Abstract
Abstract 700
Studies conducted over the last 10 years suggest that 3–5% of the general population over age 40 harbor a clonal population of lymphocytes of CLL phenotype when evaluated using sensitive flow cytometry assays (Rawstron Blood 100:635, 2002; Ghia Blood 103:2337, 2003). This discovery led to creation of the new diagnostic entity, monoclonal B-cell lymphocytosis (MBL; Marti BJH 130:325, 2005), which is considered the precursor state to chronic lymphocytic leukemia (CLL) (Landgren NEJM 360:659, 2009).
The current diagnostic criteria for CLL-like MBL specify patients have a clonal B-cell population with appropriate phenotype, an absolute B-cell count <5 × 10^9/L, and no characteristics of a lymphoproliferative disorder (e.g. lymphadenopathy, organomegaly, B-symptoms) while individuals with a clone of CLL phenotype and B-cell count >5 × 10^9/L or who have lymphadenopathy are classified as having CLL (Hallek Blood 111:5446, 2008).
The natural history of MBL appears to differ based on the absolute B-cell count. From an epidemiologic perspective, the majority of individuals with MBL have very small clonal lymphocyte populations, B-cell counts within the normal range, and appear to be at low likelihood of developing CLL (Rawstron ASH 2009). Such individuals with “low count” MBL do not appear to be at increased risk of death (Rawstron ASH 2009).
From a clinical perspective, most patients with MBL are identified due to lymphocytosis and have B-cell counts between 3–5 × 10^9/L. While such individuals with “high count” MBL progress to require treatment for CLL at a rate of ~1.5% per year (Shanafelt JCO 27:3959, 2009), whether their survival differs from that of age- and sex-matched individuals is unknown. Conceptually, patients with the precursor state to malignancy should have a risk of death similar to those without the precursor state unless they progress to develop malignancy.
To determine the impact of clinically “high count” MBL on survival, we compared the survival of 300 patients with clinically recognized MBL to the age- and sex-matched population. In addition, to explore whether the current B-cell threshold used to segregate MBL from CLL optimally classifies risk, we also evaluated the survival of 94 patients with newly diagnosed Rai 0 CLL and a B-cell count between 5–10 × 10^9/L and 218 newly diagnosed Rai 0 CLL patients with an ALC > 10 × 10^9/L to the age- and sex-matched population.
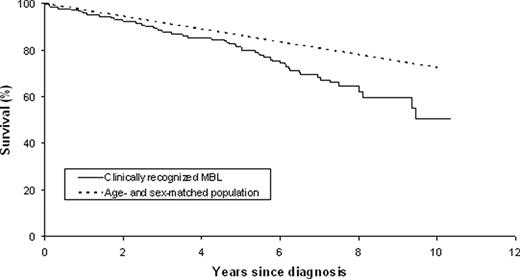
Although it appeared slightly lower, the survival of patients with clinical recognized MBL (n=300, median age 68.6) was not statistically different than age- and sex-matched individuals (p=0.14; Figure 1A). In contrast, the survival of patients with newly diagnosed Rai 0 CLL and a B-cell count between 5–10 × 10^9/L (p=0.03) and newly diagnosed Rai 0 CLL patients with an ALC > 10 × 10^9/L (p=0.00018) were both significantly shorter than expected for the age- and sex-matched population.
While these data are consistent with the designation of clinically recognized MBL as a premalignant condition, a more nuanced story emerged when the individuals with clinically recognized MBL were stratified by the CD38 status of the B-cell clone. Although the survival of individuals with a CD38- clone (n=213; 78%) was not different than age- and sex-matched individuals (p=0.14), the survival for those with a CD38+ clone (n=59; 22%) was substantially shorter than the age- and sex-matched population (p=0.0002; Figure 1B).
Collectively, these data provide additional clinical evidence in support of the 5 × 10^9/L B-cell threshold to distinguish between MBL and CLL as patients with a B-cell count between 5–10 × 10^9/L or higher are at increased risk of death compared to the age- and sex-matched population. However they also suggest that, in addition to absolute B-cell count, biologic characteristics of the B-cell clone influence survival in patients with clinically recognized MBL. Additional studies are needed to determine whether such characteristics should be considered when classifying individuals with B-cell clones <5 × 10^9/L as having a premalignant or malignant condition.
Survival of patients with clinically recognized MBL (n=300) compared to the age- and sex-matched general population
Survival of patients with clinically recognized MBL (n=300) compared to the age- and sex-matched general population
Survival of patients with clinically recognized MBL by CD38 status compared to the age- and sex-matched general population. CD38- p=0.14, CD38+ p=0.0002
Survival of patients with clinically recognized MBL by CD38 status compared to the age- and sex-matched general population. CD38- p=0.14, CD38+ p=0.0002
Shanafelt:Celgene: Research Funding; Hospira: Research Funding; Genentech: Research Funding. Off Label Use: Lenalidomide. Kay:Celgene: Research Funding; Hospira: Research Funding; Genentech: Research Funding. Zent:Genzyme: Research Funding; Genentech: Research Funding; Novartis: Research Funding; G.S.K.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal