Abstract
The PROLONG randomized trial showed that a normal D-dimer (D-d) 1 month after anticoagulation suspension for unprovoked venous thromboembolism (VTE) was associated with a low risk of late recurrences (4.4% patient years). However, it is unknown whether D-d changes subsequently. The aim of this prospective multicenter study was to assess D-d time course and its relation with late recurrences in patients with normal D-d 1 month after anticoagulation suspension for a first episode of unprovoked VTE. D-d was measured with a qualitative method (Clearview Simplify D-dimer; Inverness Medical Professional Diagnostics). Patients with a normal D-d 1 month after stopping anticoagulation repeated D-d testing every 2 months for 1 year. D-d was normal in 68% (243/355) of patients 1 month after anticoagulation suspension. Patients in whom D-d became abnormal at the third month and remained abnormal afterward had a higher risk of recurrence (7/31; 27% patient years; 95% confidence interval [CI]: 12-48) than patients in whom D-d remained normal at the third month and afterward (4/149; 2.9% patient years; 95% CI: 1-7; adjusted hazard ratio: 7.9; 95% CI: 2.1-30; P = .002). Repeated D-d testing after anticoagulation suspension for a first episode of unprovoked VTE could help tailor the duration of treatment. This trial is registered at http://clinicaltrials.gov as NCT00266045.
Introduction
The optimal duration of anticoagulation after a first episode of unprovoked venous thromboembolism (VTE) is still unknown.1-3 Recently, the American College of Chest Physicians recommended that patients with unprovoked VTE should receive at least 3 months of anticoagulant therapy and then subjects should be evaluated for the risk-benefit ratio of long-term therapy.4 Long-term treatment is recommended in those in whom risk factors for bleeding are absent and for whom good anticoagulant monitoring is achievable. In this recommendation, a relatively high value is attached to prevention of recurrent VTE and a lower value to the burden of long-term anticoagulant therapy. However, the decision about treatment is ultimately left to the physicians' subjective evaluation of the risk-benefit ratio in each patient and to patients' preferences about treatment prolongation. The risk of recurrence is greatest in the first 6 to 12 months after the initial episode, while it gradually decreases thereafter.5 As a result, the benefits of extending anticoagulation may be offset over time by the risk of clinically important bleeding associated with vitamin K antagonists (VKAs).1-3,6,7 The identification of patient characteristics predictive of recurrence would be a valuable aid in the decision about stopping or prolonging VKAs after a first episode of unprovoked VTE.
The multicenter randomized study PROLONG showed that D-dimer (D-d) could play a role in establishing the duration of anticoagulation after a first episode of idiopathic VTE. Patients were treated with VKAs for a minimum of 3 months and D-d was tested 1 month after anticoagulation withdrawal.8 If D-d was normal patients did not resume treatment, whereas those with elevated D-d were randomized to either stop or resume VKAs. Patients with an abnormal D-d had a statistically significant higher risk for recurrence compared with those with normal D-d. Continued anticoagulation in patients with elevated D-d significantly reduced the risk of recurrent VTE over an extended follow-up of 2.55 years.9 In subjects with normal D-d the rate of VTE recurrence was 4.4% patient-years (pt-y), which is higher than the expected annual rate of major bleeding (2% pt-y) with VKAs.6 As a result, the optimal duration of treatment is an unresolved issue in these patients. In the PROLONG study only a single D-d measurement was performed after stopping anticoagulation and it is unknown whether and how often D-d becomes abnormal afterward and whether a late hypercoagulability is associated with the risk of recurrences.
To address these questions, we conducted the observational multicenter prospective PROLONG II study. In this study, D-d was tested serially over 1 year in subjects with normal D-d 1 month after anticoagulation suspension for a first episode of unprovoked VTE with the aim of assessing the times and frequency of D-d becoming abnormal and its relation with recurrent VTE.
Methods
Study patients
The PROLONG II study was a prospective cohort study in patients aged 18 to 82 years with a first episode of objectively documented symptomatic idiopathic VTE, either proximal lower extremity deep vein thrombosis (DVT) and/or pulmonary embolism (PE). DVT was to be detected by compression ultrasonography or venography, and PE to be diagnosed on the basis of objective algorithms using clinical probability, ventilation-perfusion or helical computed tomography lung scan, compression ultrasonography (if indicated), and D-dimer testing. Patients were eligible for the study if they had completed at least 6 months of VKA therapy (either warfarin [Coumadin; Bristol Myers Squibb] or acenocoumarol [Sintrom; Novartis Pharma]) with a target International Normalized Ratio (INR) of 2.5 (range 2.0-3.0).
Unprovoked VTE was defined as an episode not associated with pregnancy or the puerperium, recent (ie, within 3 months) fracture or plaster casting of a leg, immobilization with confinement to bed for at least 3 consecutive days, surgery with general anesthesia lasting at least 30 minutes, active malignancy, antiphospholipid antibody syndrome, or antithrombin deficiency. Exclusion criteria were serious liver disease, renal insufficiency (plasma creatinine > 2 mg/dL), active cancer or undergoing chemotherapy and/or radiotherapy, other indications for anticoagulation or contraindications for such treatment, limited life expectancy, or geographical inaccessibility. The ethics committees of all participating clinical centers approved the study. All enrolled patients provided written informed consent in accordance with the Declaration of Helsinki.
