Abstract
Seventeen patients transplanted with hematopoietic cells to correct severe T lymphocyte immunodeficiency resulting from complete DiGeorge anomaly were identified worldwide, and retrospective data were obtained using a questionnaire-based survey. Patients were treated at a median age of 5 months (range, 2-53 months) between 1995 and 2006. Bone marrow was used in 11 procedures in 9 cases: 6 from matched unrelated donors, 4 from human leukocyte antigen (HLA)-identical siblings, and one haploidentical parent with T-cell depletion. Unmobilized peripheral blood was used in 8 cases: 5 from HLA-identical siblings, one from a matched unrelated donor, one from an HLA-identical parent, and one unrelated matched cord blood. Conditioning was used in 5 patients and graft-versus-host disease prophylaxis in 11 patients. Significant graft-versus-host disease occurred in 9 patients, becoming chronic in 3. Median length of follow-up was 13 months, with transplantation from HLA-matched sibling showing the best results. Median survival among deceased patients (10 patients) was 7 months after transplantation (range, 2-18 months). The overall survival rate was 41%, with a median follow-up of 5.8 years (range, 4-11.5 years). Among survivors, median CD3 and CD4 counts were 806 (range, 644-1224) and 348 (range, 225-782) cells/mm3, respectively, CD4+/CD45RA+ cells remained very low, whereas mitogen responses were normalized.
Introduction
The DiGeorge anomaly (DGA) results from failure of normal third and fourth pharyngeal pouch development, leading to absence or hypoplasia of the parathyroid glands, conotruncal anomalies, and thymic hypoplasia or aplasia, causing variable T lymphocyte deficiency. DGA, also known as DiGeorge syndrome, can occur as a part of several entities of which 22q11 microdeletion hemizygosity is the most common with an incidence of 1 in 3000 to 4000 live births. It is also described in other chromosomal abnormalities, including CHARGE syndrome (colobomas, heart malformations, atresia of the choanae, retarded growth and development, genital abnormalities, and ear anomalies)1 and as a complication of diabetic embryopathy.2,3 The phenotype of patients with DGA may vary widely.4 Less than 1% of patients present with complete athymia leading to a life-threatening T lymphocyte defect with a T−B+NK+ severe combined immunodeficiency (SCID) phenotype (complete DiGeorge anomaly [cDGA]).4 In typical forms of cDGA, T lymphocytes are absent or present in extremely low numbers (< 50 CD3+ cells/mm3), and there is an absent or very low proliferative response to mitogens such as phytohemagglutinin. In atypical forms of cDGA, characterized by oligoclonal peripheral T lymphocyte expansion, often associated with erythroderma and lymphadenopathy, the diagnosis is based on a lack of naive T lymphocytes (< 50 CD3+CD45RA+CD62L+ cells/mm3), indicating absence of recent thymic emigrants.5
Patients with cDGA present a therapeutic challenge. In contrast to patients with other forms of SCID, the absence of T lymphocytes is the result of a lack of thymic environment rather than an intrinsic hematopoietic defect.6 Thus, patients treated with bone marrow transplantation can achieve peripheral engraftment of post-thymic donor T lymphocytes but do not demonstrate ongoing T-cell lymphopoiesis. Adoptive transfer of cells of hematopoietic origin, achieving long-term survival of the patient, has been published in a few case reports only, including the use of bone marrow in 5 patients,7-11 cord blood in one,12 and peripheral blood lymphocyte (PBL) infusion in 4.13-16
Reports of the use of thymus transplantation in athymic infants has shown very promising results initially using fetal tissue17,18 and more recently postnatal infant thymuses.1,19 As the current literature reports only individual cases and publication bias was suspected, we performed a retrospective, worldwide, questionnaire-based survey on outcome of cDGA patients transplanted with cells of hematopoietic origin.
Methods
Data collection
Centers in Europe known to have performed hematopoietic cell transplantation (HCT) for T lymphocyte deficiency in patients with cDGA were identified through the Stem Cell Transplantation for Immunodeficiencies in Europe registry in Paris; other centers were contacted based on a literature search of published case reports and through personal communication. Data from a detailed survey questionnaire were obtained on 17 patients transplanted in 10 centers in 4 European countries, Canada, Japan, and the United States, between 1995 and 2006 with follow-up between 2 months and 12 years (median, 13 months). Partial data from 9 of these 17 patients have been previously published in individual reports.6,8,10,11,14-16,20
Patient characteristics
Characteristics of the 17 patients based on data from the questionnaires are shown in Table 1. All had features consistent with cDGA (T−B+NK+ SCID phenotype). Absence of thymus was demonstrated by chest radiograph (patients 4, 7, and 16), nuclear magnetic resonance imaging (patient 13), ultrasound (patient 9), or by direct inspection at surgery (patients 5 and 8). More than one method was used for some patients. At presentation, the T lymphocytes were absent (< 50 CD3+ cells/mm3) in 14 patients; in 3 (patients 9, 11, and 16), 142, 70, and 150 T lymphocytes/mm3, respectively, were detected, but no cells of naive (CD45RA+) phenotype. More specific markers for recent thymic emigrants (T lymphocyte receptor excision circles [TRECs] or CD45RA+/CD62L+) were missing in all 3 of the patients tested (patients 6-8). Maternofetal engraftment was not detected in any of the cases. Lymphocyte proliferative response to phytohemagglutinin (PHA) was absent where tested (patients 3, 5-15, and 17). In 8 patients (patients 3, 9, 10, and 13-17) pretransplantation expansion of T lymphocytes was documented; in the 3 patients studied (patients 9, 10, and 14), oligoclonality of T lymphocytes was demonstrated through T-cell receptor-β chain family analysis. Omenn syndrome–like symptoms consistent with atypical cDGA5,6 occurred in 3 cases (patients 9, 11, and 14). A high titer of antithyroid autoantibodies was present in one case (patient 11). Males predominated in the cohort (82%); 8 patients were hemizygous for deletion at 22q11.2 locus. Seven patients had a phenotype consistent with CHARGE syndrome; in 5 of 6 tested, a mutation in CHD7 was found. In one patient, the molecular defect has unclear significance as it is outside the normal genetic region affected in CHARGE syndrome and the mother has the same genotype with no clinical correlate.
Patient characteristics (n = 17)
| Case no. . | Sex . | Country . | Dysmorphic face . | Cardiac anatomy . | Other anomalies . | Detection method of thymus absence . | CD3+/mm . | Hypopara-thyroidism . | CHARGE association . | Molecular defect (del22q11.2/CHD7) . | Infections before transplantation . | Reference . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | Germany | Present | Normal | Renal, genital, PMR | CXR, US | 0 | Present | None | Present/ND | None | 16 |
| 2 | Male | Canada | None | ToF with intra-auricular defect | None | Surgery, CXR, CT | 0 | Present | None | Present/ND | None | |
| 3 | Male | Japan | Present | ToF, absence of pulmonary valve | Cleft palate, tracheobronchomalacia, atopic dermatitis-like skin eruptions | Surgery, CXR, CT, US | 4-107 | Present | None | Present/ND | Sepsis, 2 aseptic meningitis, and echovirus in urine | 8 |
| 4 | Male | France | Present | ToF | GER, facial nerve palsy | CXR | 9 | Present | None | Present/ND | Severe CMV infection, pneumonitis | |
| 5 | Male | United Kingdom | Present | AVSD | Cryptorchidism, micropenis, Dandy-Walker malformation | Surgery | 17 | None | None | None/none | Pneumonia (Pseudomonas spp), gastroenteritis (rotavirus) | |
| 6 | Female | United Kingdom | Present | VSD, ASD, PDA | Unilateral coloboma, hemivertebrae | Surgery, CXR | 0 | Present | Present | None/present | None | 6 (patient 1) |
| 7 | Male | United Kingdom | Present | PDA | Bilateral coloboma and choanal atresia, GER, tracheoesophageal fistula, micropenis | CXR | 0 | NA | Present | None/present | Pneumonitis, chronic lung disease | 6 (patient 2) |
| 8 | Female | United Kingdom | Present | ToF | Bilateral coloboma, Dandy-Walker malformation | Surgery | 0 | Present | Present | None/present* | None | |
| 9 | Male | United Kingdom | Present | ASD, PDA, left pulmonary vein stenosis | Dandy-Walker malformation, unilateral coloboma, absent left tibia, bilateral talipes, right preaxial polydactyly, bilateral cryptorchidism, micropenis, macular rash on the upper trunk, hepatomegaly | US | 142-200† (93% DR+, only CD4+) | Present | Present | None/present | None | 6 (patient 3) |
| 10 | Male | France | Present | Normal | Renal | CXR, US | 0-970† | Present | None | Present/ND | None | |
| 11 | Male | France | Present | Normal | Microencephaly, thyroiditis, velopharyngeal insufficiency, eczema with elevated IgE, GER, PMR, autoimmune thyroiditis, severe growth failure | CXR, US | 70 | Present | None | Present/ND | Sepsis and severe infections: sinusitis, pneumonias (C albicans, S aureus, P aeruginosa, S pneumoniae), CMV enteritis | 14, 15 |
| 12 | Male | Czech Republic | Present | PDA, right-sided aortal arch, FOA | Bilateral retinal coloboma and choanal atresia, esophageal atresia with tracheobronchial fistula, tracheobronchomalacia, GER, genital anomalies, breath-holding attacks, PMR | Surgery, MRI | 0 | Present | Present | None/ND | Sepsis (multiple organisms) | 10 |
| 13 | Male | United Kingdom | Present | PDA, FOA | Bilateral coloboma, cleft palate, tracheobronchomalacia, absence of cerebellar vermis and cerebellar hypoplasia | MRI | 0-130 | None | Present | None‡/ND | Severe infection (parainfluenza, Pseudomonas spp) | |
| 14 | Female | France | None | Normal | Maternal diabetes, PMR, erythrodermia | CXR, US | 0-1830† | Present | None | None‡/ND | None | |
| 15 | Male | USA | Present | Aberrant left subclavian artery | Unilateral choanal atresia, GER, VUR (grade 5), tracheobronchomalacia, gothic web, ankyloglossia, microgastria, vertical talus, scoliosis, 2-3 toe syndactyly, Coombs-positive hemolytic anemia | CXR, CT | 4-85 | Present | Present | None/present | E faecium urinary tract infection | 20 |
| 16 | Male | Canada | Present | Normal | Growth retardation, GER, PMR | CXR | 150-250 | Present | None | Present/ND | Severe bronchopneumonia (parainfluenza), recurrent thrush | 11 |
| 17 | Male | USA | Present | ToF | Renal | Surgery, CXR | 0-224 | Present | None | Present/ND | Severe sepsis (B cereus, Enterobacter spp, R equi) |
| Case no. . | Sex . | Country . | Dysmorphic face . | Cardiac anatomy . | Other anomalies . | Detection method of thymus absence . | CD3+/mm . | Hypopara-thyroidism . | CHARGE association . | Molecular defect (del22q11.2/CHD7) . | Infections before transplantation . | Reference . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | Germany | Present | Normal | Renal, genital, PMR | CXR, US | 0 | Present | None | Present/ND | None | 16 |
| 2 | Male | Canada | None | ToF with intra-auricular defect | None | Surgery, CXR, CT | 0 | Present | None | Present/ND | None | |
| 3 | Male | Japan | Present | ToF, absence of pulmonary valve | Cleft palate, tracheobronchomalacia, atopic dermatitis-like skin eruptions | Surgery, CXR, CT, US | 4-107 | Present | None | Present/ND | Sepsis, 2 aseptic meningitis, and echovirus in urine | 8 |
| 4 | Male | France | Present | ToF | GER, facial nerve palsy | CXR | 9 | Present | None | Present/ND | Severe CMV infection, pneumonitis | |
| 5 | Male | United Kingdom | Present | AVSD | Cryptorchidism, micropenis, Dandy-Walker malformation | Surgery | 17 | None | None | None/none | Pneumonia (Pseudomonas spp), gastroenteritis (rotavirus) | |
| 6 | Female | United Kingdom | Present | VSD, ASD, PDA | Unilateral coloboma, hemivertebrae | Surgery, CXR | 0 | Present | Present | None/present | None | 6 (patient 1) |
| 7 | Male | United Kingdom | Present | PDA | Bilateral coloboma and choanal atresia, GER, tracheoesophageal fistula, micropenis | CXR | 0 | NA | Present | None/present | Pneumonitis, chronic lung disease | 6 (patient 2) |
| 8 | Female | United Kingdom | Present | ToF | Bilateral coloboma, Dandy-Walker malformation | Surgery | 0 | Present | Present | None/present* | None | |
| 9 | Male | United Kingdom | Present | ASD, PDA, left pulmonary vein stenosis | Dandy-Walker malformation, unilateral coloboma, absent left tibia, bilateral talipes, right preaxial polydactyly, bilateral cryptorchidism, micropenis, macular rash on the upper trunk, hepatomegaly | US | 142-200† (93% DR+, only CD4+) | Present | Present | None/present | None | 6 (patient 3) |
| 10 | Male | France | Present | Normal | Renal | CXR, US | 0-970† | Present | None | Present/ND | None | |
| 11 | Male | France | Present | Normal | Microencephaly, thyroiditis, velopharyngeal insufficiency, eczema with elevated IgE, GER, PMR, autoimmune thyroiditis, severe growth failure | CXR, US | 70 | Present | None | Present/ND | Sepsis and severe infections: sinusitis, pneumonias (C albicans, S aureus, P aeruginosa, S pneumoniae), CMV enteritis | 14, 15 |
| 12 | Male | Czech Republic | Present | PDA, right-sided aortal arch, FOA | Bilateral retinal coloboma and choanal atresia, esophageal atresia with tracheobronchial fistula, tracheobronchomalacia, GER, genital anomalies, breath-holding attacks, PMR | Surgery, MRI | 0 | Present | Present | None/ND | Sepsis (multiple organisms) | 10 |
| 13 | Male | United Kingdom | Present | PDA, FOA | Bilateral coloboma, cleft palate, tracheobronchomalacia, absence of cerebellar vermis and cerebellar hypoplasia | MRI | 0-130 | None | Present | None‡/ND | Severe infection (parainfluenza, Pseudomonas spp) | |
| 14 | Female | France | None | Normal | Maternal diabetes, PMR, erythrodermia | CXR, US | 0-1830† | Present | None | None‡/ND | None | |
| 15 | Male | USA | Present | Aberrant left subclavian artery | Unilateral choanal atresia, GER, VUR (grade 5), tracheobronchomalacia, gothic web, ankyloglossia, microgastria, vertical talus, scoliosis, 2-3 toe syndactyly, Coombs-positive hemolytic anemia | CXR, CT | 4-85 | Present | Present | None/present | E faecium urinary tract infection | 20 |
| 16 | Male | Canada | Present | Normal | Growth retardation, GER, PMR | CXR | 150-250 | Present | None | Present/ND | Severe bronchopneumonia (parainfluenza), recurrent thrush | 11 |
| 17 | Male | USA | Present | ToF | Renal | Surgery, CXR | 0-224 | Present | None | Present/ND | Severe sepsis (B cereus, Enterobacter spp, R equi) |
ToF indicates tetralogy of Fallot; AVSD, atrioventricular septal defect; VSD, ventricular septal defect; ASD, atrial septal defect; PDA, patent ductus arteriosus; FOA, foramen ovale apertum; PMR, psychomotor retardation; GER, gastroesophageal reflux; VUR, vesicoureteral reflux; CXR, chest x-ray; US, ultrasound; CT, computed tomography; MRI, magnetic resonance imaging; NA, not available; and ND, not done.
The mutation found is outside the typical region; the mother of the child bears the same mutation with no clinical correlate.
Autologous expansion of T cells.
Deletion at 10p excluded.
In the pretransplantation period, 10 patients had significant infections resulting from Pseudomonas spp. (4), Bacillus cereus (1), Enterobacter spp. (1), Enterococcus faecium (1), Rhodococcus equi (1), Stenotrophomonas maltophilia (1), Acinetobacter (1), echovirus (1), cytomegalovirus (CMV; 2), rotavirus (1), parainfluenza (2), and Candida (2). Some patients experienced infection with more than one organism. Infection with Pneumocystis jiroveci was not reported.
Transplantation
Donor and recipient human leukocyte antigen (HLA) matching was determined by serology and/or molecular analysis. Serologic methods were used for the earlier patients and low-resolution class I with high-resolution class II molecular DNA typing in the more recent patients; methods were dependent on each center's practice.
Seven patients had HLA-identical sibling donors: 2 received unmanipulated marrow and 5 PBL. Seven patients received grafts from unrelated donors (6 bone marrow, one PBL) of which 6 were full (10 of 10) matches and one was mismatched at the HLA-B locus. Two patients received phenotypically matched parental hematopoietic stem cells, one T lymphocyte–depleted bone marrow, and one B lymphocyte–depleted PBL. Cord blood from a matched unrelated donor was used in one patient.
Transplantation data are outlined (Table 2). Median age at transplantation was 5 months (range, 2-53 months). Four patients received serotherapy resulting from the presence of residual T lymphocytes: alemtuzumab (2), rabbit antithymocyte globulin (one), and anti-CD3 (one). One patient received fludarabine, and the remainder received no pretransplantation conditioning. One patient who was retransplanted received busulfan and cyclophosphamide before the second procedure.
Details of transplantation and outcome (n = 17)
| Case no. . | Age at trans-plantation . | Donor . | HLA match . | Graft . | Conditioning . | GVHD prophylaxis . | Complications . | Severe infections . | Length of follow-up from the first trans-plantation, months . | Outcome . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Source . | CD3+, × 106/kg . | CD34+, × 106/kg . | Acute GVHD . | Chronic GVHD . | Other . | |||||||||
| 1 | 3 mo and day 35, day 63, day 91 | Brother | 10/10 | PBL | 100 | 0 | None | None | Skin, stage I, maximum grade 1 | None | Transitory aregenerative anemia | None | 48 | Alive and well |
| 2 | 6 mo and mo 45 | Brother | 10/10 | PBL; marrow | 0.4 | 0; 5 | None | None | Liver, stage II, maximum grade 2 | None | Mild transient arthritis, foot cellulitis | None | 79 | Alive and well |
| 3 | 13 mo and mo 6 | Brother | 10/10 | Marrow | NA | NA | ATG; Bu + CY | CyA, MTX | None | None | None | None | 12 | Sudden death at home, cause unknown |
| 4 | 3 mo | Sister | 10/10 | PBL | 80 | NA | None | None | None | None | None | CMV, rotavirus | 3 | Died of pneumonitis (CMV) |
| 5 | 5 mo | Unrelated, male | 12/12 | Marrow | 160 | 14 | None | None | None | None | None | None | 2 | Died of circulatory failure during cardiac surgery |
| 6 | 3 mo | Unrelated, male | 10/10 | Marrow | NA | 500 | None | CyA | None | None | None | Streptococcus spp. | 144 | Alive, developmental delay |
| 7 | 6 mo | Father | 5/10 | Marrow* | 0.02 | 20 | None | CyA | None | None | None | None | 4 | Died of respiratory failure |
| 8 | 3 mo and day 55 | Unrelated, female | 11/12 | Marrow | 91 | 3.8 | Campath | CyA | Skin, stage III, maximum grade 2 | None | None | None | 5 | Died of circulatory failure |
| 9 | 4 mo | Unrelated, male | 10/10 | Cord blood | 77 | 1.8 | Campath | CyA, steroids | Skin, stage II, maximum grade 2 | None | None | Parainfluenza | 6 | Died of pneumonitis (parainfluenza) associated with recurrent GER |
| 10 | 2 mo and ? | Sister | 10/10 | PBL; marrow | NA | NA | None | CyA | Gut, stage II, maximum grade 2 | Maximum grade 2 | None | NA | 20 | Alive, retransplanted with marrow December 2006; last follow-up May 15, 2007, no details given |
| 11 | 4.5 y | Sister | 10/10 | PBL | 10 | 0.07 | None | CyA, MMF | None | None | None | None | 96 | Alive and well, autoimmune thyroiditis and eczema resolved after transplant |
| 12 | 6 mo and day 36 | Unrelated, male | 9/10 | Marrow | 1 | 0.2 | None | None; CyA | Skin and liver, stage III-IV, grade 2 | None | Cardiopulmonary instability, capillary leak syndrome, ileus, feeding problems, breath-holding attacks | EBV reactivation (rituximab) | 48 | Alive, developmental delay, feeding difficulties |
| 13 | 7 mo | Unrelated, male | 10/10 | Marrow | 71 | 8.1 | None | CyA, MMF | Skin, stage III; liver and gut, Stage II-IV; maximum grade 4 | Skin, gut, maximum grade 4 | Peritonitis associated with gastrostomy tube leakage, hypertension, renal impairment | EBV reactivation (rituximab), coagulase-negative Staphylococcus spp, E coli, C albicans | 8 | Died of pneumonia, chronic GVHD |
| 14 | 6 mo | Unrelated, male | 10/10 | Marrow | 56 | 24 | OKT3, steroids | CyA, MTX | Skin, stage II; gut, stage II; maximum grade 2 | Maximum grade 2 | Pneumopathy | None | 18 | Died of hypertrophic cardiomyopathy, pneumopathy, suspected pulmonary GVHD |
| 15 | 3 mo | Unrelated, male | 10/10 | PBL | 0.5 | NA | Fludarabine | CyA | Skin, stage III, maximum grade 2 | None | Pulmonary VOD, chronic pleural effusions, pulmonary edema, bowel edema, anasarca, Evans syndrome | B pertusis, HHV6 positivity (cleared with ganciclovir) | 14 | Died of acute renal failure, intractable hyperkalemia and left ventricular dysfunction after open lung biopsy |
| 16 | 5 mo | Brother | 10/10 | Marrow | NA | NA | None | None | None | None | None | None | 62 | Alive and well |
| 17 | 3 mo | Mother | 10/10 | PBL† | 10 | NA | None | None | Skin, stage III-IV; lung suspected, maximum grade 2 | Suspected | Transient pancytopenia | None | 11 | Died of pulmonary hemorrhage after second cardiac surgery |
| Case no. . | Age at trans-plantation . | Donor . | HLA match . | Graft . | Conditioning . | GVHD prophylaxis . | Complications . | Severe infections . | Length of follow-up from the first trans-plantation, months . | Outcome . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Source . | CD3+, × 106/kg . | CD34+, × 106/kg . | Acute GVHD . | Chronic GVHD . | Other . | |||||||||
| 1 | 3 mo and day 35, day 63, day 91 | Brother | 10/10 | PBL | 100 | 0 | None | None | Skin, stage I, maximum grade 1 | None | Transitory aregenerative anemia | None | 48 | Alive and well |
| 2 | 6 mo and mo 45 | Brother | 10/10 | PBL; marrow | 0.4 | 0; 5 | None | None | Liver, stage II, maximum grade 2 | None | Mild transient arthritis, foot cellulitis | None | 79 | Alive and well |
| 3 | 13 mo and mo 6 | Brother | 10/10 | Marrow | NA | NA | ATG; Bu + CY | CyA, MTX | None | None | None | None | 12 | Sudden death at home, cause unknown |
| 4 | 3 mo | Sister | 10/10 | PBL | 80 | NA | None | None | None | None | None | CMV, rotavirus | 3 | Died of pneumonitis (CMV) |
| 5 | 5 mo | Unrelated, male | 12/12 | Marrow | 160 | 14 | None | None | None | None | None | None | 2 | Died of circulatory failure during cardiac surgery |
| 6 | 3 mo | Unrelated, male | 10/10 | Marrow | NA | 500 | None | CyA | None | None | None | Streptococcus spp. | 144 | Alive, developmental delay |
| 7 | 6 mo | Father | 5/10 | Marrow* | 0.02 | 20 | None | CyA | None | None | None | None | 4 | Died of respiratory failure |
| 8 | 3 mo and day 55 | Unrelated, female | 11/12 | Marrow | 91 | 3.8 | Campath | CyA | Skin, stage III, maximum grade 2 | None | None | None | 5 | Died of circulatory failure |
| 9 | 4 mo | Unrelated, male | 10/10 | Cord blood | 77 | 1.8 | Campath | CyA, steroids | Skin, stage II, maximum grade 2 | None | None | Parainfluenza | 6 | Died of pneumonitis (parainfluenza) associated with recurrent GER |
| 10 | 2 mo and ? | Sister | 10/10 | PBL; marrow | NA | NA | None | CyA | Gut, stage II, maximum grade 2 | Maximum grade 2 | None | NA | 20 | Alive, retransplanted with marrow December 2006; last follow-up May 15, 2007, no details given |
| 11 | 4.5 y | Sister | 10/10 | PBL | 10 | 0.07 | None | CyA, MMF | None | None | None | None | 96 | Alive and well, autoimmune thyroiditis and eczema resolved after transplant |
| 12 | 6 mo and day 36 | Unrelated, male | 9/10 | Marrow | 1 | 0.2 | None | None; CyA | Skin and liver, stage III-IV, grade 2 | None | Cardiopulmonary instability, capillary leak syndrome, ileus, feeding problems, breath-holding attacks | EBV reactivation (rituximab) | 48 | Alive, developmental delay, feeding difficulties |
| 13 | 7 mo | Unrelated, male | 10/10 | Marrow | 71 | 8.1 | None | CyA, MMF | Skin, stage III; liver and gut, Stage II-IV; maximum grade 4 | Skin, gut, maximum grade 4 | Peritonitis associated with gastrostomy tube leakage, hypertension, renal impairment | EBV reactivation (rituximab), coagulase-negative Staphylococcus spp, E coli, C albicans | 8 | Died of pneumonia, chronic GVHD |
| 14 | 6 mo | Unrelated, male | 10/10 | Marrow | 56 | 24 | OKT3, steroids | CyA, MTX | Skin, stage II; gut, stage II; maximum grade 2 | Maximum grade 2 | Pneumopathy | None | 18 | Died of hypertrophic cardiomyopathy, pneumopathy, suspected pulmonary GVHD |
| 15 | 3 mo | Unrelated, male | 10/10 | PBL | 0.5 | NA | Fludarabine | CyA | Skin, stage III, maximum grade 2 | None | Pulmonary VOD, chronic pleural effusions, pulmonary edema, bowel edema, anasarca, Evans syndrome | B pertusis, HHV6 positivity (cleared with ganciclovir) | 14 | Died of acute renal failure, intractable hyperkalemia and left ventricular dysfunction after open lung biopsy |
| 16 | 5 mo | Brother | 10/10 | Marrow | NA | NA | None | None | None | None | None | None | 62 | Alive and well |
| 17 | 3 mo | Mother | 10/10 | PBL† | 10 | NA | None | None | Skin, stage III-IV; lung suspected, maximum grade 2 | Suspected | Transient pancytopenia | None | 11 | Died of pulmonary hemorrhage after second cardiac surgery |
Semicolons separate data on each transplantation; time is rounded; PBL is always unmobilized.
NA indicates data not available; ATG indicates rabbit antithymocyte globulin; Bu, busulfan; CY, cyclophosphamide; CyA, cyclosporine A; MTX, methotrexate; MMF, mycophenolate mofetil; VOD, veno-occlusive disease; CMV, cytomegalovirus; EBV, Epstein-Barr virus; HHV6, human herpesvirus 6; and GER, gastroesophageal reflux.
T cell–depleted marrow.
B cell–depleted PBLs.
For graft-versus-host disease (GVHD) prophylaxis, 11 patients received cyclosporin A, of whom 2 also received methotrexate and 2 mycophenolate mofetil. One patient additionally received methylprednisolone. Six patients receiving HLA-matched grafts did not receive any GVHD prophylaxis.
All patients were isolated in high-efficiency particulate air–filtered or laminar flow facilities.
Statistical analysis
The χ2 and t tests were used for statistical analysis of patients' outcome; a P value of .05 or less was considered significant. Analyses were performed using Statistica (Version 7.1, StatSoft).
Results
Engraftment and immune reconstitution
Twelve patients (patients 1, 4-6, 9, and 11-17) showed evidence of T-cell engraftment after a single procedure (Table 3). In 2 patients (patient 15 who received fludarabine conditioning and patient 17 in whom there was no conditioning), there was evidence of some additional myeloid engraftment.
Immunologic reconstitution after transplantation (n = 17)
| Case no. . | Age at last follow-up . | Engraft-ment . | T cells . | B cells . | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CD3+, cells/mm3 . | CD4+, cells/mm3 . | CD8+, cells/mm3 . | IRI+,index . | Mitogen response (PHA) . | TREC or equivalent* . | Naive/memory . | CD19+, cells/mm3 . | IVIg . | Antibody response . | |||||
| CD4+ CD45RA+, percentage of CD4+ . | CD4+ CD45RO+, percentage of CD4+ . | Tetanus . | Hib . | |||||||||||
| 1 | 4 y 3 mo | T | 980 | 430 | 490 | 0.9 | normal† | ND | NA | 68 | 100 | No | Good response | ND |
| 2 | 7 y 1 mo | Yes | 45%‡ | 14%‡ | 31%‡ | 0.5 | NA | ND | ND | ND | 40%‡ | No | ND | ND |
| 3 | 2 y 1 mo | Yes | 496 | 305 | 259 | 1.2 | Normal | ND | 25 | 85 | 365 | Yes | ND | ND |
| 4 | 7 mo | T | 900 | 288 | 612 | 0.5 | NA | ND | ND | ND | 576 | Yes | ND | ND |
| 5 | 7 mo | T | 174 | NA | NA | NA | Normal | NA | NA | NA | NA | Yes | ND | ND |
| 6 | 12 y 3 mo | T | 786 | 348 | 433 | 0.8 | Normal | 0 | NA | NA | NA | No | Good response | Good response |
| 7 | 10 mo | No | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 573 | Yes | ND | ND | |
| 8 | 8 mo | T | 464 | NA | NA | NA | ND | 0 | NA | NA | 590 | Yes | ND | ND |
| 9 | 10 mo | T | 504 | 163 | 293 | 0.6 | ND | 0 | NA | NA | 2236 | Yes | ND | ND |
| 10 | NA | No | 0§ | 0 | 0 | 0 | 50% | NA | NA | NA | 1379 | Yes | ND | ND |
| 11 | 12.5 y | T | 644 | 225 | 419 | 0.5 | 50% | 0 | NA | NA | 243 | No | Good response | Good response |
| 12 | 4 y 6 mo | T | 806 | 265 | 472 | 0.6 | Normal | 0 | 2 | 99 | 219 | Yes | Good response | ND |
| 13 | 1 y 3 mo | T | 1342 | 1065 | 276 | 3.9 | ND | ND | 8 | 84 | 0 | Yes | ND | ND |
| 14 | 2 y | T | 868 | 742 | 56 | 13.3 | Normal | ND | 6 | 95 | 378 | Yes | NA | NA |
| 15 | 1 y 5 mo | Yes | 196 | 160 | 39 | 4.1 | Normal | 0 | NA | NA | 273 | No | ND | ND |
| 16 | 5 y 7 mo | T | 1224 | 782 | 238 | 3.3 | 77% | ND | 1 | 99 | 1786 | No | Good response | Good response |
| 17 | 1 y 2 mo | Yes | 195 | 176 | 12 | 14.7 | 33% | ND | NA | NA | 422 | Yes | ND | ND |
| Case no. . | Age at last follow-up . | Engraft-ment . | T cells . | B cells . | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CD3+, cells/mm3 . | CD4+, cells/mm3 . | CD8+, cells/mm3 . | IRI+,index . | Mitogen response (PHA) . | TREC or equivalent* . | Naive/memory . | CD19+, cells/mm3 . | IVIg . | Antibody response . | |||||
| CD4+ CD45RA+, percentage of CD4+ . | CD4+ CD45RO+, percentage of CD4+ . | Tetanus . | Hib . | |||||||||||
| 1 | 4 y 3 mo | T | 980 | 430 | 490 | 0.9 | normal† | ND | NA | 68 | 100 | No | Good response | ND |
| 2 | 7 y 1 mo | Yes | 45%‡ | 14%‡ | 31%‡ | 0.5 | NA | ND | ND | ND | 40%‡ | No | ND | ND |
| 3 | 2 y 1 mo | Yes | 496 | 305 | 259 | 1.2 | Normal | ND | 25 | 85 | 365 | Yes | ND | ND |
| 4 | 7 mo | T | 900 | 288 | 612 | 0.5 | NA | ND | ND | ND | 576 | Yes | ND | ND |
| 5 | 7 mo | T | 174 | NA | NA | NA | Normal | NA | NA | NA | NA | Yes | ND | ND |
| 6 | 12 y 3 mo | T | 786 | 348 | 433 | 0.8 | Normal | 0 | NA | NA | NA | No | Good response | Good response |
| 7 | 10 mo | No | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 573 | Yes | ND | ND | |
| 8 | 8 mo | T | 464 | NA | NA | NA | ND | 0 | NA | NA | 590 | Yes | ND | ND |
| 9 | 10 mo | T | 504 | 163 | 293 | 0.6 | ND | 0 | NA | NA | 2236 | Yes | ND | ND |
| 10 | NA | No | 0§ | 0 | 0 | 0 | 50% | NA | NA | NA | 1379 | Yes | ND | ND |
| 11 | 12.5 y | T | 644 | 225 | 419 | 0.5 | 50% | 0 | NA | NA | 243 | No | Good response | Good response |
| 12 | 4 y 6 mo | T | 806 | 265 | 472 | 0.6 | Normal | 0 | 2 | 99 | 219 | Yes | Good response | ND |
| 13 | 1 y 3 mo | T | 1342 | 1065 | 276 | 3.9 | ND | ND | 8 | 84 | 0 | Yes | ND | ND |
| 14 | 2 y | T | 868 | 742 | 56 | 13.3 | Normal | ND | 6 | 95 | 378 | Yes | NA | NA |
| 15 | 1 y 5 mo | Yes | 196 | 160 | 39 | 4.1 | Normal | 0 | NA | NA | 273 | No | ND | ND |
| 16 | 5 y 7 mo | T | 1224 | 782 | 238 | 3.3 | 77% | ND | 1 | 99 | 1786 | No | Good response | Good response |
| 17 | 1 y 2 mo | Yes | 195 | 176 | 12 | 14.7 | 33% | ND | NA | NA | 422 | Yes | ND | ND |
Data are given for the last follow-up.
IRI indicates immunoregulatory index; PHA, phytohemagglutinin; IVIg, intravenous immunoglobulin; NA, data not available; T, T cells; Hib, Haemophilus influenzae b; and ND, not done.
TREC equivalent = CD4+CD45RA+CD27+ or CD3+CD45RA+CD62L.
Also stimulated with anti-CD3, CD28.
No absolute cell count available.
Data after first transplantation; details after the second one are not available.
The remaining 5 patients (patients 2, 3, 7, 8, and 10) did not achieve T-cell engraftment after a single procedure. Patient 7 (who received a haploidentical T cell–depleted graft) continued to lack T lymphocytes and died of respiratory failure. In the remaining 4 patients, further procedures with PBL or marrow were undertaken. T-cell engraftment was achieved in 3 patients (patients 2, 3, and 8), follow-up data are lacking in patient 10. Patient 3 received busulfan and cyclophosphamide preconditioning, and full donor engraftment was achieved.
Two other patients (patients 1 and 12) received planned repeated graft infusions despite showing evidence of T-cell engraftment after the initial treatment.
The median T lymphocyte count achieved in engrafted patients was 574 cells/mm3 (range, 0-1342 cells/mm3). TRECs or their equivalents were absent in the 7 patients in whom they were sought. In a further 3 patients, absent or very low numbers of CD4+CD45RA+ T lymphocytes were documented. Patient 3 showed an increasing proportion of naive autologous T lymphocytes to a level of 25% of CD4 cells. Seven of 14 patients with data available had an inverted CD4+/CD8+ ratio (< 1.0) after transplantation. A normal lymphocyte proliferation response to phytohemagglutinin was found in all patients tested (Table 3).
Infection after transplantation
Most infectious complications were viral (Table 2), but bacterial infections were significant in some patients. Patient 13 had pneumonia and sepsis, multiple organisms were isolated, including coagulase-negative Staphylococcus spp, Escherichia coli, Candida albicans, and C parapsilosis. Patient 15 was infected with Bordetella pertussis. Patient 6 had significant infection with Streptococcus spp. No patient had fungal infection. Viral infections predating transplantation were present in 6 cases (2 CMV, 2 parainfluenza, 1 rotavirus, 1 echovirus). Only 2 of these survived in the long-term (one with CMV and one with parainfluenza), although the viruses were not always the main cause of death. One case (patient 5) developed CMV infection after transplantation with fatal outcome, 2 developed Epstein-Barr virus infection (1 survived), and 1 developed human herpesvirus 6 (died).
Adverse events
Only 2 patients experienced no significant adverse events. Patient 1 experienced transitory marrow suppression, and mild arthritis and cellulitis were seen in patient 2. Significant acute GVHD (grades 2-4) occurred in 9 patients, in 4 the condition became chronic, and in 2 it was associated with death. Circulatory instability contributed to death in 3 patients, related to cardiac surgery in 2. Patient 14 died of hypertrophic cardiomyopathy and pneumopathy associated with suspected pulmonary GVHD. Patient 15 died with biopsy-proven pulmonary veno-occlusive disease, associated with acute renal failure.
Outcome
Median follow-up was 13 months (range, 2 months to 11.5 years). Seven patients (41%) are alive and well with a median follow-up of 5 years, 10 months (range, 4-11.5 years). The 10 deaths (59%) occurred at a median of 7 months after transplantation (range, 2-18 months). In 5 patients, death was the result of cardiorespiratory failure (3 of these deaths occurred in association with cardiac or lung surgery). Two patients died of pneumopathy and chronic GVHD, and 2 of severe viral pneumonitis (CMV, parainfluenza). One patient died unexpectedly at home of unknown cause.
Comparison of survivors and nonsurvivors is shown (Table 4). Absence of conditioning and graft from matched sibling donor were the only parameters significantly associated with survival. There were no differences in incidence of severe posttransplantation infections or GVHD between patients receiving marrow or PBL.
Association of different parameters and outcome (n = 17)
| Parameter/category . | n . | Outcome . | ||
|---|---|---|---|---|
| Survivors (n = 7) . | Nonsurvivors (n = 10) . | P . | ||
| Phenotype | ||||
| CHARGE | 7 | 2 | 5 | NS |
| DGS | 10 | 5 | 5 | NS |
| Atypical DGS | 3 | 1 | 2 | NS |
| Gene defect | ||||
| 22q11.2 | 8 | 5 | 3 | NS |
| CHD7 | 4 | 3 | 1 | NS |
| Transplantation regimen | ||||
| GVHD prophylaxis | 11 | 4 | 7 | NS |
| Conditioning | 5 | 0 | 5 | .026 |
| Donor | ||||
| MSD | 7 | 5 | 2 | .034 |
| MRD | 1 | 0 | 1 | NS |
| Haploidentical | 1 | 0 | 1 | NS |
| MUD | 8 | 2 | 6 | NS |
| Graft | ||||
| Marrow | 9 | 3 | 6 | NS |
| Combined (PBL, then marrow) | 2 | 2 | 0 | NS |
| PBL | 5 | 2 | 3 | NS |
| Cord | 1 | 0 | 1 | NS |
| B cell–depleted PBL | 1 | 0 | 1 | NS |
| T cell–depleted marrow | 1 | 0 | 1 | NS |
| Age at transplantation | ||||
| Less than or equal to 3 months | 7 | 3 | 4 | NS |
| Median | 17 | 5 | 4.5 | NS |
| Immune reconstitution | ||||
| T cells/mm3 (median at the last follow-up) | 15 | 806 (5 patients) | 480 (10 patients) | NS |
| Complications | ||||
| GVHD (grade ≥ 2) | 9 | 3 | 6 | NS |
| Parameter/category . | n . | Outcome . | ||
|---|---|---|---|---|
| Survivors (n = 7) . | Nonsurvivors (n = 10) . | P . | ||
| Phenotype | ||||
| CHARGE | 7 | 2 | 5 | NS |
| DGS | 10 | 5 | 5 | NS |
| Atypical DGS | 3 | 1 | 2 | NS |
| Gene defect | ||||
| 22q11.2 | 8 | 5 | 3 | NS |
| CHD7 | 4 | 3 | 1 | NS |
| Transplantation regimen | ||||
| GVHD prophylaxis | 11 | 4 | 7 | NS |
| Conditioning | 5 | 0 | 5 | .026 |
| Donor | ||||
| MSD | 7 | 5 | 2 | .034 |
| MRD | 1 | 0 | 1 | NS |
| Haploidentical | 1 | 0 | 1 | NS |
| MUD | 8 | 2 | 6 | NS |
| Graft | ||||
| Marrow | 9 | 3 | 6 | NS |
| Combined (PBL, then marrow) | 2 | 2 | 0 | NS |
| PBL | 5 | 2 | 3 | NS |
| Cord | 1 | 0 | 1 | NS |
| B cell–depleted PBL | 1 | 0 | 1 | NS |
| T cell–depleted marrow | 1 | 0 | 1 | NS |
| Age at transplantation | ||||
| Less than or equal to 3 months | 7 | 3 | 4 | NS |
| Median | 17 | 5 | 4.5 | NS |
| Immune reconstitution | ||||
| T cells/mm3 (median at the last follow-up) | 15 | 806 (5 patients) | 480 (10 patients) | NS |
| Complications | ||||
| GVHD (grade ≥ 2) | 9 | 3 | 6 | NS |
DGS indicates DiGeorge syndrome; CHD, chromodomain helicase; MRD, matched related donor; MUD, matched unrelated donor; MSD, matched sibling donor; GVHD, graft-versus-host disease; PBL, peripheral blood lymphocyte; OBL, peripheral lymphocyte; and NS, statistically not significant.
Immune reconstitution data in those long-term survivors with evaluable data (5 patients) show the median (range) number of T lymphocytes measured at last follow-up of 806 cells/mm3 (644-1224 cells/mm3) and for CD4 counts 348 cells/mm3 (225-782 cells/mm3). No difference in these numbers was seen between those receiving PBLs or marrow, although numbers are very small. All of 6 survivors tested have normal or only mildly decreased PHA responses, and one of 7 has significant numbers of naive CD4 T cells. Five of 7 survivors no longer receive replacement immunoglobulin, 5 have received vaccinations, and of these 4 responded to tetanus toxoid, 3 to Haemophilus influenzae type B antigen, and 2 to Streptococcus pneumoniae antigens. Patient 12 was shown to have a proliferative response to tetanus toxoid but remains on immunoglobulin replacement.
Discussion
The data presented here represent the largest cohort of patients with cDGA phenotype treated with HCT for severe immunodeficiency. With a further 9 patients reported in the literature7,9,12,13,21,22 (supplemental Table 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article), details of 26 transplanted patients are available.
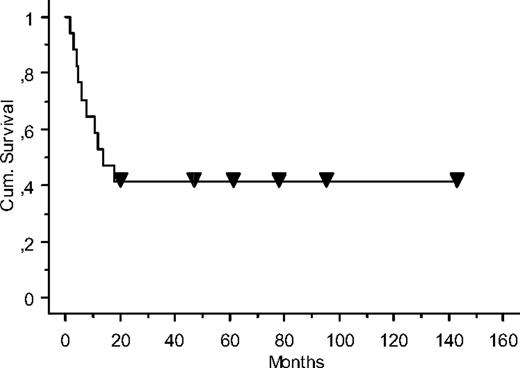
The overall survival (Figure 1) in the survey cohort was 41% with median follow-up of almost 6 years. If the previously published patients are also included, the survival increases to 50% with median follow-up of 8.5 years (range, 4-24 years). This mortality rate is probably skewed by the fact that infants with DGA have multisystem problems associated with the underlying disorder; 5 patients died of such complications, generally associated with cardiorespiratory failure. Four patients died of complications related to GVHD or engraftment pneumonitis (15%), 2 patients died of severe infection, and in 2 patients the cause of death is unknown. The incidence of GVHD was similar to other published series of HCT for SCID23,24 ; 6 of 17 (35%) in this series had acute GVHD of gut, liver, or lung grade 2 to 4, and a further 2 had grade 2 skin acute GVHD. Fifteen percent had chronic GVHD. However, there is an impression that GVHD in cDGA patients is more severe, or chronic than expected, given that most have had no chemotherapeutic cytoreduction before transplantation, and that the majority of donors are well matched. There are a number of possible reasons for this. First, the underlying condition may predispose to chronically inflamed tissue acting as a substrate for GVHD, for instance, lung inflammation secondary to gastroesophageal reflux and pulmonary aspiration. Second, an absence of thymus-derived regulatory T cells may predispose to prolonged and severe GVHD. Third, the reaction could be related to homeostatic expansion of donor T cells as no new T lymphopoiesis takes place in complete athymic DGA or CHARGE syndrome. Given this increased risk of severe or chronic GVHD, all patients should receive appropriate prophylaxis, including those with HLA-identical matches, and this should be cautiously discontinued, as preexisting inflammation resolves.
The failure of new lymphopoiesis may also explain the poor outcome of patients presenting with preexisting viral infection, with only 2 of 6 surviving, compared with an overall survival of 59% for patients with severe combined immunodeficiency, even after haplo-identical transplantation, in the European series.25 Given that there will be no thymopoiesis and that B lymphocytes from DiGeorge/CHARGE patients have potentially normal function, there is no advantage to engraftment of stem cell progenitors, and so conditioning is not necessary in the majority of cases; indeed, conditioning was associated with a significantly higher mortality in this series. The exceptions may be those patients with atypical cDGA or maternal T lymphocyte engraftment, in whom some form of anti-T lymphocyte serotherapy may be required before transplantation.
Although the use of marrow or PBL as source of T cells did not affect the outcome, use of PBL is more rational as adoptive transfer of mature T cells is the key principle of this procedure. Certainly, administration of T cell–depleted marrow should be strongly discouraged. On the other hand, use of matched sibling donor transplantations had a significantly better outcome than unrelated donor and cord blood transplantations. In the combined survey/published data, survival after unrelated donor PBL or marrow transplantations was only 3 of 9 and for unrelated donor cord blood was 1 of 3. Combining survey data on matched sibling donors with the literature gives an overall survival of 8 of 13 (62%). Because immune reconstitution in this condition depends on engraftment of long-lived postthymic memory T cells the choice of cord blood may not be ideal because of the antigenic naivete of the donor.
Most patients who survived long-term remain clinically well/stable without frequent infections, although 2 in the literature survey were reported as having recurrent severe infections (patients 19 and 26).9,21,22 Humoral immune function in survivors is good, with only 2 of 7 of the survivors in the survey group requiring immunoglobulin treatment (data not available from the literature group) and good antibody responses to protein or conjugate vaccines when tested. No data were available on polysaccharide antibody responses. Information on T cell-mediated immune function was not complete; where tested, there were relatively low numbers of CD3+ and CD4+ cells in most cases, an absence of naive T cells, and skewed T lymphocyte receptor repertoire. Long-term follow-up data from a recent large series of patients with other forms of SCID who have undergone HCT suggest that patients with low CD4 counts (present in all but one of the evaluable survivors in the present series) but not naive CD4 cells were significantly more probable to have complications, including infections, autoimmune inflammatory complications, and nutritional problems, than those with normal counts.26 This suggests that these patients may remain at risk of late complications, particularly if cell numbers decline with time.
One patient who had late unexplained death (patient 3) did produce significant numbers of CD4+CD45RA+ cells. It is not clear whether these were true thymic emigrants as neither TRECs analysis nor CD45RA/CD62L analysis was available. If these were true thymic emigrants, then it suggests that the patient did not have a truly complete form of DGA as suggested by the authors in a published report of this case.8
Recent experience of transplantation of cultured thymic epithelium in patients with cDGA has shown promising results, with good immune reconstitution, including normal T-cell receptor repertoire diversity and the ongoing presence of recent thymic emigrants.2 GVHD was not seen. Survival with a median follow-up period of 3 years and 10 months was 75%. Most deaths were associated with chronic lung disease or viral infections, both predating the transplantation. Approximately one-third of the survivors developed autoimmune disease, mostly affecting the thyroid gland. It has been pointed out that patient selection in this study meant that those patients with the most severe comorbidities were not offered the therapy.17 Nevertheless, the results compare favorably with the outcome from our survey both in terms of survival and quality of immune reconstitution. Currently, thymic transplantation requires specialized facilities for thymus culture and is only available in 2 centers in the world, thus limiting its availability.
Although the data collected in this retrospective study are incomplete, and the numbers of cases in subcategories small, some tentative conclusions can be drawn. Where a well-matched sibling donor is available, infusion of peripheral lymphocytes can be considered without preconditioning, and early before end-stage organ damage occurs or worsens. Prophylactic GVHD treatment should be given, and cautiously withdrawn as any preexisting inflammation resolves. However, in a relatively well child without any infections, the survival after thymic transplantation is at least as good (75% vs 62%, although the patients were preselected) and immune reconstitution superior. Thus, for other patients, the feasibility of thymic transplantation should be considered.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Prof Louise Markert for invaluable help in identifying some patients and the patients and their parents for allowing us to care for them as well as learn from them.
This work was supported in part by the Czech Ministry of Education (grant VZ MSM CR 21620812) and the Czech Ministry of Health (grant MZOFNM2005).
Authorship
Contribution: A.J. and A.R.G. designed the study, prepared and collected data through a questionnaire, analyzed data, and wrote the paper; M.A.S. and E.G.D. reported on their patients and significantly contributed to the data analysis and the final version of the paper; and P.S., M.H., W.F., M.C., T.M., A.F., B.N., A.C., D.B., P.B., D.L., W.S., N.J. and F.A.B. collected data and participated in the manuscript's preparation.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ales Janda, Department of Pediatric Hematology and Oncology, University Hospital Motol and 2nd Medical School, Charles University, Prague, Czech Republic; e-mail: ales.janda@lfmotol.cuni.cz.