Abstract
Abstract 2408
Vitamin D insufficiency is common globally and in the United States. Approximately 25–50% of patients seen in routine clinical practice have vitamin D levels below the optimal range with low levels linked to higher cancer incidence. Although vitamin D insufficiency is also related to inferior prognosis in some cancers, no data exists for chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL).
To test the hypothesis that vitamin D levels predict outcome in patients with CLL, we evaluated the relationship of 25 (OH)D serum levels with time-to-treatment (TTT) and overall survival (OS) in 390 newly diagnosed CLL patients participating in a prospective cohort study (discovery cohort) and separate cohort of 153 previously untreated patients participating in an observational study (confirmation cohort). 25 (OH)D levels were measured by liquid chromatography-tandem mass spectrometry. Intra- and inter-assay coefficients of variation were all <7% (data not shown). All vitamin D assays were performed on stored research samples; results were not included in the clinical record and were not known to the treating physicians in either study. Vitamin D insufficiency was defined as a serum 25 (OH)D level <25 ng/mL (62.5 nmol/L), an accepted level3 for the establishment of hypovitaminosis D and the threshold used in routine clinical practice to identify individuals with 25 (OH)D insufficiency by our laboratory in routine clinical practice (http://www.mayomedicallaboratories.com).
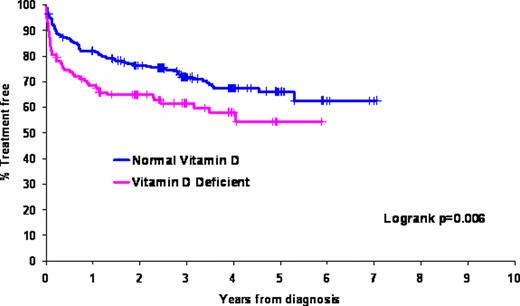
We evaluated the relationship of 25 (OH)D serum levels with time-to-treatment (TTT) and overall survival (OS) in newly diagnosed CLL patients participating in a prospective cohort study (discovery cohort) and a separate cohort of previously untreated patients participating in an observational study (confirmation cohort). Of 390 CLL patients in the discovery cohort, 119 (30.5%) were 25 (OH)D insufficient. 25 (OH)D insufficiency had no relationship with CD38, ZAP-70, CD49d or IGHV mutation status and had no relationship with FISH risk category as classified using the Dohner system. After median follow-up of 3 years, TTT (hazard ratio [HR]=1.66; p=0.005) and OS (HR=2.39; p=0.01) were shorter for 25 (OH)D insufficient patients (figure). We next attempted to validate these findings in an independent group of previously untreated CLL patients. In the validation cohort, 61 of 153 patients (39.9%) were 25 (OH)D insufficient. After median follow-up of 9.9 years, TTT (HR=1.59; p=0.05) and OS (HR 1.63; p=0.06) were again shorter for 25 (OH)D insufficient patients. On pooled multivariable analysis of patients in both cohorts adjusting for age, sex, stage, CD38, ZAP-70, IGHV, CD49d, and FISH, 25 (OH)D insufficiency remained an independent predictor of TTT (HR=1.47; p=0.008). On multivariable analysis for OS, the HR for death associated with 25 (OH)D insufficiency was similar to univariate findings although the p value did not reach the threshold of statistical significance (HR=1.47; 95% CI=0.97–2.23; p=0.07).
25 (OH)D insufficiency is associated with inferior TTT and OS in CLL patients. Whether normalizing vitamin D levels in deficient CLL patients would improve outcome merits clinical testing.
Figure: Time from Diagnosis to Treatment in Discovery Cohort (n=390)
Figure: Time from Diagnosis to Treatment in Discovery Cohort (n=390)
Zent: Genzyme: Research Funding; Genentech: Research Funding; Novartis: Research Funding; G.S.K.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal