with PBS containing 5% FCS to quench aldehyde groups. Cells were then permeabilized with PBS/BSA 0.5%/saponin 0.3% and stained with anti-phospho-tyrosine (4G10, Upstate Biotechnology) and granzyme B (Alexis Biotechnical), followed by Alexa Fluor 488–conjugate anti–mouse IgG. Slides were mounted with Mowiol (Sigma-Aldrich) and analyzed using a Coolsnap camera HQ2 on a Leica DMR system. Images of phase-contrast microscopy were analyzed using Metavue Version 7.1.4.0 software (Universal Imaging). Cell conjugates at the synapse were quantified with ImageJ software and their percentage was assessed in randomly selected fields. Differential interference contrast (DIC) images were collected simultaneously with the fluorescent images.
Protein isolation and Western blot analysis
Western blot analysis was performed to measure GAPDH, PI3K (p85), granzyme B protein contain, and ERK phosphorylation. Protein concentration was determined using the BCA protein assay reagent (Pierce). Equivalent protein extracts (20-40 μg/lane) for each sample were denatured by boiling in SDS-polyacrylamide and β-mercaptoethanol, separated by SDS-PAGE gel electrophoresis (7%-12%) and transferred to nitrocellulose membranes. The efficiency of the electrotransfer was assessed by Ponceau red staining. Membranes were probed with primary antibodies and then incubated with peroxide-conjugated secondary antibodies. They were saturated for 1 hour at room temperature in TBS-0.1% Tween-20 and incubated with specific monoclonal antibody (see details in supplemental Table), followed by incubation with HRP-conjugated anti–rabbit or anti–mouse IgG secondary antibody (Biotest Diagnostics, 1:1500). Detection used a SuperSignal West Pico stable peroxide solution (Pierce) and an ECL detection system (Amersham Biosciences) was used according to the manufacturer's instructions. Quantification of the blotted protein was determined using Fujifilm Intelligent Dark Box II and Image Gauge Version 4.0 software.
Cytokine detection by ELISA
Cultured cell supernatants were harvested after 4 days of coculture and tested in triplicate for production of IFN-γ (eBioscience), total HLA-G (Exbio), and PGE-2 (R&D Systems) by ELISA, according to the manufacturer's instructions. The ELISA plates were read at OD450 nm on a Microplate ELISA reader (Titertek multiskan plus).
Data analysis
Statistical analysis was performed using GraphPad Prism software (GraphPad). All experiments were performed in at least 3 independent assays, which gave highly comparable results. Data are presented as mean ± SD. The statistical significance (P values) of the results was calculated using the 2-tailed Student t test. A P < .05 was considered statistically significant. Informed written approval was obtained from the Inserm Institutional Review Board for these studies. Informed consent was provided according to the Declaration of Helsinki.
Results
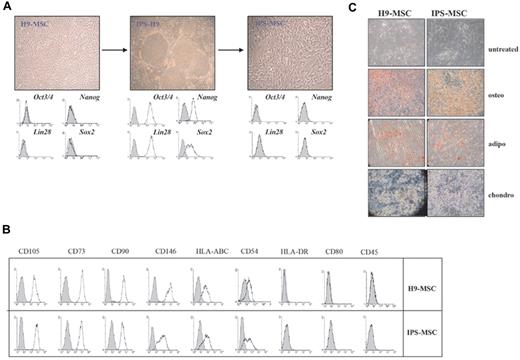
Characterization of human MSC-derived iPS
To compare the functional properties of MSC-derived iPS with their parental embryonic MSCs of the same genetic background we generated iPS cell line from 2 embryonic MSCs (H9 and SA01). In addition we explored the MSC functions from 3 iPS generated from Amniotic fluid Cells. IPS-MSCs showed a spindle-shaped morphology (Figure 1A) and all shares the same phenotype than ES-MSCs (trivedi) and BM-MSCs.25 They were positive for CD90, CD105, CD146, CD54 (ICAM-1), CD73; expressed an intermediate level of HLA class I (HLA-ABC); and were negative for hematopoietic markers (CD45), HLA class II (HLA-DR), and costimulatory molecules (Figure 1B). IPS-MSCs did not express the reprogramming factors Oct3/4, Sox-2, Nanog, and Lin-28 (Figure 1A) neither the transgene measured by RT-PCR (data not shown). IPS-MSCs were multipotent and able to differentiate into adipogenic, chondrogenic and osteogenic lineages (Figure 1C).
Characterization of human IPS-MSCs and H9-MSCs. (A) Morphology of MSCs and iPS: H9-MSCs and IPS-MSCs were characterized by spindle-cell morphology (original magnification, 40×) and iPS-H9 colonies by ES-like morphology. (B) Expression of pluripotent markers in MSCs and iPS by flow cytometry. FACS analysis of Oct-4, Nanog, Lin 28 and Sox-2 were performed after permeabilization in PFA 3%/Saponin 0.1% in MSC-H9 before reprogramming, iPSC-H9 and iPS-differentiated MSCs. Marker expression is presented as histograms. Filled histograms indicate a negative isotype. (C) Immunohistochemical staining of surface antigens on human H9-MSCs and IPS-MSCs after differentiation toward adipogenic, osteogenic, and chondrogenic lineages (original magnification, 40×). Staining with alizarin red shows development of calcium accumulation under inductive osteogenic conditions, in vitro, for 4 weeks, whereas oil red O staining shows development of lipid accumulation under inductive adipogenic conditions, in vitro, for 4 weeks. Alcian blue stain was used to detect extracellular matrix proteoglycans under inductive chondrogenic conditions, in vitro, for 4 weeks.
Characterization of human IPS-MSCs and H9-MSCs. (A) Morphology of MSCs and iPS: H9-MSCs and IPS-MSCs were characterized by spindle-cell morphology (original magnification, 40×) and iPS-H9 colonies by ES-like morphology. (B) Expression of pluripotent markers in MSCs and iPS by flow cytometry. FACS analysis of Oct-4, Nanog, Lin 28 and Sox-2 were performed after permeabilization in PFA 3%/Saponin 0.1% in MSC-H9 before reprogramming, iPSC-H9 and iPS-differentiated MSCs. Marker expression is presented as histograms. Filled histograms indicate a negative isotype. (C) Immunohistochemical staining of surface antigens on human H9-MSCs and IPS-MSCs after differentiation toward adipogenic, osteogenic, and chondrogenic lineages (original magnification, 40×). Staining with alizarin red shows development of calcium accumulation under inductive osteogenic conditions, in vitro, for 4 weeks, whereas oil red O staining shows development of lipid accumulation under inductive adipogenic conditions, in vitro, for 4 weeks. Alcian blue stain was used to detect extracellular matrix proteoglycans under inductive chondrogenic conditions, in vitro, for 4 weeks.
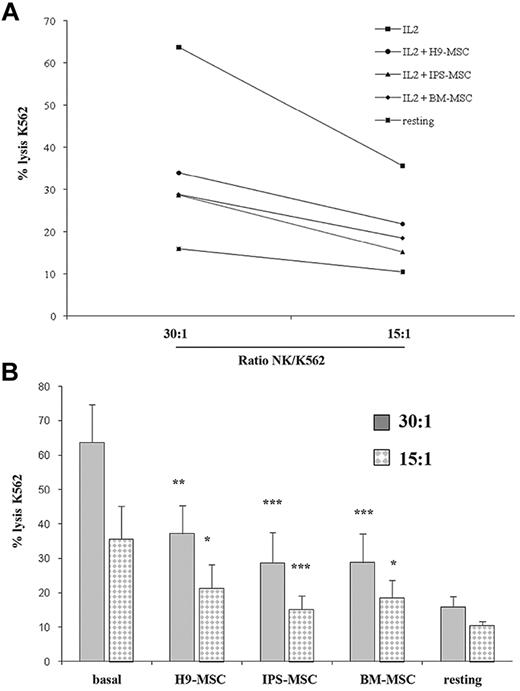
IPS-MSCs inhibit IL-2–activated NK-cell cytotoxicity
Since BM-MSCs inhibit NK-cell cytotoxicity,26,34 we investigated the role of MSC-derived iPS on NK cytotoxic function in comparison with embryonic-MSCs and BM-MSCs. Whereas resting NK cells were minimally cytotoxic against K562 cells, IL-2–activated NK cells exhibited strong killing in a ratio-dependent manner, which was efficiently impaired by the 5 IPS-MSCs, H9-MSCs, SA01-MSCs, and BM-MSCs (Figure 2). In agreement with others, our results show that BM-MSCs were able to down-regulate NK-cell function.26 Interestingly, the inhibition of NK lysis mediated by MSC-derived iPS was comparable to BM-MSCs and the embryonic MSCs. We confirmed that iPS-MSCs are efficient immunosuppressors as adult BM-MSCs.
IPS-MSCs impair NK cytotoxicity. (A) NK cells were tested in a 4-h 51Cr-release assay against K562 cells at different effector/target ratios. NK cells were cultured in medium alone (resting) or were supplemented with IL-2 (250 U/mL) (■), BM-MSCs (♦), H9-MSCs (●), or IPS-MSCs (▴; NK/MSC ratio, 4:1) before the assays. (B) The bar graphs represent the percentage release of 51Cr at 30:1 and 15:1 NK/K562 ratios. Results are representative of 5 independent experiments and are shown as the means ± SD of triplicate samples. Statistically significant differences between NK cells cultured with or with MSCs are indicated by asterisks. ***P < .001; **P < .01 compared with IL-2–activated NK cells alone.
IPS-MSCs impair NK cytotoxicity. (A) NK cells were tested in a 4-h 51Cr-release assay against K562 cells at different effector/target ratios. NK cells were cultured in medium alone (resting) or were supplemented with IL-2 (250 U/mL) (■), BM-MSCs (♦), H9-MSCs (●), or IPS-MSCs (▴; NK/MSC ratio, 4:1) before the assays. (B) The bar graphs represent the percentage release of 51Cr at 30:1 and 15:1 NK/K562 ratios. Results are representative of 5 independent experiments and are shown as the means ± SD of triplicate samples. Statistically significant differences between NK cells cultured with or with MSCs are indicated by asterisks. ***P < .001; **P < .01 compared with IL-2–activated NK cells alone.
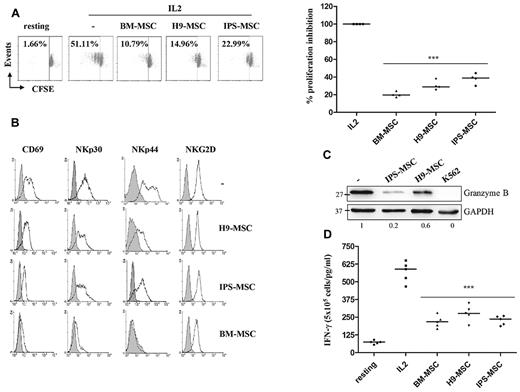
IPS-MSCs prevent NK-cell proliferation and activation
IL-2–activated NK cells were cocultured for 4 days with or without the 5 iPS-MSCs, the embryonic MSCs (H9-MSC, SA-01-MSC) or adult BM-MSCs, to assess their impact on NK-cell activities. As evaluated by the CFSE dilution assay, both IPS-MSCs and H9-MSCs prevented the proliferation of activated NK cells (Figure 3A) as the BM-MSCs. In addition, significant down-modulation of NK-cell receptors CD69, NKp30, and NKp44 was observed after interaction of NK cells with BM-MSCs (Figure 3B), whereas NKG2D expression was not significantly modified by IPS-MSCs and H9-MSCs. In contrast, the expression of activating receptors was less decreased in NK cells cultured with iPS-MSCs or embryonic MSCs. The expression of granzyme B protein (Figure 3C) and the production of IFN-γ were reduced in presence of IPS-MSCs, H9-MSCs, and BM-MSCs (Figure 3D). The same results were observed with 5 different iPS-MSCs. Our results suggest that iPS-MSCs can impair NK-cell proliferation and cytokine-induced activation of IL-2–activated NK cells in a similar way to that of embryonic MSCs and adult MSCs.
MSCs prevent NK-cell proliferation and activation. (A) NK cells were stimulated with IL-2 (250 U/mL) and cultured with IPS-MSCs or H9-MSCs for 4 days (NK/MSC ratio, 5:1). Results represent a representative experiment in which proliferation of CD56+/CD3− NK cells was evaluated using the CFSE dilution method (5μM for 5 minutes at 37°C). (B) Activating receptors expression on activated NK cells cultured with MSCs for 4 days. Gray profiles represent marker expression, whereas open bars represent the negative control. (C) Granzyme B expression was determined by Western blot using anti-granzyme B mAb. GAPDH was used as a loading control. Numbers below each panel represent the intensities of granzyme B adjusted to GAPDH levels. (D) Secretion of IFN-γ in IL-2–activated NK cells after coculture with MSCs for 4 days was evaluated by ELISA assay. Results are representative of 5 independent experiments and are shown as the means ± SD of triplicate samples.
MSCs prevent NK-cell proliferation and activation. (A) NK cells were stimulated with IL-2 (250 U/mL) and cultured with IPS-MSCs or H9-MSCs for 4 days (NK/MSC ratio, 5:1). Results represent a representative experiment in which proliferation of CD56+/CD3− NK cells was evaluated using the CFSE dilution method (5μM for 5 minutes at 37°C). (B) Activating receptors expression on activated NK cells cultured with MSCs for 4 days. Gray profiles represent marker expression, whereas open bars represent the negative control. (C) Granzyme B expression was determined by Western blot using anti-granzyme B mAb. GAPDH was used as a loading control. Numbers below each panel represent the intensities of granzyme B adjusted to GAPDH levels. (D) Secretion of IFN-γ in IL-2–activated NK cells after coculture with MSCs for 4 days was evaluated by ELISA assay. Results are representative of 5 independent experiments and are shown as the means ± SD of triplicate samples.
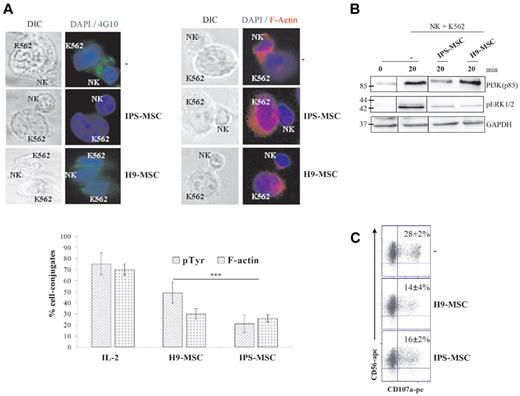
IPS-MSCs inhibit NKIS formation and cytolytic degranulation on NK cells
A NK-cell immunologic synapse (NKIS) is observed when NK cells interact with targets that express ligands for the NK receptors.27-29 To analyze NKIS and its function, we measured the presence of phospho-tyrosine at the NK/target K562 cell-line interface using the 4G10 antibody (Figure 4A). Fluorescence microscopy analysis showed polarization and accumulation of 4G10 in the contact area between NK and K562 cells, indicating that IL-2–activated NK cells can efficiently interact with K562 cells. In contrast, after 4 days of coculture with iPS-MSCs, the NK cells displayed an absence of the phospho-tyrosine polarization that leads to a strong decrease in NK-cell activity. However, H9-MSCs do not impair NKIS as strong as iPS-MSCs. During receptor engagement, one of the major downstream events is the phosphorylation of extracellular signal-regulated kinase (ERK), which leads to cytolytic degranulation.30-32 Direct interactions between NK and K562 cells strongly activated the ERK1/2 signaling pathway in NK cells, which was strongly down-regulated by the presence of IPS-MSCs or H9-MSCs (Figure 4B). The cytotoxic degranulation ability of NK cells was evaluated through expression of CD107a (lysosomal-associated membrane protein-1, LAMP-1), a functional marker that colocalizes with perforin in secretory lysosomes.24 CD107a degranulation was not detected in resting NK cells (data not shown). However, CD107a was strongly expressed at the cell surface by activated NK cells on contact with K562 target cells, which was then completely reduced by the presence of iPS-MSCs and H9-MSCs (Figure 4C). These results clearly demonstrate that iPS-MSCs down-regulate NK-cell functions, leading to general disruption of the secretory machinery on NK cells.
Inhibition of ERK prevents the ability of NK cells to form NKIS. (A) NKIS were visualized by fluorescence microscopy. Erythroleukaemia K562 cells were mixed with activated NK cells (ratio NK/K562, 2:1) and cultured for 20 minutes at 37°C on a poly-lysine–coated slide and stained with anti-phospho-tyrosine (4G10, green stain) and F-actin (red stain). Nuclei were stained with DAPI (blue stain). In the differential interference contrast micrograph (DIC) on the left (63×), a human NK cell is shown conjugated to a K562 cell and the synapse is indicated with an arrow. One representative experiment, of at least 3 independent ones, is shown. Signal intensity for 4G10 and F-actin was quantified with ImageJ software. (B) NK cells were cultured with K562 for 20 minutes at 37°C (ratio NK/K562, 2:1) and PI3K (p85) and pERK protein expression was evaluated by Western blot analysis. GAPDH was used as loading control. (C) Degranulation ability by NK cells cultured with IPS-MSCs or H9-MSCs for 4 days was evaluated using the CD107a assay. NK cells were stained with anti-CD56–APC and with anti-CD107a–PE and analyzed by flow cytometry. Monensin (10μM) was added to prevent the acidification of the endosomal compartment and the degradation of the granules secretion. The percentages listed represent the ratios of CD56+/CD107a+ cells. Results are representative of 4 independent experiments. Results are representative of 4 independent experiments and are shown as the means ± SD of triplicate samples.
Inhibition of ERK prevents the ability of NK cells to form NKIS. (A) NKIS were visualized by fluorescence microscopy. Erythroleukaemia K562 cells were mixed with activated NK cells (ratio NK/K562, 2:1) and cultured for 20 minutes at 37°C on a poly-lysine–coated slide and stained with anti-phospho-tyrosine (4G10, green stain) and F-actin (red stain). Nuclei were stained with DAPI (blue stain). In the differential interference contrast micrograph (DIC) on the left (63×), a human NK cell is shown conjugated to a K562 cell and the synapse is indicated with an arrow. One representative experiment, of at least 3 independent ones, is shown. Signal intensity for 4G10 and F-actin was quantified with ImageJ software. (B) NK cells were cultured with K562 for 20 minutes at 37°C (ratio NK/K562, 2:1) and PI3K (p85) and pERK protein expression was evaluated by Western blot analysis. GAPDH was used as loading control. (C) Degranulation ability by NK cells cultured with IPS-MSCs or H9-MSCs for 4 days was evaluated using the CD107a assay. NK cells were stained with anti-CD56–APC and with anti-CD107a–PE and analyzed by flow cytometry. Monensin (10μM) was added to prevent the acidification of the endosomal compartment and the degradation of the granules secretion. The percentages listed represent the ratios of CD56+/CD107a+ cells. Results are representative of 4 independent experiments. Results are representative of 4 independent experiments and are shown as the means ± SD of triplicate samples.
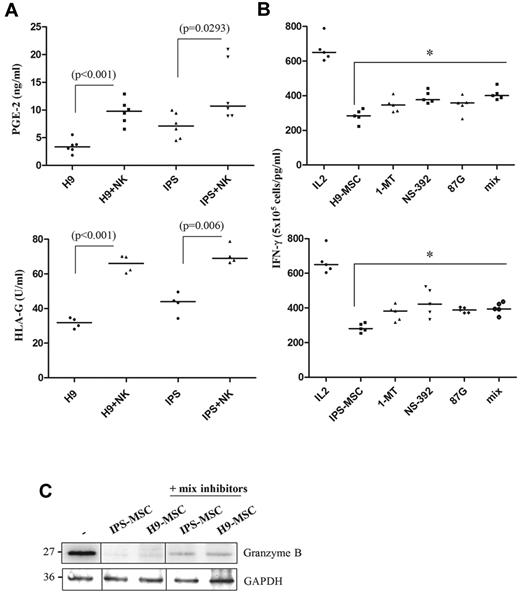
Role of soluble factors secreted by MSCs in NK-cell activation
Several soluble factors, such as HLA-G and prostaglandin E2 (PGE-2), and other factors, such as indolamine 2,3-dioxygenase (IDO), have been reported to be involved in the adult MSC-mediated inhibitory effect against NK cells.33,34 We observed a remarkable increase of soluble HLA-G and PGE-2 in the supernatants after the coculture between the different iPS-MSCs and NK cells (Figure 5A) in the same way than embryonic MSCs. The addition to the culture of single inhibitors specific to the IDO pathway (1-MT), HLA-G (87G), and PGE-2 (NS-398), only marginally counteracted (< 10%) the inhibitory effect exerted by the iPS-MSCs. Interestingly, the simultaneous impairment of the IDO, HLA-G, and PGE-2 pathway in H9-MSCs and IPS-MSCs, did not significantly restored the IFN-γ secretion (Figure 5B) and the granzyme B production (Figure 5C), emphasizing the fact these 3 factors are not sufficient to completely restore NK-cell activation.
Role of soluble factors secreted by MSCs in NK-cell activation. (A) Secretion of PGE-2 (ng/mL) and HLA-G (U/mL) by MSCs during the culture with NK cells was evaluated by ELISA assay. Results are representative of 5 independent experiments and are shown as the means ± SD of triplicate samples. Statistically significant differences between MSCs cultured or not with NK cells are indicated by asterisks (***P < .001; **P < .01). (B) Freshly isolated NK cells were stimulated for 4 days with IL-2 (250 U/mL) in the presence of MSCs. Inhibitors of IDO activity (1-MT, 1mM), PGE-2 secretion (NS-398, 5μM) and HLA-G neutralizing antibody (87G, 10μg/mL) were added at the start of the culture. Granzyme B expression was determined by Western blot using anti-granzyme B mAb. (C) Secretion of IFN-γ in IL-2–activated NK cells in presence of MSCs and soluble factors inhibitors was evaluated by ELISA assay. Results are representative of 5 independent experiments and are shown as the means ± SD of triplicate samples. Statistically significant differences between NK cells cultured with MSCs in presence or not with soluble inhibitors are indicated by asterisks (***P < .001; *P < .05).
Role of soluble factors secreted by MSCs in NK-cell activation. (A) Secretion of PGE-2 (ng/mL) and HLA-G (U/mL) by MSCs during the culture with NK cells was evaluated by ELISA assay. Results are representative of 5 independent experiments and are shown as the means ± SD of triplicate samples. Statistically significant differences between MSCs cultured or not with NK cells are indicated by asterisks (***P < .001; **P < .01). (B) Freshly isolated NK cells were stimulated for 4 days with IL-2 (250 U/mL) in the presence of MSCs. Inhibitors of IDO activity (1-MT, 1mM), PGE-2 secretion (NS-398, 5μM) and HLA-G neutralizing antibody (87G, 10μg/mL) were added at the start of the culture. Granzyme B expression was determined by Western blot using anti-granzyme B mAb. (C) Secretion of IFN-γ in IL-2–activated NK cells in presence of MSCs and soluble factors inhibitors was evaluated by ELISA assay. Results are representative of 5 independent experiments and are shown as the means ± SD of triplicate samples. Statistically significant differences between NK cells cultured with MSCs in presence or not with soluble inhibitors are indicated by asterisks (***P < .001; *P < .05).
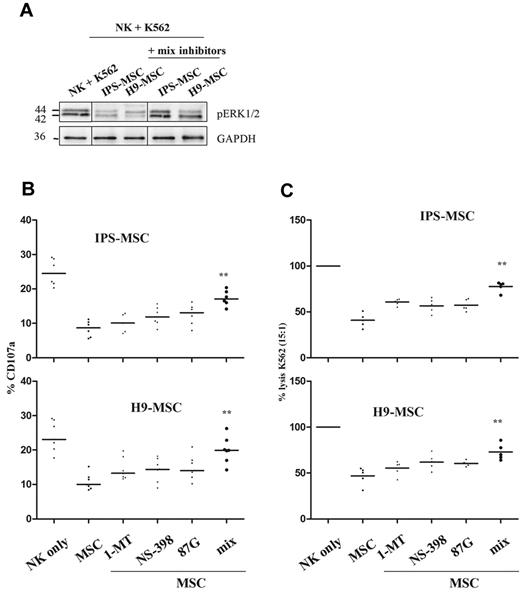
Role of soluble factors secreted by MSCs in NK-cell degranulation and cytotoxicity
Although IDO, PGE-2, and HLA-G were not found to restore NK activation, they were able to significantly reestablish not only the ERK signaling (Figure 6A), but the consequent degranulation ability (CD107a; Figure 6B) and cytotoxicity (Figure 6C) in activated NK cells, indicating a complex mechanism of immunosuppression activity by IPS-MSCs and H9-MSCs.
Role of soluble factors secreted by MSCs in NK-cell degranulation and cytotoxicity. (A) NK cells were cultured in presence of K562 target cells for 20 minutes (ratio NK/K562, 2:1). pERK protein expression was determined by Western blot analysis and GAPDH was used as a loading control. CD107a degranulation (B) and NK-cell cytotoxicity was evaluated using the 51Cr-release assay (C) after IPS-MSC or H9-MSC culture. Results are expressed as the percentage of K562 lysis in the presence of inhibitors of HLA-G, IDO and PGE-2. One hundred percent indicates NK cells alone. Bars represent the median obtained from 6 independent experiments. The NK/K562 ratio was 15:1 for the 51Cr-release assay and 5:1 for the CD107a assay. Statistically significant differences between MSCs in presence or not with soluble inhibitors are indicated by asterisks, **P < .01.
Role of soluble factors secreted by MSCs in NK-cell degranulation and cytotoxicity. (A) NK cells were cultured in presence of K562 target cells for 20 minutes (ratio NK/K562, 2:1). pERK protein expression was determined by Western blot analysis and GAPDH was used as a loading control. CD107a degranulation (B) and NK-cell cytotoxicity was evaluated using the 51Cr-release assay (C) after IPS-MSC or H9-MSC culture. Results are expressed as the percentage of K562 lysis in the presence of inhibitors of HLA-G, IDO and PGE-2. One hundred percent indicates NK cells alone. Bars represent the median obtained from 6 independent experiments. The NK/K562 ratio was 15:1 for the 51Cr-release assay and 5:1 for the CD107a assay. Statistically significant differences between MSCs in presence or not with soluble inhibitors are indicated by asterisks, **P < .01.
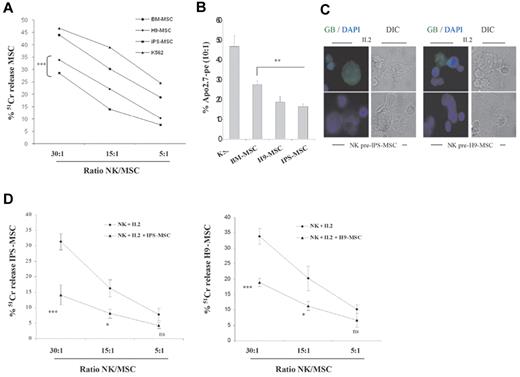
IPS-MSCs and H9-MSCs are less susceptible to NK cells than BM-MSCs
Previous studies have shown significant lysis of BM-MSCs26,35 and ES-MSCs36 by the cytotoxic immune effectors. We explored the susceptibility of iPS-MSCs to lysis by NK cells. NK cells were stimulated with IL-2 for 48 hours and used in cytotoxicity assays against iPS-MSCs, H9-MSCs, or BM-MSCs. Resting NK cells did not kill MSCs, regardless of their origin (data not shown). However, as shown by the 51Cr-release assay (Figure 7A) and the Apo2.7 assay (Figure 7B), activated NK cells displayed cytolytic activity in a ratio-dependent manner. ES-MSCs and iPS-MSCs are killed in vitro with a less efficiency than BM-MSCs and apparently more resistant to activated NK cells. Similar results were observed with the different iPS-MSCs (data not shown). Because iPS-MSCs and H9-MSCs inhibited NK-mediated K562 lysis, we investigated if MSCs could directly prevent their own death. As shown in Figure 7C (top panel), preactivated–IL-2 NK cells efficiently interacted with iPS-MSCs and H9-MSCs, as observed by the polarization of granzyme B granules in the NKIS (60%-70% for iPS-MSCs and 50%-60% for H9-MSCs). In contrast, NK cells cocultured with iPS-MSCs or ES-MSCs for 4 days in the presence of IL-2, although able to form conjugates with MSCs, did not induce granule polarization inside the synapse with MSCs (Figure 7C bottom panel). These results were confirmed by the 51Cr-release assay in which activated NK cells were able to kill iPS-MSCs and H9-MSCs, whereas activated NK cells precultured with MSCs did not (Figure 7D).
IPS-MSCs and H9-MSCs are more resistant to activated NK cytolysis than BM-MSCs. NK cells stimulated with IL-2 for 48 hours were cocultured with MSCs for 4 hours. Activated NK cells were tested in a 4-hour 51Cr-release assay against H9-MSCs (♦), IPS-MSCs (■) or BM-MSCs (●) at different NK/MSC ratios (A). (B) MSCs were cultured for 4 hours with activated NK cells (ratio NK/MSC, 10:1) and then stained with an anti-Apo2.7–PE for 30 minutes at 4°C to evaluate their apoptosis. All experiments were done in triplicate. K562 cells (▴) were used as a positive control for NK cells. The interaction between NK cells and MSCs was visualized by fluorescence microscopy. (C) IPS-MSCs or H9-MSCs were mixed with activated (IL-2) or MSC-cultured NK cells (preIPS-MSCs or preH9-MSCs; ratio 2:1) and cultured for 20 minutes at 37°C on a poly-lysine–coated slide. Granule polarization, as defined by the accumulation of granzyme B (green) staining in the contact area between NK cells and MSC, after 30 minutes of coculture, was analyzed by fluorescence microscopy using a specific mAb. Nuclei were stained with DAPI (blue stain). In the differential interference contrast micrograph (DIC), on the left (63×), a human NK cell is shown conjugated to a MSC. One representative experiment, of at least 4 independent experiments, is shown. (D) NK cells were tested in a 4-hour 51Cr-release assay against IPS-MSCs or H9-MSCs at different E/T ratios. The panels show IL-2–activated NK cells against IPS-MSCs or H9-MSCs. Pretreatment with IPS-MSCs or H9-MSCs strongly decreased the killing potential of NK cells. Results are representative of 5 independent experiments and are shown as the means ± SD of triplicate samples. Statistically significant differences between NK cells cultured with or with MSCs are indicated by asterisks (***P < .001; **P < .01).
IPS-MSCs and H9-MSCs are more resistant to activated NK cytolysis than BM-MSCs. NK cells stimulated with IL-2 for 48 hours were cocultured with MSCs for 4 hours. Activated NK cells were tested in a 4-hour 51Cr-release assay against H9-MSCs (♦), IPS-MSCs (■) or BM-MSCs (●) at different NK/MSC ratios (A). (B) MSCs were cultured for 4 hours with activated NK cells (ratio NK/MSC, 10:1) and then stained with an anti-Apo2.7–PE for 30 minutes at 4°C to evaluate their apoptosis. All experiments were done in triplicate. K562 cells (▴) were used as a positive control for NK cells. The interaction between NK cells and MSCs was visualized by fluorescence microscopy. (C) IPS-MSCs or H9-MSCs were mixed with activated (IL-2) or MSC-cultured NK cells (preIPS-MSCs or preH9-MSCs; ratio 2:1) and cultured for 20 minutes at 37°C on a poly-lysine–coated slide. Granule polarization, as defined by the accumulation of granzyme B (green) staining in the contact area between NK cells and MSC, after 30 minutes of coculture, was analyzed by fluorescence microscopy using a specific mAb. Nuclei were stained with DAPI (blue stain). In the differential interference contrast micrograph (DIC), on the left (63×), a human NK cell is shown conjugated to a MSC. One representative experiment, of at least 4 independent experiments, is shown. (D) NK cells were tested in a 4-hour 51Cr-release assay against IPS-MSCs or H9-MSCs at different E/T ratios. The panels show IL-2–activated NK cells against IPS-MSCs or H9-MSCs. Pretreatment with IPS-MSCs or H9-MSCs strongly decreased the killing potential of NK cells. Results are representative of 5 independent experiments and are shown as the means ± SD of triplicate samples. Statistically significant differences between NK cells cultured with or with MSCs are indicated by asterisks (***P < .001; **P < .01).
Discussion
Because of their immunoregulatory properties adult MSCs have been placed in first line for the GVHD treatment and in organ transplantation.37-40 During allogeneic transplantation, such as bone marrow41 and organ transplantation,42 NK cells play an important role. NK cells are specialized lymphocytes that kill target cells without prior activation.43 In addition, they play a critical role in the surveillance of tumors, virus-infected cells and allogeneic cells.44-46 By impairing NK functions, MSCs protect against GVHD and may delay graft rejection. MSCs, and mainly BM-MSCs, have been used to treat resistant GVHD and to prevent acute rejection in organ transplantation.38-40 However, it should be stated that, although BM-MSCs can efficiently prevent GvDH, they can only delay allograft rejection as these cells cannot assure long-lasting immunoregulatory function in vitro and in vivo.2 Indeed, successive passages slow the proliferation rate, and MSCs progressively show loss of multipotentiality and lack immunosuppressive activity. The interest of identifying new sources of MSCs relates to obtain more primitive MSCs with a higher proliferation rate. Embryonic MSCs represent an alternative to the use of classic BM-MSCs as they display immunoregulatory properties.8-10,47 IPSC arising from reprogrammed adult somatic cells represent an interesting alternative to ES cells but the immunosuppression activity of iPS-derived MSCs remains to be explored and compared with embryonic-derived MSCs and adult MSCs. Our results indicate that iPS-derived MSCs display a strong immunosuppressive properties on NK cells with a long-lasting effect in successive passages similarly to ES-derived MSCs, by interfering in the NK activation process and, therefore, efficiently protecting target cells from being killed by NK cells.
We have developed an original model of human iPS based on reprogramming differentiated human embryonic MSCs, which has allowed a comparison between IPS-MSCs and their parental embryonic counterpart, ES-MSCs. We have confirmed that the transduced transgenes, Nanog, Lin-28, Sox-2, and Oct3/4, were completely silenced in iPS as expected48 and were not reexpressed after differentiation toward the MSC lineage. IPS-MSCs expressed a similar phenotype to their parental ES-MSCs and have similar immunoregulatory functions.
We demonstrate that iPS-MSCs modulate NK-cell responses and clearly affect several NK-cell primordial functions (direct cytolysis of target cells and production of IFN-γ), involving at least HLA-G, prostaglandin E2 (PGE-2), and indolamine 2,3-dioxygenase (IDO). We have shown that IPS-MSCs are similar to ES-MSCs and inhibit efficiently NK-cell cytolytic activity as well as BM-MSCs, can strongly down-regulate IL-2–induced proliferation of NK cells, the expression of natural cytotoxic receptors (NCR) and IFN-γ production, This is principally because of the fact that, in both IPS-MSCs and H9-MSCs, prevention of the ERK signaling pathway enables NK cells to form immunologic synapses with target cells inhibiting at the same time polarization of cytolytic granules to the immunologic synapse. We did not observe any functional variability between MSCs derived from distinct human iPSC. Interestingly, the immune function of iPS-MSCs and ES-MSCs is maintained during multiple passages without any senescence in contrast to BM-MSCs (10 passages vs 3 passages for the BM-MSCs). The transient inhibitory effect of BM-MSCs may be related to the time-limited production of immunoregulatory factors and the identification of potential soluble factors from iPS-MSCs that efficiently inhibit NK cells will offer the opportunity to increase and promote the functions of adult MSCs. Therefore, detailed analysis of immune cell interaction with MSCs is important, and should provide the basis for designing novel strategies to increase the viability and function of MSCs in different tissue engineering applications. In agreement with previous studies we also show in this report that NK cells can target and significantly kill MSCs. Indeed, compared with K562 lysis, NK cells can mediate significant lysis of BM-MSCs. Moreover, we demonstrate that iPS-MSCs and ES-MSCs are also direct targets of NK-cell mediated killing, but appear to be more resistant to being killed by preactivated NK cells. Our study reported for the first time that iPS-MSCs and ES-MSCs could directly prevent their own death by an unknown mechanism.
In conclusion, studies reported in this work provide evidence for immune regulatory function of iPS-derived MSCs that could be explained by the secretion of tolerogenic factors. IPS-MSCs could provide an immeasurable source of autologous cells that can be prepared from individual patients to different therapies. Nevertheless, the fact the iPS-MSCs contain a transgene whose site of integration cannot be predicted, limit for the moment the preclinical and clinical use of this kind of cells. The recent development of methodologies for inducing IPS without the use of lentiviral vectors will render iPS-MSCs an attractive candidate for biotherapies.49-52 Transcriptomic, epigenetic, and proteomic comparative studies will be helpful to identify novel and putative secreted immunosuppressive factors to either promote adult MSC functions or replace MSCs as alternative and perspective approaches.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by grants from the Association Nouvelles Recherches Biomédicales (ANRB), DIM STEM POLE, Région Ile de France (MEDICEN IngeCell programm), the Université Paris Sud-11, and Institut Francilien de Recherche en Nephrologie et Transplantation (IFRNT). This work was also supported in part by grants from the Association pour la Recherche sur le Cancer (ARC; no. 3272), Ligue contre le Cancer, as well as the Institut National du Cancer (INCA), ARC/INCA, and Agence Nationale de la Recherche.
Authorship
Contribution: M.G. and N.O. designed and performed experiments, analyzed data, and wrote the manuscript; Z.M.N. and A.V. performed experiments, analyzed data, and edited the manuscript; and S.C., B.A., A.D., and A.B.G. designed research, analyzed and interpreted data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Pr Annelise Bennaceur Griscelli, UMR 935, Paul Brousse Hospital, Villejuif, France; e-mail: annelise.bennaceur@pbr.aphp.fr
References
Author notes
M.G. and N.O. contributed equally to this article.