Study procedures
At the end of the intended anticoagulation period (T0), subjects were assessed for eligibility and baseline clinical conditions. The presence of known comorbidities such as coronary heart disease, peripheral arterial disease, cerebrovascular disease, chronic intestinal inflammatory diseases, chronic pulmonary obstructive disease, autoimmune disease, diabetes, arterial hypertension, obesity, and dyslipidemias was collected on a standardized form. Patients underwent compression ultrasonography (CUS) of the proximal deep veins in both legs to measure the diameter of any residual venous obstruction (RVO) in the common femoral, superficial femoral, and popliteal veins.10 Patients then underwent blood sampling for INR. If the INR was in the therapeutic range (INR: 1.8-3.2), D-d was also measured using the Clearview Simplify D-dimer assay (Inverness Medical Professional Diagnostics; kindly provided by the Instrumentation Laboratory Co). This is a qualitative, fast, whole-blood method, previously shown to perform well in VTE diagnosis with good reproducibility.11 The test itself is a standard immunochromatographic test in which the D-d–specific murine monoclonal antibody DD3B6/223 is conjugated to colloidal gold particles. It is performed by mixing 35 μL of capillary or venous blood with 2 drops of test reagent. A positive test result occurs when D-d levels exceed 80 ng/mL (as measured by an enzyme-linked immunosorbent assay [ELISA] method, DIMERTEST GOLD EIA) and is indicated by a visible pink-purple colored line that forms at the test zone. Test results are valid if a pink-purple line is also present at the control zone. The test can be read within 10 minutes.
Patients with abnormal D-d continued VKAs and they were scheduled for a reassessment of D-d after 6 months. Patients with a normal D-d were instructed to stop oral anticoagulation on the same day and refrain from taking any other antithrombotic drugs until the next visit, scheduled after 30 (± 10) days (T30).
At the 30-day visit, venous blood was sampled for D-d assay and thrombophilia tests. Patients with abnormal D-d results resumed anticoagulation with VKAs (INR 2.0-3.0).
Patients with a normal D-d test did not resume anticoagulation and underwent bimonthly D-d testing (± 10 days) over 1 year at the third (T90), fifth (T150), seventh (T210), ninth (T270), eleventh (T330), and thirteenth (T390) months.
Testing for lupus anticoagulant phenomenon and/or antiphospholipid antibodies and antithrombin, protein C and protein S activities, factor V Leiden, and the G20210A mutation in the prothrombin gene was performed at the enrolling centers, as reported before.12 Subjects found to have antiphospholipid syndrome or antithrombin deficiency were excluded from further analysis and resumed anticoagulation.
Follow-up and study outcomes
All patients with a normal D-d were followed for a maximum duration of 13 months from the assignment visit and were seen at the clinical center every 2 months over 1 year when D-d testing was repeated for a maximum of 6 times.
D-d testing was avoided and rescheduled after 30 days in case of recent trauma, surgery, or other conditions that could have influenced the results.
Patients were instructed to contact the clinical center immediately if symptoms developed suggestive of VTE or in case of bleeding.
All subjects who continued VKAs for an altered D-d during anticoagulation or who resumed VKAs for an altered D-d at 1 month after stopping anticoagulation were scheduled for a reassessment of D-d after at least 3 to 6 months.
The main study outcome was confirmed recurrent VTE in subjects who stopped anticoagulation for a normal D-d 1 month after VKA withdrawal. The secondary outcome was the composite of major bleeding and recurrent VTE in those who continued or resumed VKAs for abnormal D-d.
In cases of suspected DVT recurrence, the results of CUS were compared with those of the last available previous examination. A recurrent DVT was diagnosed if a previously fully compressible segment (contralateral or ipsilateral) was no longer compressible or if an increase of at least 4 mm in the diameter of the residual thrombus during compression was detected.10 When thrombus diameter changed between 1.1 mm and 3.9 mm, or in cases of high/moderate clinical probability and normal proximal compression ultrasonography, the examination was repeated 5 to 7 days later.
In patients with suspected PE, diagnosis of recurrence was based on objective algorithms13,14 using clinical probability, ventilation-perfusion lung scanning or helical computed tomography, compression ultrasonography, and/or D-d if indicated.
Major bleeding events were defined as bleeds that were retroperitoneal or intracranial, or associated with a decrease in the hemoglobin of at least 2.0 g/dL, or required transfusion of at least 2 units of blood, or if surgery or invasive procedures were necessary to stop bleeding.6
All suspected outcome events and all deaths were evaluated by a central adjudication committee whose members were unaware of the name of the subject, the enrolling center, the results of D-d, thrombophilia assays, INRs, and VKA treatment. All clinical investigation results were also reviewed by the committee members without any indication of the name of the subject, the assigned group, or the city/institution where the testing had been performed.
Statistical analysis
Baseline differences between groups were assessed by the χ2 test (Yates correction) or Fisher exact test for categorical variables and t test or Mann-Whitney U test for continuous variables, as appropriate.
Patients with a normal D-d 1 month (T30) after stopping anticoagulation were evaluated according to the D-d result at each subsequent time point (T90, T150, T210, T270, T330, T390) and were divided into 4 groups: (1) patients in whom D-d was normal, being also normal at the previous time point; (2) patients in whom D-d became newly abnormal, being normal at the previous time point; (3) patients in whom D-d was abnormal, being also abnormal at the previous time point; (4) patients in whom D-d became normal, being abnormal at the previous time point. At each time point the rate of recurrence was calculated over the next 2 months.
Patients with a normal D-d 1 month after stopping anticoagulation were also divided into 3 subgroups according to D-d subsequent time course: (1) patients in whom D-d remained normal at T90 and afterward (with D-d becoming abnormal only once); (2) patients in whom D-d became abnormal at T90 and remained abnormal persistently or at least twice; and (3) patients in whom D-d became abnormal after T90 and remained abnormal persistently or at least twice.
Kaplan-Meier survival curves were plotted to estimate the cumulative incidence of symptomatic recurrent VTE. Hazard ratios and their 95% confidence intervals were calculated using the Cox proportional hazards model. Initially, an unadjusted hazard ratio was calculated with age, sex, duration of anticoagulation, DVT versus DVT and/or PE as the index event, presence/absence of comorbidities, presence/absence of thrombophilia, presence/absence of RVO. Then a multivariate model was constructed, introducing only those variables with a P < .2 at the univariate analysis.
The data were analyzed using the Prism statistical software package (Version 3.0; GraphPad Software Inc) and the SPSS statistical package (Version 11.0; SPSS Inc).
Results
Patients
A total of 355 patients were enrolled in 15 clinical centers between March 1, 2005, and February 2, 2008.
The flow chart of the study from T0 to T30 is shown in Figure 1. During anticoagulation, D-d was abnormal in 19 subjects (5.3%; 95% CI: 3%-8%) in whom VKAs were continued, whereas D-d was normal in the remaining 336 patients and they stopped VKAs. At T30, D-d was abnormal in 85 of 328 patients (26%; 95% CI: 21%-31%), and these patients resumed VKAs.
The baseline characteristics of the patients are reported in Table 1. Patients (n = 104) who prolonged or resumed VKA for an abnormal D-d either at T0 or at T30 were significantly older, had more comorbidities and had a longer follow-up than patients who stopped VKAs for a normal D-d at both T0 and T30 (n = 243).
Baseline characteristics of the enrolled patients
| . | Patients, N = 355 . | D-d normal at T0 or at T30, N = 243 . | D-d abnormal at T0 or at T30, N = 104 . | P* . |
|---|---|---|---|---|
| Female sex, n (%) | 162 (45.6) | 107 (44) | 53 (51) | .28 |
| Age | ||||
| Mean ± 95% CI, y | 62 + 1.2 | 59 + 2 | 69 + 2 | < .001 |
| 65 y or older, n (%) | 195 (55) | 108 (44.4) | 78 (75) | < .001 |
| Type of venous thromboembolism, n (%) | ||||
| Proximal DVT; no PE | 236 (66.5) | 155 (63.7) | 73 (70.2) | .22 |
| DVT + symptomatic PE | 43 (12.1) | 30 (12.3) | 13 (12.5) | .97 |
| Isolated PE | 76 (21.4) | 58 (23.8) | 18 (17.3) | .22 |
| Comorbidities | 155 (43.7) | 97 (39.9) | 57 (54.8) | .014 |
| Residual venous thrombosis, n (%) | 124 (35) | 84 (40.2) | 42 (44.2) | .59 |
| (no. CUS available, %) | (302; 85) | (209; 86) | (95; 91.3) | |
| Congenital thrombophilic alteration, n (%) | ||||
| Examined, n (%) | 273 (77) | 206 (84.8) | 67 (64.4) | |
| All | 132 (48.3) | 97 (47.1) | 36 (53.7) | .42 |
| Prot C, S, AT deficiencies, LAC | 5 (1.8) | 2 (1.0) | 3 (4.4) | .18 |
| Hyperhomocysteinemia | 60 (22) | 43 (20.1) | 18 (26.8) | .39 |
| FV Leiden | 33 (12) | 25 (12.3) | 8 (11.9) | .96 |
| Prothrombin mutation | 20 (7.3) | 16 (7.7) | 4 (6.0) | .82 |
| Combined alterations and/or homozygous | 14 (5.1) | 11 (5.3) | 3 (4.5) | .78 |
| Duration of previous anticoagulant treatment, n (%) | ||||
| Less than 6 months, n (%) | 77 (21.6) | 54 (22.2) | 21 (20.2) | .78 |
| 7 to 12 months, n (%) | 164 (46.2) | 110 (45.2) | 49 (47.1) | .84 |
| More than 12 months, n (%) | 114 (32.1) | 79 (32.5) | 34 (32.7) | .97 |
| Total duration of follow-up, patient y | 365 | 212 | 153 | < .001 |
| Follow-up, mean ± 95% CI, mo | 10.6 ± 0.2 | 18 ± 16 |
| . | Patients, N = 355 . | D-d normal at T0 or at T30, N = 243 . | D-d abnormal at T0 or at T30, N = 104 . | P* . |
|---|---|---|---|---|
| Female sex, n (%) | 162 (45.6) | 107 (44) | 53 (51) | .28 |
| Age | ||||
| Mean ± 95% CI, y | 62 + 1.2 | 59 + 2 | 69 + 2 | < .001 |
| 65 y or older, n (%) | 195 (55) | 108 (44.4) | 78 (75) | < .001 |
| Type of venous thromboembolism, n (%) | ||||
| Proximal DVT; no PE | 236 (66.5) | 155 (63.7) | 73 (70.2) | .22 |
| DVT + symptomatic PE | 43 (12.1) | 30 (12.3) | 13 (12.5) | .97 |
| Isolated PE | 76 (21.4) | 58 (23.8) | 18 (17.3) | .22 |
| Comorbidities | 155 (43.7) | 97 (39.9) | 57 (54.8) | .014 |
| Residual venous thrombosis, n (%) | 124 (35) | 84 (40.2) | 42 (44.2) | .59 |
| (no. CUS available, %) | (302; 85) | (209; 86) | (95; 91.3) | |
| Congenital thrombophilic alteration, n (%) | ||||
| Examined, n (%) | 273 (77) | 206 (84.8) | 67 (64.4) | |
| All | 132 (48.3) | 97 (47.1) | 36 (53.7) | .42 |
| Prot C, S, AT deficiencies, LAC | 5 (1.8) | 2 (1.0) | 3 (4.4) | .18 |
| Hyperhomocysteinemia | 60 (22) | 43 (20.1) | 18 (26.8) | .39 |
| FV Leiden | 33 (12) | 25 (12.3) | 8 (11.9) | .96 |
| Prothrombin mutation | 20 (7.3) | 16 (7.7) | 4 (6.0) | .82 |
| Combined alterations and/or homozygous | 14 (5.1) | 11 (5.3) | 3 (4.5) | .78 |
| Duration of previous anticoagulant treatment, n (%) | ||||
| Less than 6 months, n (%) | 77 (21.6) | 54 (22.2) | 21 (20.2) | .78 |
| 7 to 12 months, n (%) | 164 (46.2) | 110 (45.2) | 49 (47.1) | .84 |
| More than 12 months, n (%) | 114 (32.1) | 79 (32.5) | 34 (32.7) | .97 |
| Total duration of follow-up, patient y | 365 | 212 | 153 | < .001 |
| Follow-up, mean ± 95% CI, mo | 10.6 ± 0.2 | 18 ± 16 |
D-d denotes D-dimer; VKA, vitamin K antagonist treatment; FV Leiden, factor V Leiden mutation; DVT, deep vein thrombosis; PE, pulmonary embolism; AT, antithrombin; LAC, lupus anticoagulant; and CUS, compression ultrasonography.
P value refers to χ2 or Fisher exact test or t test, as appropriate, between normal D-d and abnormal D-d.
Follow-up and recurrent venous thromboembolism
Recurrences before T30 were observed in 2 patients who stopped VKA for a normal D-d at T0 (0.59%; 95% CI: 0%-2%). Among the 243 patients with a normal D-d at T30 who maintained VKA suspension, 8 early recurrences (3.3%; 95% CI: 1%-6%) were observed before D-d was determined at T90.
Total follow-up after T30 in patients with normal D-d was 212 patient-years, mean follow-up was 10.6 months (range 1-13 months), and 79% of patients (192/243) had a follow-up of at least 7 months.
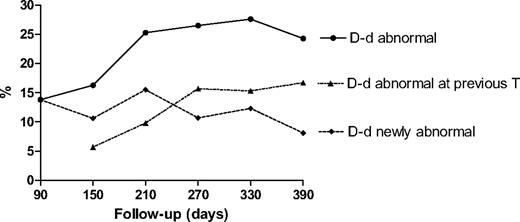
Figure 2 shows the rate of conversion from D-d normal to abnormal from T90 to T390. After T90, the rate of newly abnormal D-d remained stable (approximately 10%-15%) up to T270. Afterward, the rate of newly abnormal D-d decreased to 8%-10%.
Frequency of conversion from D-dimer (D-d) normal to abnormal from the third month (T90) to the 13th month (T390).
Frequency of conversion from D-dimer (D-d) normal to abnormal from the third month (T90) to the 13th month (T390).
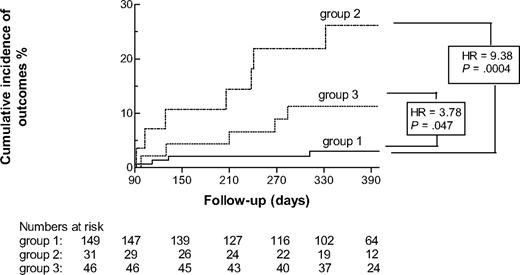
Cumulative incidence and hazard ratios (HRs) of main outcomes according to D-d time course from the third month (T90) to the 13th month (T390). Group 1: Patients in whom D-d was normal at T90 and afterward (with D-d becoming abnormal only once). Group 2: Patients in whom D-d became abnormal at T90 and afterward remained altered persistently or at least twice. Group 3: Patients in whom D-d became abnormal after T90 and afterward remained abnormal persistently or at least twice.
Cumulative incidence and hazard ratios (HRs) of main outcomes according to D-d time course from the third month (T90) to the 13th month (T390). Group 1: Patients in whom D-d was normal at T90 and afterward (with D-d becoming abnormal only once). Group 2: Patients in whom D-d became abnormal at T90 and afterward remained altered persistently or at least twice. Group 3: Patients in whom D-d became abnormal after T90 and afterward remained abnormal persistently or at least twice.
Table 2 illustrates study follow-up from T90 to T390. The rate of recurrence was 22.6% (7/31; 95% CI: 10%-41%) in those subjects in whom D-d was abnormal at T90 and 4.6% (9/195; 95% CI: 2%-9%) in patients in whom D-d was normal at T90 (P = .003). Recurrence rates were significantly higher in males than in females (15/136: 11%; 95% CI: 6%-18% vs 1/107: 1%; 95% CI: 0%-5%; P = .001), while a trend for higher recurrences was observed in subjects with than in those without comorbidities (10/89: 11.3%; 95% CI: 6%-20% vs 6/136: 4.4%; 95% CI: 2%-9%; P = .06).
D-d time course from T90 to T390 and recurrences observed in the two months between each D-d measurement
| Time points . | Patients, N (D-d not one) . | D-d . | D-d normal also at previous T . | D-d newly abnormal . | D-d abnormal also at previous T . | D-d normal but altered at previous T . | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal (%) . | Abnormal (%) . | No. of patients . | rVTE (%) . | No. of patients (%) . | rVTE (%) . | No. of patients . | rVTE (%) . | No. of patients . | rVTE (%) . | ||
| T90 | 228 (3) | 194 | 4 (2.1) | 31 (13.8) | 3 (9.7)* | ||||||
| 3 DVTs, 1 PE | 2 DVTs, 1 PE | ||||||||||
| 2 patients resumed | 2 patients withdrew | ||||||||||
| VKAs for SVT | |||||||||||
| T150 | 209 (1) | 174 | 34 (16.3) | 162 | 0 (0) | 22 (10.6) | 1 (4.5)† | 12 | 0 | 12 | 1 (8.3)‡ |
| 2 patients withdrew | 1 DVT | 1 DVT | |||||||||
| T210 | 193 | 144 | 49 (25.3) | 132 | 0 (0) | 30 (15.5) | 1 (3.3)§ | 19 | 2 (10.5)∥ | 12 | 0 |
| 1 DVT | 2 DVTs | ||||||||||
| T270 | 178 (1) | 130 | 47 (26.5) | 115 | 0 (0) | 19 (10.7) | 0 | 28 | 3 | 15 | 0 |
| 1 patient resumed | (10.7)¶ | ||||||||||
| VKAs for afib | 3 DVTs | ||||||||||
| T330 | 163 (4) | 114 | 45 (28.3) | 97 | 1 (1) | 20 (12.5) | 0 | 25 | 0 | 17 | 0 |
| 1 DVT | |||||||||||
| T390 | 144 (9) | 100 | 35 (26) | 84 | 0 (0) | 11 (8.1) | 0 | 24 | 0 | 16 | 0 |
| Time points . | Patients, N (D-d not one) . | D-d . | D-d normal also at previous T . | D-d newly abnormal . | D-d abnormal also at previous T . | D-d normal but altered at previous T . | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal (%) . | Abnormal (%) . | No. of patients . | rVTE (%) . | No. of patients (%) . | rVTE (%) . | No. of patients . | rVTE (%) . | No. of patients . | rVTE (%) . | ||
| T90 | 228 (3) | 194 | 4 (2.1) | 31 (13.8) | 3 (9.7)* | ||||||
| 3 DVTs, 1 PE | 2 DVTs, 1 PE | ||||||||||
| 2 patients resumed | 2 patients withdrew | ||||||||||
| VKAs for SVT | |||||||||||
| T150 | 209 (1) | 174 | 34 (16.3) | 162 | 0 (0) | 22 (10.6) | 1 (4.5)† | 12 | 0 | 12 | 1 (8.3)‡ |
| 2 patients withdrew | 1 DVT | 1 DVT | |||||||||
| T210 | 193 | 144 | 49 (25.3) | 132 | 0 (0) | 30 (15.5) | 1 (3.3)§ | 19 | 2 (10.5)∥ | 12 | 0 |
| 1 DVT | 2 DVTs | ||||||||||
| T270 | 178 (1) | 130 | 47 (26.5) | 115 | 0 (0) | 19 (10.7) | 0 | 28 | 3 | 15 | 0 |
| 1 patient resumed | (10.7)¶ | ||||||||||
| VKAs for afib | 3 DVTs | ||||||||||
| T330 | 163 (4) | 114 | 45 (28.3) | 97 | 1 (1) | 20 (12.5) | 0 | 25 | 0 | 17 | 0 |
| 1 DVT | |||||||||||
| T390 | 144 (9) | 100 | 35 (26) | 84 | 0 (0) | 11 (8.1) | 0 | 24 | 0 | 16 | 0 |
rVTE indicates recurrent venous thromboembolism; SVT, superficial vein thrombosis; and afib, atrial fibrillation.
P = .05 vs D-d normal also previously.
P = .11 vs D-d normal also previously.
P = .07 vs D-d normal also previously.
P = .18 vs D-d normal also previously.
P = .015 vs D-d normal also previously.
P = .007 vs D-d normal also previously.
Table 2 also shows the events observed in the 2 months between each measurement according to D-d results at each time point. At T90, newly abnormal D-d was associated with a significantly higher rate of recurrence compared with normal D-d. At T210 and at T270, the rate of recurrence was significantly higher in those subjects in whom D-d was abnormal also previously compared with persistently normal D-d.
Table 3 shows the recurrence rate according to D-d time course from T90. All recurrent events were idiopathic except 1 event secondary to trauma in a subject with a normal D-d at T90. The rate of recurrence was significantly higher in subjects in whom D-d became abnormal at T90 and remained abnormal afterward than in subjects in whom D-d was normal at T90 and remained normal afterward (P = .001). However, the rate of recurrence was also significantly higher in subjects in whom D-d became abnormal after T90 than in subjects in whom D-d was normal at T90 and remained normal afterward (P = .035).
Recurrent VTE according to D-dimer time course from the third month
| Outcomes . | Normal D-d at T90* . | Abnormal D-d at T90† . | Abnormal D-d after T90‡ . |
|---|---|---|---|
| N (%, 95% CI) | 149 (66, 59-72) | 31 (14, 10-19) | 46 (20.3, 15-26) |
| n (%, 95% CI) | 4 (2.7, 1-7) | 7 (22.6, 10-41)§ | 5 (10.9, 4-24)∥ |
| n/100 person, y (95% CI) | 2.9 (1-7) | 27 (12-48) | 11.1 (4-24) |
| Patient years | 138 | 25.6 | 45 |
| Type of recurrent VTE¶ | |||
| DVT | 4 | 6 | 4 |
| DVT + PE | 0 | 0 | 0 |
| Isolated PE | 0 | 1 | 1 |
| Outcomes . | Normal D-d at T90* . | Abnormal D-d at T90† . | Abnormal D-d after T90‡ . |
|---|---|---|---|
| N (%, 95% CI) | 149 (66, 59-72) | 31 (14, 10-19) | 46 (20.3, 15-26) |
| n (%, 95% CI) | 4 (2.7, 1-7) | 7 (22.6, 10-41)§ | 5 (10.9, 4-24)∥ |
| n/100 person, y (95% CI) | 2.9 (1-7) | 27 (12-48) | 11.1 (4-24) |
| Patient years | 138 | 25.6 | 45 |
| Type of recurrent VTE¶ | |||
| DVT | 4 | 6 | 4 |
| DVT + PE | 0 | 0 | 0 |
| Isolated PE | 0 | 1 | 1 |
D-d indicates D-dimer; VTE, venous thromboembolism; DVT, deep vein thrombosis; and PE, pulmonary embolism.
D-d always normal from T90 but once in 25 patients.
D-d always abnormal from T90 in 14 patients and abnormal at least twice in 17 patients.
D-d always abnormal after T90 in 23 patients and abnormal at least twice in 23 patients.
P = .001 vs normal D-d.
P = .035 vs normal D-d.
Seven DVTs occurred in the ipsilateral limb and 7 in the contralateral limb, 1 event was distal DVT, all recurrent events were idiopathic except for 1 DVT secondary to trauma in a patient with normal D-d at T90.
Table 4 shows the hazard ratio for the main outcomes associated with the different subgroups according to D-d time course, while the survival curves associated with the different subgroups are indicated in Figure 3. Covariates such as age, duration of anticoagulation, DVT versus DVT and/or PE as the index event, presence/absence of thrombophilia, presence/absence of RVO had a P value greater than .20 at the univariate analysis and therefore they were not introduced in the multivariate analysis. Only sex (P = .025) and presence/absence of comorbidities (P = .025) had a significant effect and were introduced in the multivariate model.
Hazard ratios for main outcomes
| . | Hazard ratios (95% CI) . | |||
|---|---|---|---|---|
| Unadjusted . | P . | Adjusted* . | P . | |
| D-d normal at T90 | 1 | 1 | ||
| D-d abnormal at T90 | 9.38 (2.75-32.0) | < .001 | 7.90 (2.08-30.0) | .002 |
| D-d abnormal after T90 | 3.78 (1.01-14.1) | .047 | 2.62 (0.68-10.1) | .161 |
| . | Hazard ratios (95% CI) . | |||
|---|---|---|---|---|
| Unadjusted . | P . | Adjusted* . | P . | |
| D-d normal at T90 | 1 | 1 | ||
| D-d abnormal at T90 | 9.38 (2.75-32.0) | < .001 | 7.90 (2.08-30.0) | .002 |
| D-d abnormal after T90 | 3.78 (1.01-14.1) | .047 | 2.62 (0.68-10.1) | .161 |
Adjusted for sex (P = .025 male vs female), and presence vs absence of comorbidities (P = .025).
Subjects with an abnormal D-d at T90 and in the subsequent time points after VKA withdrawal had a significantly higher hazard ratio for recurrence than subjects with a normal D-d at T90 and in the subsequent time points and the difference remained significant after correction. After adjustment, no difference was observed between subjects in whom D-d became abnormal after T90 and patients with a normal D-d at T90.
No significant difference was observed in the conversion of D-dimer from normal to abnormal between subjects with PE (isolated or with DVT; 25/81; 31%) and DVT without PE (51/145; 35%). The risk of recurrence was also similar in subjects with PE (4/81; 5%) and in those without PE (12/145; 8%).
Among the 104 patients in whom VKAs were continued for an abnormal D-d at T0 or at T30, 2 episodes of pulmonary embolism occurred in 2 patients who discontinued VKAs (1 for invasive maneuvers). D-d was retested after an additional VKA course of at least 3 to 6 months in 42 patients, of whom 7 had an altered D-d during treatment and therefore continued VKAs. The remaining 35 patients stopped VKAs for a normal D-d during anticoagulation but 30 (85.7%) resumed VKAs because D-d became abnormal at 1 month after stopping anticoagulation. Among the 5 patients who stopped VKAs, 2 recurrent DVTs were observed (1 after a month and 1 after 10 months).
Major bleeding
Major hemorrhages were recorded in 5 of the 104 patients who either continued or resumed VKAs for an abnormal D-d at T0 or at T30 (3 gastrointestinal hemorrhages, 1 retroperitoneal haematoma, 1 fatal intracranial hemorrhage; 4.8%, 95% CI: 2%-11%; 3.3% pt-y, 95% CI: 1%-7%). In 2 patients, VKAs were discontinued for severe chronic anemia. One patient died due to sepsis.
Discussion
The previously reported PROLONG randomized study showed that patients with a first episode of unprovoked VTE who have an abnormal D-d 1 month after VKA suspension had a higher rate of recurrent VTE (15%; 10.9% pt-y), compared with D-d–positive patients who resumed anticoagulation (combined rate of recurrent VTE and major bleeding of 2.9%; 2.0% pt-y) over a follow-up of 18 months.8 In the patients with a normal D-d who stopped VKAs, the observed rate of recurrence of 6.2% (4.4% pt-y) is clinically relevant, although it was not statistically different from that of patients with abnormal D-d who resumed anticoagulation. The role of D-d in predicting late recurrences was also confirmed by a systematic review of randomized and prospective studies in 1888 patients who had completed at least 3 months of anticoagulation for a first episode of unprovoked VTE and after approximately 2 years of follow-up.15 In the different studies a single D-d test was conducted between 3 weeks and 2 months after stopping VKAs. A negative D-d result was associated with a 3.5% (95% CI: 2.7%-4.3%) annual risk for recurrent disease, whereas a positive D-d result was associated with an 8.9% (95% CI: 5.8%-11.9%) annual risk for recurrence.15
The rate of recurrence in D-d–negative patients is similar to the rate of recurrence observed after a first VTE episode triggered by a transient risk factor, which is usually treated with a short course of anticoagulation.16 However, the recurrence rate in D-d–negative patients might still be considered high enough to warrant prolonging anticoagulation. As a result, the risk/benefit relationship of prolonging anticoagulation in patients with a normal D-d is uncertain, but it is also unknown how often and when an initially single, normal D-d may become abnormal over time. To this purpose, the PROLONG II study evaluated the usefulness of repeated D-d testing to assess the frequency and time frame of late hypercoagulability and its association with recurrences in subjects with a normal D-d 1 month after the suspension of VKAs for a first episode of VTE.
The results of the study indicate that an initially normal D-d 1 month after VKA suspension becomes abnormal at the third month in approximately 14% of cases and becomes abnormal at each subsequent time point in approximately 10% to 15% of subjects up to T270 and then it decreases to 8% to 10%. This late hypercoagulability is associated with a significantly increased rate of recurrence between T90 and T150 compared with subjects with normal D-d, while at the later time points the recurrence rate is significantly higher only for those patients in whom D-d was abnormal also in the previous time point. In those patients in whom D-d remains normal compared with the previous time point the rate of recurrence is negligible. These results indicate that the rate of recurrence in subjects with a normal D-d during and 1 month after VKA withdrawal is highest in the first 3 to 5 subsequent months and may warrant repeated testing in this time frame.
When the entire D-d time course over a year is considered, a normal D-d 1 month after VKA withdrawal remains normal in the majority of patients (66%) and in these patients the rate of VTE recurrence after T90 is low (2.7%; 2.9% pt-y). In the remaining patients, an initially normal D-d becomes abnormal at the third month and remains persistently abnormal in 14% of subjects and it is associated with a significant higher rate of recurrence compared with that of patients with normal D-d at T90 in whom D-d remains normal. In 20% of subjects D-d becomes abnormal after the third month and remains persistently abnormal afterward. In these patients the adjusted hazard ratio for recurrence is not statistically different from that of patients with persistently normal D-d at T90.
PE was present in 34% of patients and they might be more likely to convert from a normal to an abnormal D-dimer and also at higher risk of recurrence. No significant difference was observed either in the conversion of D-dimer from normal to abnormal or recurrence rate between subjects with PE (isolated or with DVT) and those with DVT without PE. However, the sample of subjects with PE was too small to draw definitive conclusions.
In those patients with an abnormal D-d either at T0 or 1 month after VKA withdrawal who continued or resumed VKAs and in whom D-d was retested after 3 to 6 months, D-d was abnormal in the majority of cases and VKAs were either continued or resumed for the long term. This indicates that an abnormal D-d at T0 or T30 remains abnormal over time in the majority of patients.
The results of this study should be evaluated with some caution. First, the trial was prospective, and bias could not be completely minimized, in spite of a blinded central adjudication committee. However, the baseline characteristics of patients who stopped anticoagulation were similar to those of patients who resumed anticoagulation except for age and comorbidities. The rates of events in treated and untreated patients are similar to those reported in the literature, albeit low, as expected, with large confidence intervals.
Second, some very early recurrences were observed in the first month after stopping VKAs and it is unknown whether testing D-d during anticoagulation could also help tailor the duration of treatment. However, only approximately 5% to 10% of subjects have an abnormal D-d during anticoagulation in the therapeutic range and very large studies would be needed to address this question.
Third, a qualitative method for D-d testing was used to allow a uniform approach across the participating centers for classifying D-d levels as either normal or abnormal. Although a formal interobserver variability assessment was not performed and some variability in the interpretation of the test can be expected, the test itself was previously shown to have good reproducibility.11 However, in a post-hoc analysis we have calculated specific cut-offs of different quantitative D-d methods on frozen plasma samples from the PROLONG study.17 The prospective management DULCIS (D-dimer and Ultrasound in Combination Italian Study) study is currently ongoing to validate these cutoffs.
Fourth, D-d time course was difficult to describe, as it did not always have a clear pattern. Some patients who had a persistently normal D-d also had a single abnormal test indicating only transient hypercoagulability, whereas others with an abnormal test had a normal D-d once or twice.
Fifth, although a normal D-d at T90, which remains normal over 1 year after VKA withdrawal, identifies a subgroup of patients with unprovoked VTE with a low risk of recurrence (2.7%; 2.9% pt-y), the lowest acceptable rate of recurrence, which may not warrant prolonging treatment after unprovoked VTE, is not yet defined. This low rate of recurrence could be similar to the expected rate of major bleeding (∼ 2% pt-y) during anticoagulation.6 In the present study, the rate of major bleeding in patients who continued or resumed long-term VKAs was very similar (4.8%; 3.3% pt-y) to the rate of recurrence in subjects with a persistently normal D-d over a year but higher than expected. This could be due to the higher risk of bleeding associated with the older age of patients with an abnormal D-d who resumed VKAs and also to their longer exposure time (mean follow-up of 18 months vs 10 months in patients with a normal D-d who stopped VKAs) as the majority of these patients underwent long-term anticoagulation.
In conclusion, the results of this study indicate that repeated D-d testing especially in the first 3 months after VKA withdrawal for a first episode of unprovoked VTE could identify a subgroup of patients with a low risk of recurrence, which may not warrant prolonged anticoagulation. To address this issue we are currently conducting the multicenter prospective management study DULCIS (http://clinicaltrials.gov; NCT00954395) in which D-d is tested in the first 3 months after VKA withdrawal together with RVO. Subjects with repeated normal D-d more than 3 months after VKA withdrawal and without significant RVO do not resume VKAs whereas subjects in whom D-d becomes abnormal over the first 3 months after stopping anticoagulation resume VKAs. The results of the study should be available by the end of 2011.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The study was supported by the Italian Federation of Anticoagulation Clinics (FCSA) and by the Department of Angiology and Blood Coagulation of the University Hospital St Orsola-Malpighi of Bologna (Coordinating Center), Italy. The Instrumentation Laboratory Co (Milan) provided the kits for D-dimer measurement (Clearview Simplify D-dimer test).
Authorship
Contribution: B.C. designed the study, wrote the protocol, performed the research, analyzed and interpreted the data, and wrote the manuscript; C.L. collected and analyzed the data and performed the statistical analysis; and A. Tosetto, V.P., A.G., S.T., D. Prisco, D. Poli, A. Tripodi, F.M., and G.P. designed the study and wrote the protocol, analyzed and interpreted the data, and contributed to writing the manuscript.
Conflict-of-interest disclosure: B.C., C.L., G.P., V.P., S.T., and A. Tripodi report having been paid lecture fees by the Instrumentation Laboratory Company, Milan, Italy. The remaining authors declare no competing financial interests.
A complete list of the PROLONG investigators appears as a supplemental Appendix to this article (available on the Blood website; see the Supplemental Materials link at the top of the online article).
Correspondence: Benilde Cosmi, Department of Angiology and Blood Coagulation Marino Golinelli, St Orsola-Malpighi University Hospital, Via Albertoni, 15-Bologna, Italy; e-mail: benilde.cosmi@unibo.it.