Abstract
Abstract 2427
The introduction of chemo-immunotherapy (R-FC) has led to impressive improvement of response, PFS and remarkably overall survival in CLL. Irrespective of these improvements, the genetic markers remain important predictors of outcome. With increasing intensity of 1st line treatment, the proportion of patients with refractory disease is decreasing. At the same time the selective pressure on tumor cells increases. Relatively little is known about the genetic profile of risk groups as defined by the length of 1st remission. We therefore analysed the CLL8 cohort (FC vs. FCR in untreated and fit patients with CLL) to identify the genetic profile (before 1st line treatment) of patients either not responding to (refractory) or relapsing early after first line therapy.
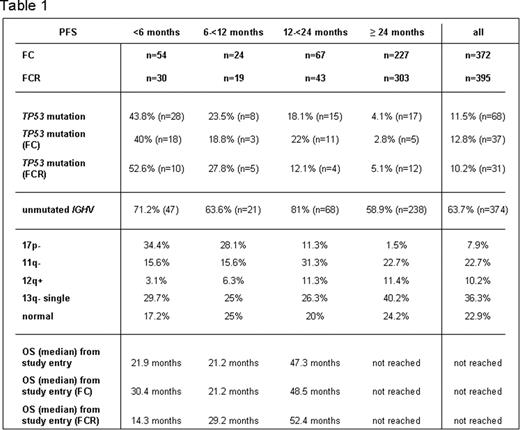
In order to characterize the genetic profile of refractory CLL and CLL with early relapse we formed 4 cohorts based on response and response duration after initial therapy. We selected F-refractory (no PR/CR or PR/CR < 6 months), patients with PFS 6−<12 months, 12−<24 months and ≥ 24 months for the analysis. Median follow-up was 37.7 months. Genetic characterization was performed in a central laboratory (Ulm). Data was available for IGHV (n=587), TP53 mutation (n=592), and FISH (n=581).
Based on the above definition 84/767 (11%) patients were F-refractory. Very short PFS was observed in 43/767 (5.6%)(6−<12 months) and 110/767 (14.3%)(12−<24 months).
The overall survival (OS) of patients in the 4 categories was significantly different with median OS (from study entry) of 21.9 months (F-refractory patients), 21.2 months (PFS 6−<12 months), and 47.3 months (12−<24 months) compared to not reached in patients with a median PFS ≥24 months.
When comparing the treatment arms, the overall number of patients with short remission was lower in the FCR arm (Table 1).
As shown in Table 1, the incidence of 17p- and TP53 mutation is highest in the F-refractory group with similar distribution in both treatment arms (34.4% 17p-; 43.8% TP53). In the subgroup of patients with very short PFS (6−<12 months) the incidence of highest risk genetic aberrations was still high (17p- 28.1%; TP53 mutation 23.5%). In contrast the fraction of patients with these aberrations was very low (1.5 and 4.1% resp.) in the group of patients with long PFS (≥24 months).
Conversely, the incidence of good risk genetics (e.g. 13q- single) increased with length of remission (Table 1). Similarly, the incidence of trisomy 12 was higher in patients with longer PFS (11.3% and 11.4% for PFS 12−<24 months)(Table 1).
Early relapse (within 24 months) is associated with high risk genetics (TP53 mutation and 17p deletion). In addition to patients with F-refractory CLL, patients relapsing within 6–12 and 12–24 months after intense 1st line treatment have a poor overall survival. Decisions on 2nd line treatment options should integrate genetic characterisation and remission duration.
Zenz: Roche: Honoraria; Boehringer: Honoraria; GSK: Honoraria; Celgene: Honoraria. Fink: Roche: Travel grant. Fischer: Roche: Travel grant. Kneba: Roche: Honoraria, Research Funding. Boettcher: Roche: Research Funding. Mendila: Roche: Employment. Wenger: Roche: Employment. Hallek: Roche: Honoraria, Research Funding. Döhner: Roche: Research Funding. Stilgenbauer: Roche, Celgene, GSK, Boehringer, Genzyme: Honoraria, Research Funding.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal