In this issue of Blood, Ju and colleagues report that a selective inhibitor of Janus kinase 3 (Jak3) blocks autocrine and paracrine interleukin 2 (IL-2), IL-9, and IL-15 activation, which is important for lymphocyte proliferation induced by human T-cell leukemia virus (HTLV).1
DNA sequence analysis predicts 90 protein tyrosine kinases encoded by the human genome, including 32 nonreceptor kinases.2 One group of nonreceptor kinases are the Janus family kinases: Jak1, Jak2, Jak3, and Tyk2. Whereas, Jak1, Jak2, and Tyk2 are constitutively expressed in mammalian cells, Jak3 is primarily restricted to hematopoietic cells. Hematopoietic cytokines and growth factors use members of the Jak family for signal transduction, and Jaks are important for cell proliferation, survival, development, and differentiation. Loss of Jak function results in immune deficiency, such as a form of severe combined immune deficiency syndrome associated with loss of Jak3. In contrast, activating mutations in Jaks cause malignant transformation.
HTLV type 1 (HTLV-1) is the etiologic agent of adult T-cell leukemia lymphoma (ATLL) and tropical spastic paraparesis (TSP), also termed HTLV-1–associated myelopathy (HAM).3 The transcriptional activator protein, Tax, promotes virus replication by up-regulating transcriptional activity of CREB/ATF proteins. Tax, which suppresses apoptosis through constitutive activation of the NFκB pathway, is also sufficient for immortalization of CD4+ lymphocytes. Tax also exhibits posttranscriptional effects through inhibition of cell-cycle phase inhibitors, DNA repair factors, DNA damage responses, and chromosome instability checkpoint proteins. Despite its role in initiating transformation, Tax expression is diminished or absent after ATLL is established, and such immortalized cells frequently exhibit growth factor independence.
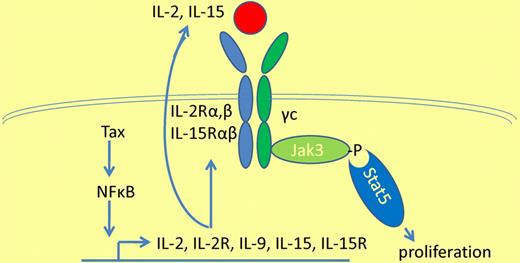
The Jak-Stat pathway is constitutively activated in HTLV-1–transformed cells.4 This may occur through constitutive autocrine stimulation of IL-2, IL-15, and IL-2 and IL-15 receptor expression, as a result of Tax-induced NFκB expression (see figure).5 Alternatively, paracrine stimulation of IL-9 by HTLV-1 Tax could also promote activation of the IL-9 receptor on monocytes, which in turn stimulates proliferation of HTLV-1–infected lymphocytes.6 The current article by Ju and colleagues demonstrates that inhibition of all 3 receptor-mediated pathways prevents proliferation of HTLV-1–infected lymphocytes more effectively than inhibition of any one of the pathways.1 Moreover, because the IL-2, IL-9, and IL-15 receptors all share the use of the common γ chain (γc), inhibition of γc-associated Jak3 proved to be as effective as combined inhibition of all 3 pathways. CP690 550 is a selective Jak3 inhibitor, plus it also inhibits mutant forms of Jak2.2 Clinical studies are under way in patients with rheumatoid arthritis and psoriasis; other studies will also examine the prevention of renal transplant rejection.
Constitutive Jak-Stat signaling in HTLV-1 infection resulting in overexpression of interleukins 2, 9, and 15, interleukin receptors 2 and 15, and activation of Jak3 and Stat5, resulting in lymphocyte proliferation.
Constitutive Jak-Stat signaling in HTLV-1 infection resulting in overexpression of interleukins 2, 9, and 15, interleukin receptors 2 and 15, and activation of Jak3 and Stat5, resulting in lymphocyte proliferation.
The Jak-Stat pathway may also be constitutively activated in transformed cells due to gain-of-function mutations. Although Jak2 mutations are common in myeloproliferative disorders, Jak3 mutations have been reported in only a few patients with solid tumors, and have not been identified in ATLL.2,7 Alternatively, the Jak-Stat pathway may be activated by loss of suppressor of cytokine signaling (SOCS) proteins, E3 ubiquitin ligases that promote the degradation of Jak proteins. HTLV-1 infection overcomes the effects of interferon-induced Jak-Stat activation by up-regulation of SOCS1.8
In light of the limited efficacy of current therapies for ATLL and HAM/TSP, the current preclinical results with Jak3–targeted therapy offer a potential new avenue of treatment for these disorders.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal