The Jak2V617F mutation is found in most classical BCR/ABL-negative myeloproliferative neoplasms (MPNs). Usually, heterozygosity of the mutation is associated with essential thrombocythemia (ET) and homozygosity with polycythemia vera (PV). Retrovirally transduced or transgenic animal models have shown that the mutation is sufficient for MPN development but that the level of expression is crucial for MPN phenotypes. Therefore we investigated the effect of an endogenous heterozygous expression of Jak2V617F in knock-in (KI) mice. These animals displayed constitutive JAK2 activation and autonomous erythroid progenitor cell growth. Mice suffered from marked polycythemia, granulocytosis and thrombocytosis. Spleens and marrows displayed myeloid trilineage hyperplasia. Most animals survived to develop advanced fibrosis in these organs at around 9 months of age. In conclusion, constitutive heterozygous expression of JAK2V617F in mice is not embryo-lethal but results in severe PV-like disease with secondary myelofibrosis and not in ET-like disease as expected from patient study.
Introduction
The acquired Jak2V617F mutation is present in 95% of polycythemia vera (PV) patients and approximately 50% of patients suffering from essential thrombocythemia (ET) or primary myelofibrosis (PMF).1,–3 Interestingly, heterozygosity of the Jak2V617F mutation is usually associated with ET and homozygosity, resulting from mitotic recombination, with PV.4 Animal models using JAK2V617F retrovirally (RV)–transduced bone marrow (BM) cells5,,–8 or transgenesis (TG)9,10 have shown that JAK2V617F expression in hematopoietic stem cells (HSC) is sufficient to induce myeloproliferative neoplasms (MPNs) in mice. As suggested by patient studies, animals develop either an ET- or a PV-like disease depending on the JAK2V617F expression levels.6,9 Therefore, considering the crucial role of JAK2V617F expression level in disease development, we generated a knock-in (KI) model allowing for a physiologic expression of JAK2V617F from the endogenous Jak2 promoter to further our understanding of MPN physiopathology and JAK2V617F mechanism of action. We report here the phenotype of these mice.
Methods
Establishment of the Jak2V617F KI mouse line
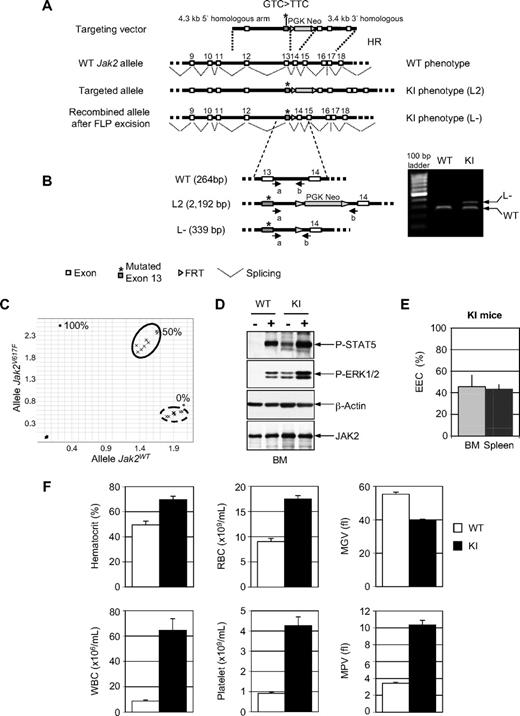
Jak2V617F KI animals were generated at the Mouse Clinical Institute, Illkirch, France (http://www-mci.u-strasbg.fr). All animal experiments were carried out at the Animal Facilities of the Institut Gustave Roussy under the conditions established by the European Community (Directive 86/609/CCE) and according to French law. The targeting vector (Figure 1A) was constructed as follows. A fragment encompassing Jak2 exon 13 was amplified by polymerase chain reaction (PCR) on 129S2/SvPas mouse embryonic stem (ES) cell genomic DNA to introduce the GTC > TTC point mutation (617V > F) and subcloned in a vector with a floxed neomycin resistance (NeoR) cassette resulting in a step1 plasmid. A 5′ homologous arm was amplified by PCR and subcloned in step1 plasmid to generate a step2 plasmid. Finally, a 3′ homologous arm was subcloned in step2 plasmid to generate the final targeting construct. Targeted 129S2/SvPas ES clones were confirmed by PCR and Southern blot and injected into C57BL/6J blastocysts to generate chimeric mice. Chimeras (L2) were crossed with flippase (FLP) TG C57BL/6 mice to excise the FRT site-flanked NeoR cassette on F1 progenies (L-). Finally, F1 animals (L-) were crossed with 129Sv mice to generate F2 animals.
Mouse analysis
Blood parameters were determined using an automated MS9 counter (Schloessing Melet). For histology, femur and spleen sections were stained with hematoxylin-eosin-safran and reticulin fibers were revealed by silver staining according to the Gordon Sweet method. Progenitor cell assays were carried out in duplicate in methylcellulose (StemCell Technologies) supplemented or not with cytokines and erythropoietin (EPO).6
Results and discussion
The heterozygous status of all KI mice was confirmed by tail DNA PCR genotyping (Figure 1B). Quantitative allele-specific RT-PCR (Figure 1C) showed that heterozygosity resulted in equal amounts of mutated and wild-type (WT) Jak2 mRNAs, suggesting normal regulation of the Jak2V617F KI allele. Western blot analysis showed that JAK2 protein levels in KI and WT mice were comparable (Figure 1D) but, in the absence of antibody recognizing specifically the mutated or WT proteins, we could not verify that both forms were in equal amounts in KI mice. STAT5 and ERK1/2 downstream signaling molecules were phosphorylated in the absence of added growth factors in KI BM (Figure 1D) and spleen (data not shown). Finally, around 45% of colony forming unit–erythroid (CFU-E) from BM or spleen of KI mice gave rise to endogenous erythroid colonies (EECs; Figure 1E). These results show that JAK2V617F was constitutively activated in KI mice, resulting in EPO hypersensitive or independent growth.
Characterization of the Jak2V617F KI mouse model. (A) Schematic representation of the targeting vector. Homologous recombination into the Jak2 WT allele of mouse embryonic stem (ES) cells resulted into the L2 knock-in (KI) genotype. A correctly targeted ES clone was injected into blastocyst stage embryos to generate L2 chimeric mice. Chimeras were bred with flippase (FLP) transgenic mice to generate L-. (B) PCR analysis of genomic tail biopsy DNA using primers a (5′-CCTGTCTCAGAATCCTTCTCATTTAGGG-3′) and b (5′-CTCCAGGGTTACACGAGTCACC-3′) detects successful recombination events in the L- KI mice (right panel). (C) Wild-type (WT) and mutated Jak2 Taqman allele specific amplification from bone marrow (BM) and spleen RNA samples of 2 KI (within the circle in plain line, studied in duplicate 12 and 20 weeks after birth) and WT mice (in duplicate, within the circle in dashed line) was performed. Standard curve (0%, 50%, and 100%) was carried out from mixtures of plasmids containing Jak2V617F or Jak2WT cDNAs. (D) Constitutive phosphorylation of ERK1/2 (Thr 202/Tyr 204) and STAT5 (Tyr 694) and total JAK2 protein in KI mice identified by Western blot analysis (antibodies from Ozyme). Cells isolated from WT and KI mice were starved for 40 hours and stimulated (+) or not (−) with interleukin-3 and granulocyte-macrophage colony-stimulating factor for 15 minutes. β-actin served as loading control. (Sigma). (E) Autonomous growth in KI mice represented as the percentage of CFU-Es derived from BM or spleen KI mice forming endogenous erythroid colonies (EECs) in the absence of added erythropoietin (mean value ± SD, n = 4). No EEC was detected from control mice. (F) Blood cell parameters (mean value ± SE) from KI (n = 11) and WT (n = 8) mice studied at 12 (± 2) weeks of age. RBC indicates red blood cell; MGV, mean globular volume; WBC, white blood cell; and MPV, mean platelet volume.
Characterization of the Jak2V617F KI mouse model. (A) Schematic representation of the targeting vector. Homologous recombination into the Jak2 WT allele of mouse embryonic stem (ES) cells resulted into the L2 knock-in (KI) genotype. A correctly targeted ES clone was injected into blastocyst stage embryos to generate L2 chimeric mice. Chimeras were bred with flippase (FLP) transgenic mice to generate L-. (B) PCR analysis of genomic tail biopsy DNA using primers a (5′-CCTGTCTCAGAATCCTTCTCATTTAGGG-3′) and b (5′-CTCCAGGGTTACACGAGTCACC-3′) detects successful recombination events in the L- KI mice (right panel). (C) Wild-type (WT) and mutated Jak2 Taqman allele specific amplification from bone marrow (BM) and spleen RNA samples of 2 KI (within the circle in plain line, studied in duplicate 12 and 20 weeks after birth) and WT mice (in duplicate, within the circle in dashed line) was performed. Standard curve (0%, 50%, and 100%) was carried out from mixtures of plasmids containing Jak2V617F or Jak2WT cDNAs. (D) Constitutive phosphorylation of ERK1/2 (Thr 202/Tyr 204) and STAT5 (Tyr 694) and total JAK2 protein in KI mice identified by Western blot analysis (antibodies from Ozyme). Cells isolated from WT and KI mice were starved for 40 hours and stimulated (+) or not (−) with interleukin-3 and granulocyte-macrophage colony-stimulating factor for 15 minutes. β-actin served as loading control. (Sigma). (E) Autonomous growth in KI mice represented as the percentage of CFU-Es derived from BM or spleen KI mice forming endogenous erythroid colonies (EECs) in the absence of added erythropoietin (mean value ± SD, n = 4). No EEC was detected from control mice. (F) Blood cell parameters (mean value ± SE) from KI (n = 11) and WT (n = 8) mice studied at 12 (± 2) weeks of age. RBC indicates red blood cell; MGV, mean globular volume; WBC, white blood cell; and MPV, mean platelet volume.
Breeding between WT and KI mice yielded heterozygous KI progeny at approximately the expected mendelian frequency (10 of 42 pups). Of 1F1 and 10F2 KI studied mice, 5 died unexpectedly (15 ± 3 weeks), 5 were killed (23 ± 10 weeks) and one 12-week-old mouse is still alive. Parameters from peripheral blood of KI mice were profoundly modified (Figure 1F). The hematocrit increased, the number of red blood cells (RBCs) doubled but their volume decreased (Figure 1F). Iron deficiency (supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article) probably contributed to microcytosis. RBC polychromatophilia, anisocytosis and poikilocytosis were observed (Figure 2A). WBC counts increased 7.3-fold (P < .05) due to a rise in total numbers of granulocytes (12.5-fold), monocytes (3.5-fold), and lymphocytes (3.3-fold). Furthermore, circulating granulocytic precursors (myeloblasts, metamyelocytes; 0.5%-5%) and erythroblasts (0.5%-8.5%) were seen, especially in old mice (Figure 2A). Platelet counts and volume (MPV) increased 4.7-fold and 3-fold, respectively with the presence of giant platelets, indicative of dysmegakaryopoiesis (Figure 2A).
Blood, BM, and spleen features from Jak2V617F KI mice. (A) Blood smears from a 31-week-old Jak2V617F KI mouse revealed RBC polychromatophilia, anisocytosis and poikilocytosis, large platelets, and erythroblastosis (May-Grünwald-Giemsa staining). Images were obtained (63× lens) using a Zeiss Axiophot microscope with a Zeiss AxioCam Mrc camera and AxioVision Rel.4.3 acquisition software. (B) Spleen weight in KI mice proportionally increased with age (mean value ± SD, n = 3). (C) Myeloid trilineage hyperplasia in KI mice. The left panel shows no blockade in the differentiation processes and increases in the cumulative numbers (BM plus spleen) of granulocytic and erythroid precursor cells in KI compared with WT mice (mean value ± SD, n = 2, 27 and 31 weeks old). Calculation is based on the assumption that 1 femur represented 6% of the total marrow and from the number of cells isolated from the spleen. Cell types were identified from May-Grünwald-Giemsa stained cell cytospins. BL indicates blast; MY, myeloblast/myelocyte; ME/PN, metamyelocyte/polymorph; LY, lymphocyte; MO, monocyte; EO, eosinophil; and ERY, erythroblast. The right panel shows clustered megakaryocytes (MKs) with multilobulated nucleus from a hematoxylin/eosin/safran (HES)–stained KI mouse spleen (400× magnification). Images were obtained using a DM2000 Leica microscope and a DFC300FX Leica camera with Leica Application Suite v.2.5,OR1 acquisition software. (D-E) Histology of the spleen. (D) Hematoxylin-eosin coloration of a 12-week-old KI mouse revealed hyperplasia of the red pulp with the partially preserved white pulp that was clearly visible in a WT mouse (arrows). In contrast, white pulp of a 27-week-old KI mouse was completely blended. (25× magnification). (E) Silver stain coloration indicated high-grade fibrosis in a 36-week-old mouse. Fibrosis was absent in 12-week-old KI and 27-week-old WT mice (200× magnification). (F) Cumulative numbers of progenitor cells in BM and spleen from KI and WT mice scored after 2 (CFU-E) or 7 (BFU-E and CFU-GM) days of culture (mean value ± SE, n = 4, 21 ± 5 weeks of age). WT littermates were usually used as controls.
Blood, BM, and spleen features from Jak2V617F KI mice. (A) Blood smears from a 31-week-old Jak2V617F KI mouse revealed RBC polychromatophilia, anisocytosis and poikilocytosis, large platelets, and erythroblastosis (May-Grünwald-Giemsa staining). Images were obtained (63× lens) using a Zeiss Axiophot microscope with a Zeiss AxioCam Mrc camera and AxioVision Rel.4.3 acquisition software. (B) Spleen weight in KI mice proportionally increased with age (mean value ± SD, n = 3). (C) Myeloid trilineage hyperplasia in KI mice. The left panel shows no blockade in the differentiation processes and increases in the cumulative numbers (BM plus spleen) of granulocytic and erythroid precursor cells in KI compared with WT mice (mean value ± SD, n = 2, 27 and 31 weeks old). Calculation is based on the assumption that 1 femur represented 6% of the total marrow and from the number of cells isolated from the spleen. Cell types were identified from May-Grünwald-Giemsa stained cell cytospins. BL indicates blast; MY, myeloblast/myelocyte; ME/PN, metamyelocyte/polymorph; LY, lymphocyte; MO, monocyte; EO, eosinophil; and ERY, erythroblast. The right panel shows clustered megakaryocytes (MKs) with multilobulated nucleus from a hematoxylin/eosin/safran (HES)–stained KI mouse spleen (400× magnification). Images were obtained using a DM2000 Leica microscope and a DFC300FX Leica camera with Leica Application Suite v.2.5,OR1 acquisition software. (D-E) Histology of the spleen. (D) Hematoxylin-eosin coloration of a 12-week-old KI mouse revealed hyperplasia of the red pulp with the partially preserved white pulp that was clearly visible in a WT mouse (arrows). In contrast, white pulp of a 27-week-old KI mouse was completely blended. (25× magnification). (E) Silver stain coloration indicated high-grade fibrosis in a 36-week-old mouse. Fibrosis was absent in 12-week-old KI and 27-week-old WT mice (200× magnification). (F) Cumulative numbers of progenitor cells in BM and spleen from KI and WT mice scored after 2 (CFU-E) or 7 (BFU-E and CFU-GM) days of culture (mean value ± SE, n = 4, 21 ± 5 weeks of age). WT littermates were usually used as controls.
The number of nucleated cells collected from femurs (16 ± 2 × 106/femur) was lower than in controls (21 ± 2 × 106/femur; P < .05, n = 5, week 21 ± 6). An increase in neutrophil precursors (1.5-fold) and a drop in both erythroblasts (2-fold) and lymphocytes (3-fold) were observed. There was no shift in the proportion of immature precursor cells showing that maturation was unaffected. Spleen weights from KI mice increased over the time of survey (Figure 2B). Splenomegaly was due to an increase in erythroid (88-fold) and myeloid (82-fold) precursors without any noticeable blockage of maturation. Cumulative numbers in BM plus spleen showed an increase in erythroid and myeloid precursors but no change in the total lymphocyte population (Figure 2C). Differential count data in blood, BM and spleen were confirmed by fluorescence-activated cell sorting analysis with lineage markers (data not shown). Histologic examination of the spleens also revealed clusters of megakaryocytes (MKs) with a multilobulated nucleus and granulocyte emperipolesis demonstrating megakaryocytic hyperplasia (Figure 2C right panel). Spreading of the red pulp with progressive extinction of the white pulp with age emphasized myeloid trilineage hyperplasia (Figure 2D). Grade 3 fibrosis with low collagen deposition was evidenced in spleen (Figure 2E) and BM of aged mice (around week 30). Extramedullary hematopoiesis was observed in the liver with the presence of MKs, granulocytes and erythroblasts (data not shown). Finally, cumulative numbers of CFU-E, burst-forming unit–erythroid (BFU-E), and colony-forming unit–granulocyte-macrophage (CFU-GM) progenitor cells in BM and spleen of KI mice were increased 87-, 6-, and 4-fold, respectively, compared with control (Figure 2F). The progenitor pool amplification was mostly due to splenic hematopoiesis.
This study shows for the first time that heterozygous expression of JAK2V617F in KI mice induces a severe PV-like disorder leading to myelofibrosis. The disease is similar to some phenotypes previously described in RV-transduced5,6 and especially low expresser TG9,10 models. In contrast, Jak2V617F heterozygosity in patients is usually associated with the development of ET.4 The absence of ET-like disease in the KI mice may be due to several reasons. First, the embryonic development of this inherited disease, compared with the adult acquired human disease, may have changed the disease phenotype. However, heterozygous KI induced in adult life (our preliminary results and Akada et al11 ) also lead to PV-like phenotypes. Second, heterozygous patients developing PV exist but, compared with heterozygous ET patients, display a majority of mutated progenitor cells.12 If it is the reason for PV development in heterozygous patients, it is not surprising that 100% mutated progenitors in KI mice give rise to a PV phenotype. Third, genetic differences between human and mice and between mouse strains5 should be taken into consideration. Among these differences, the JAK2V617F signaling complex, including receptors, positive and negative regulator interactions, may be more active, long-lasting, and more competitive toward the JAK2WT signaling complex in mice than in humans.
To date, no Jak2V617F inherited human disorder has been described although Jak2V617F acquired familial forms of MPNs exist.13 The severity of the disease suggests that an inherited disorder may be embryo-lethal in human. In conclusion, we have described the effects of a constitutive heterozygous Jak2V617F mutation in mice. Work remains to understand the absence of an ET-like phenotype and to study potential nonhematopoietic phenotypes.
Addendum
During the review of this paper Akada et al11 demonstrated that heterozygous and homozygous Jak2V617F KI induced after birth developed a PV-like disease that is transplantable in recipient mice. Hematologic parameters of our constitutive KI mouse resemble those of the homozygous inducible KI mice, both models being analyzed at similar ages in a C57Bl6/129Sv background.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We are grateful to Carole Beaumont (Inserm U773, Centre de Recherche Biomédicale Bichat Beaujon, Université Paris Diderot Paris, UFR de Médecine site Bichat, Paris, France) for the iron status investigation, and Françoise Wendling for critically reviewing the manuscript. We thank the staff of the animal facilities of the Institut Gustave Roussy directed by Patrick Gonin. The mouse mutant line was established at the Mouse Clinical Institute (Institut Clinique de la Souris, MCI/ICS) in the Targeted Mutagenesis and Transgenesis Department with funds from the Ligue Nationale contre le Cancer, Cancéropôle ÎIle-de-France, and Cancer, Aidez la Recherche. C.M. is a recipient of the Institut National du Cancer (INCa) and the Fondation de France.
Authorship
Contribution: C.M. and C.L. designed the study, performed research, and analyzed data; A.M. performed the histopathology; S.H. performed research; S.J. and M.-C.B. generated the KI mice; W.V. designed the study; and J.-L.V. designed the study, performed research, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Jean-Luc Villeval, Inserm U1009, Institut Gustave Roussy, PR1, 114 rue Edouard Vaillant, 94805 Villejuif, France; e-mail: villeval@igr.fr.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal