Disseminated intravascular coagulation in sepsis is associated with microvascular thrombosis and organ dysfunction. It was expected that prothrombotic disposition such as factor V Leiden (FVL) mutation would worsen clinical outcome. Astonishingly, clinical trial and animal experimental data indicate that FVL can be associated with improved survival. This study investigated the effect of FVL on the response to endotoxin of the coagulation and fibrinolytic system in humans. Fourteen healthy male subjects without FVL and 15 healthy males with heterozygous FVL received an intravenous bolus dose of endotoxin, 2 ng/kg of body weight. Blood samples were drawn before and 1, 2, 4, 6, and 24 hours after administration of the endotoxin. Injection of endotoxin led to a more pronounced increase in soluble fibrin in patients with FVL than in controls. Patients with FVL displayed a more sustained increase in plasmin-plasmin inhibitor complex after 4, 6, and 24 hours. Patients with FVL mutation also displayed higher levels of D-dimer and fibrinogen-fibrin degradation products in plasma after 24 hours. Patients with FVL generate higher levels of soluble fibrin, which may serve as cofactor in tissue plasminogen activator–induced plasminogen activation, leading to a more sustained activation of fibrinolysis with production of more fibrinogen- and fibrin-degradation products.
Introduction
Replacement of Arg506 with Gln in coagulation factor V (the factor V Leiden [FVL] mutation)1 results in the loss of an important cleavage site for activated protein C (aPC). Factor Va carrying the FVL mutation is less sensitive to inactivation by aPC. In addition, FVL may display an impaired cofactor function in the degradation of factor VIIIa by aPC. FVL predisposes for the development of venous thrombosis.2 The high prevalence of FVL in the European population3 indicates some survival advantage, which might be related to less blood loss on injury or childbirth or to improved wound healing.4 This may be a consequence of enhanced fibrin formation due to the impaired inactivation of factor Va.
Presence of disseminated intravascular coagulation (DIC) in sepsis is associated with an adverse outcome.5 DIC may lead to microvascular thrombosis, causing multiple organ dysfunctions, and it is conceivable that a prothrombotic disposition such as FVL would be associated with an increased rate of fibrin disposition, causing organ dysfunction and death in sepsis.
Astonishingly, data from the Recombinant Human Activated Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) and Extended Evaluation of Recombinant Human Activated Protein C in Severe Sepsis (ENHANCE) trials indicate that the FVL mutation might be associated with improved survival in severe sepsis.6,7 In the PROWESS trial, mortality of patients with severe sepsis with heterozygous FVL was 15.6%, compared with 31.0% in patients without FVL in the patient group not treated with recombinant aPC (Drotrecogin alfa [activated]). In patients treated with Drotrecogin alfa (activated), the difference was smaller, with a mortality of 20.3% in heterozygous FVL carriers and 24.9% in patients without FVL.
Kondaveeti et al8 determined FVL status in 259 children with meningococcal disease. Mortality was similar in patients with and without heterozygous FVL, but patients with FVL had an increased rate of surgical skin grafting, referral to plastic surgeon, and/or amputation.8 In a population-based study, Benfield et al9 did not find a survival benefit related to the presence of FVL in sepsis, but the investigators combined patients with heterozygous and with homozygous FVL and did not account for disease severity.9 Thus, apart from the PROWESS and ENHANCE study data, there is little evidence from clinical trials for or against a beneficial effect of the FVL mutation in severe sepsis.
Kerlin et al7 compared the survival of wild-type and transgenic heterozygous and homozygous FVL mice after intraperitoneal injection of endotoxin and found a significantly improved survival in heterozygous FVL mice compared with wild-type mice as well as homozygous FVL mice. However, experiments by Brüggemann et al,10 using transgenic FVL mice receiving intraperitoneal injections of Escherichia coli bacteria in contrast, did not show any beneficial effect of the FVL mutation.
The present experimental study does not focus on clinical outcome but on the mechanisms of action of FVL in the context of endotoxemia. Although endotoxemia models may differ substantially from actual bacterial sepsis, they may be used to gain information about the pathophysiology of inflammatory conditions. We used an established human endotoxemia model in healthy males with heterozygous FVL and in a control group consisting of healthy males without FVL. One advantage of this model compared with a mouse model is that a full array of hemostasis assays, including various assays for fibrin derivatives, can be used. Most activation marker assays do not function properly in a mouse model because the assays are based on murine monoclonal antibodies directed against human antigens, which show little reactivity with the corresponding murine antigens. In addition, there might be species differences in the response of the coagulation system to endotoxin. The present data might be helpful for the interpretation of the clinical results for patients with FVL and for the planning of future clinical trials involving laboratory markers for coagulation and fibrinolysis activation.
Methods
The local ethical committee of the University Medical Center Mannheim approved all procedures. After written informed consent was obtained in accordance with the Declaration of Helsinki, 14 healthy male subjects without FVL or other known thrombophilic disorder, 27 to 51 years of age, and 15 healthy males with heterozygous FVL, 20 to 69 years of age, were included in the trial. The participants had not been treated with anticoagulant or antiplatelet drugs for at least 2 months before inclusion in the trial.
The human endotoxemia model described in detail by Pernestorfer et al11 was used. After overnight fasting, an infusion of 5% glucose was started and continued for 8.5 hours at 3 mL/kg of body weight per hour. Parallel to the start of infusion, patients received 500 to 1000 mg of paracetamol to alleviate symptoms such as headache and fever induced by endotoxin administration.12 After 30 minutes, venous blood samples were drawn, and patients received an intravenous bolus dose of endotoxin, 2 ng/kg of body weight (National Reference Endotoxin, E coli; The United States Pharmacopoial Convention Inc). Further venous blood samples were drawn 1, 2, 4, 6, and 24 hours after administration of the endotoxin.
Citrated blood was centrifuged at 2000g for 20 minutes, and plasma was harvested and transferred to polypropylene sample tubes. Serum tubes were stored at room temperature for 60 minutes, then centrifuged at 2000g for 20 minutes, and aliquots of serum were transferred to polypropylene sample tubes.
The plasma and serum aliquots were frozen in liquid nitrogen and stored at −70°C until analysis. The laboratory analyses were performed in batches to minimize analytical bias. For analysis, samples were thawed in a water bath at 37°C for 10 minutes and then centrifuged at 10 000g for 5 minutes.
Fibrinogen (functional assay according to Clauss13 ) was measured with the use of reagents and equipment from DadeBehring Diagnostics.
Photometric immunoassays with the use of antibody-coated latex particles were also performed on a Hitachi 904 autoanalyzer. The TINAquant D-dimer assay was from Roche Diagnostics. The Iatron SF assay for soluble fibrin,14 and the assay for fibrinogen and fibrin degradation products in plasma (FDP-P) was from Iatron Laboratories. The Sekusui SF assay for measurement of soluble fibrin15 was from Daiichi Pure Chemicals and was also performed on the Hitachi 904 autoanalyzer, in parallel with the other assays. Plasmin-plasmin inhibitor complexes (PPICs; plasmin-antiplasmin) were measured with the use of a 96-well microtiter plate enzyme-linked immunoabsorbent assay from DRG Instruments GmbH.
Data analysis
To minimize the effect of outliers and distribution effects in view of the small number of patients, medians and interquartile ranges were used rather than mean values and standard deviations. All group comparisons were performed with the use of Wilcoxon signed rank sum test. For correlation graphs, coefficients of correlation R were calculated, using a linear correlation model.
Results
Effect of FVL on the procoagulant and profibrinolytic response to endotoxin
Activation of the coagulation system in response to endotoxin, as well as other stimuli, leads to the formation of fibrin. Depending on the location, mechanism, and intensity of coagulation activation, part of the fibrin is not incorporated into clots, but appears in blood samples as “soluble fibrin.” This soluble fibrin can be detected by laboratory assays based on monoclonal antibodies against neo-epitopes generated directly or indirectly by the action of thrombin on fibrinogen. For the present study, we used 2 soluble fibrin assays based on different monoclonal antibodies, but both used similar immunoassay technologies.
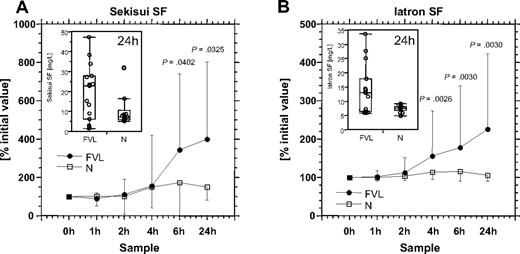
As shown in Table 1, the baseline results of the Sekisui SF assay were similar in patients with and without FVL. The Iatron SF assay showed a lower median value in patients with FVL than in controls. Injection of endotoxin led to considerably more pronounced increase in soluble fibrin in patients with FVL than in controls (Figure 1).
Baseline levels of coagulation parameters in FVL patients and controls
| . | Baseline values (mean ± IQR, range) . | P . | |
|---|---|---|---|
| FVL . | Controls . | ||
| Fibrinogen Clauss, g/L | 2.70 ± 0.70 (2.10-4.30) | 2.50 ± 0.68 (2.10-3.90) | .430 |
| Sekisui SF, mg/L | 5.40 ± 4.18 (0.70-10.60) | 5.10 ± 4.50 (2.80-28.20) | .948 |
| Iatron SF, mg/L | 5.80 ± 1.38 (5.00-9.40) | 7.25 ± 1.20 (4.20-9.00) | .038 |
| TINAquant D-dimer, mg/L | 0.31 ± 0.28 (0.04-1.14) | 0.10 ± 0.08 (0.02-0.24) | .014 |
| Iatron FDP-P, mg/L | 3.20 ± 1.05 (2.40-4.70) | 2.20 ± 0.50 (1.60-3.00) | < .001 |
| PPIC, μg/L | 230.2 ± 99.4 (172.7-476.3) | 194.2 ± 79.2 (152.5-336.3) | .064 |
| TINAquant D-dimer (Serum), mg/L | 0.25 ± 0.22 (0.07-0.95) | 0.10 ± 0.12 (0.00-0.19) | .001 |
| . | Baseline values (mean ± IQR, range) . | P . | |
|---|---|---|---|
| FVL . | Controls . | ||
| Fibrinogen Clauss, g/L | 2.70 ± 0.70 (2.10-4.30) | 2.50 ± 0.68 (2.10-3.90) | .430 |
| Sekisui SF, mg/L | 5.40 ± 4.18 (0.70-10.60) | 5.10 ± 4.50 (2.80-28.20) | .948 |
| Iatron SF, mg/L | 5.80 ± 1.38 (5.00-9.40) | 7.25 ± 1.20 (4.20-9.00) | .038 |
| TINAquant D-dimer, mg/L | 0.31 ± 0.28 (0.04-1.14) | 0.10 ± 0.08 (0.02-0.24) | .014 |
| Iatron FDP-P, mg/L | 3.20 ± 1.05 (2.40-4.70) | 2.20 ± 0.50 (1.60-3.00) | < .001 |
| PPIC, μg/L | 230.2 ± 99.4 (172.7-476.3) | 194.2 ± 79.2 (152.5-336.3) | .064 |
| TINAquant D-dimer (Serum), mg/L | 0.25 ± 0.22 (0.07-0.95) | 0.10 ± 0.12 (0.00-0.19) | .001 |
Soluble fibrin levels before and 1, 2, 4, 6, and 24 hours after administration of the endotoxin. Results are shown as medians and interquartile ranges for patients with FVL (●) and controls (□). Patients with FVL display a higher level of soluble fibrin after endotoxin infusion. Inserts show the distribution of the 24-hour values for patients with FVL and controls (N).
Soluble fibrin levels before and 1, 2, 4, 6, and 24 hours after administration of the endotoxin. Results are shown as medians and interquartile ranges for patients with FVL (●) and controls (□). Patients with FVL display a higher level of soluble fibrin after endotoxin infusion. Inserts show the distribution of the 24-hour values for patients with FVL and controls (N).
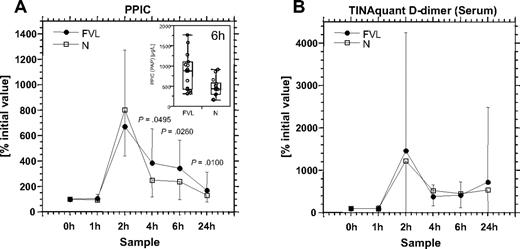
Endotoxemia causes enhanced release of tissue plasminogen activator (tPA) from the endothelium, and soluble fibrin serves as cofactor in tPA-induced plasminogen activation. Plasmin is inactivated by formation of a covalent complex with α2-plasmin inhibitor. This PPIC may serve as an indicator for in vivo activation of fibrinolysis. Baseline PPIC levels did not differ significantly between patients with FVL and controls (Table 1). Endotoxin injection caused a strong increase in PPIC with a maximum 2 hours after the injection (Figure 2A). The maximum values were similar in both groups, but patients with FVL mutation displayed a more sustained increase in PPIC at 4, 6, and 24 hours after endotoxin injection.
PPIC and serum D-dimer levels before and 1, 2, 4, 6, and 24 hours after administration of the endotoxin. Results are shown as medians and interquartile ranges for patients with FVL (●) and controls (□). Patients with FVL display a more sustained generation of PPIC after endotoxin infusion. Highest levels of D-dimer in serum are observed 2 hours after endotoxin infusion. Inserts in panel A show the distribution of the 6-hour values for patients with FVL and controls (N).
PPIC and serum D-dimer levels before and 1, 2, 4, 6, and 24 hours after administration of the endotoxin. Results are shown as medians and interquartile ranges for patients with FVL (●) and controls (□). Patients with FVL display a more sustained generation of PPIC after endotoxin infusion. Highest levels of D-dimer in serum are observed 2 hours after endotoxin infusion. Inserts in panel A show the distribution of the 6-hour values for patients with FVL and controls (N).
TINAquant D-dimer is specific for plasmin-modified crosslinked fibrin derivatives. Baseline values of TINAquant D-dimer were higher for patients with FVL both in plasma and in serum, indicating enhanced baseline generation of crosslinked fibrin degradation products in patients with FVL (Table 1). Initial serum levels of D-dimer antigen were slightly lower than plasma levels.
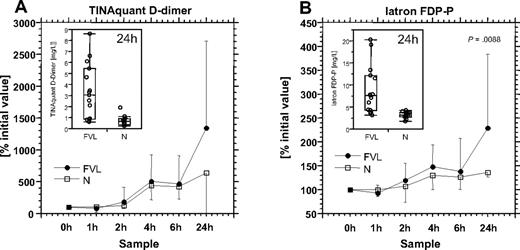
D-dimer antigen measured with the TINAquant D-dimer assay in plasma and serum differed in kinetics. Endotoxin injection led to an increase in D-dimer antigen levels both in serum (Figure 2B) and plasma (Figure 3A), but the highest levels in serum were found after 2 hours, whereas in plasma, the maximum levels were found after 24 hours. The course of D-dimer antigen in serum resembles the course of PPIC. No significant differences were observed between patients with FVL and controls in serum D-dimer antigen levels.
TINAquant D-dimer and Iatron FDP-P levels before and 1, 2, 4, 6, and 24 hours after administration of the endotoxin. Results are shown as medians and interquartile ranges for patients with FVL (●) and controls (□). Patients with FVL display higher levels of D-dimer and FDP-P 24 hours after endotoxin injection. Inserts show the distribution of the 24-hour values for patients with FVL and controls (N).
TINAquant D-dimer and Iatron FDP-P levels before and 1, 2, 4, 6, and 24 hours after administration of the endotoxin. Results are shown as medians and interquartile ranges for patients with FVL (●) and controls (□). Patients with FVL display higher levels of D-dimer and FDP-P 24 hours after endotoxin injection. Inserts show the distribution of the 24-hour values for patients with FVL and controls (N).
Baseline levels of FDP-P were significantly higher in patients with FVL than in controls (Table 1). This indicates that persons with FVL have an increased activation of fibrinolysis. FDP-P levels increased in response to endotoxin injection, and the kinetics were similar to TINAquant D-dimer measured in plasma, with the highest values present after 24 hours (Figure 3B). Patients with FVL displayed higher levels of FDP-P and D-dimer 24 hours after endotoxin injection, and the difference was statistically significant for FDP-P (P < .009).
Discussion
Endotoxin injection caused a higher level of soluble fibrin and a more sustained activation of fibrinolysis in patients with FVL than in controls without FVL.
Soluble fibrin supports tPA-induced plasminogen activation.16,17 A good example for this effect is the injection of thrombin-like snake venom enzymes such as ancrod, which induce massive intravascular fibrin formation.18 The plasminogen activation in response to ancrod injection occurs without changes in tPA or plasminogen activator inhibitor 1 (PAI-1) levels and is caused primarily by the cofactor effect of fibrin on tPA-induced plasminogen activation.19
Injection of endotoxin similarly causes formation of large amounts of plasmin, with a maximum PPIC concentration after 2 hours.20 In contrast to ancrod, endotoxin also stimulates tPA release from the endothelium.20,21 The profibrinolytic response is subsequently terminated by increasing levels of PAI-1,20,21 resulting in a rapid drop in PPIC concentration.
The present results indicate that this drop in PPIC is less pronounced in patients with FVL. This may be a consequence of the increased amount of soluble fibrin acting as cofactor in tPA-induced plasminogen activation and possibly shielding tPA from inactivation by PAI-1. Pernerstorfer at al20 showed that maximal thrombin generation occurs 4 to 6 hours after endotoxin infusion. Levels of prothrombin fragment F1.2 and thrombin-antithrombin complexes, as well as soluble fibrin, return to baseline within 24 hours.20 In patients with FVL, thrombin formation and formation of soluble fibrin follow different kinetics, with elevated levels also after 24 hours.
Enhanced fibrinolysis is a central defense mechanism against organ dysfunction in sepsis-induced DIC.22 Inhibition of fibrinolysis by treatment with antifibrinolytic agents in this condition promotes microvascular thrombosis, resulting in organ failure.23 In survivors of severe sepsis, markers of coagulation and fibrinolytic activation correlate, whereas in nonsurvivors coagulation activation is not balanced by activation of fibrinolysis.22 In animal experiments, homozygous FVL provides no survival benefit in endotoxemia.7 A possible explanation is that homozygous FVL exaggerates fibrin formation to a level that is above the threshold for effective clearance.
Elevated levels of PAI-1,24 as well as activated thrombin-activated fibrinolysis inhibitor (TAFIa),25 are frequent findings in patients with severe meningococcal sepsis. Meningococcal sepsis can be associated with tissue necrosis caused by widespread microvascular occlusion, a condition termed sepsis-induced purpura fulminans.26 As mentioned earlier, children with meningococcal infection and FVL had an increased rate of surgical skin grafting, referral to plastic surgeon, and/or amputation,8 indicating that the enhanced fibrin formation caused by FVL in conjunction with high PAI-1 and TAFIa promotes microvascular occlusion rather than preventing it.
A possible beneficial effect of FVL in sepsis would probably disappear if fibrinolysis is suppressed by massively elevated PAI-1 levels, if strongly elevated levels of the TAFIa prevent binding of plasminogen and tPA to the fibrin, or if massive coagulation activation leads to formation of more fibrin than can be cleared by the fibrinolytic system.
In conclusion, FVL induces an enhanced fibrinolytic response to endotoxin injection, presumably caused by higher levels of soluble fibrin acting as cofactor in tPA-induced plasminogen activation. “Latent coagulation”27 with presence of soluble fibrin complexes in the circulation might serve as a defense mechanism, leading to increased plasminogen activation, clearance of fibrin deposits, reduction of fibrinogen levels, and generation of fibrinogen degradation products acting as “endogenous anticoagulants.”
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank the medical technicians of the laboratory, Anja Kirchner, Natascha Heim, and Cornelia Kehl, for excellent laboratory work.
This work was supported by Heinrich Vetter Stiftung, Mannheim.
Authorship
Contribution: E.E. and N.S. were responsible for the human endotoxemia model experiments; B.J. contributed the experimental details for the endotoxemia model; the experimental approach and results were thoroughly discussed with H.W., who had performed similar experiments in mice; M.B. reviewed the manuscript; and C.-E.D. developed the experimental design for the study, supervised the endotoxemia model experiments, performed the laboratory analyses, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Carl-Erik Dempfle, University Hospital of Mannheim, I Department of Medicine, Theodor Kutzer Ufer 1-3, D-68167 Mannheim, Germany; e-mail: carl-erik.dempfle@umm.de.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal