Abstract
Exposed subendothelial collagen acts as a substrate for platelet adhesion and thrombus formation after vascular injury. Synthetic collagen-derived triple-helical peptides, designated collagen-related peptide (CRP), GFOGER, and VWF-III, can specifically engage the platelet collagen receptors, glycoprotein VI and integrin α2β1, and plasma von Willebrand factor (VWF), respectively. Hitherto, the role of these 3 collagen-binding axes has been studied indirectly. Use of these uniform peptide substrates, rather than collagen fibers, provides independent control of each axis. Here, we use confocal imaging and novel image analysis techniques to investigate the effects of receptor-ligand engagement on platelet binding and activation during thrombus formation under flow conditions. At low shear (100s−1 and 300s−1), both GFOGER and CRP are required for thrombus formation. At 1000s−1, a combination of either CRP or GFOGER with VWF-III induces comparable thrombus formation, and VWF-III increases thrombus deposition at all shear rates, being indispensable at 3000s−1. A combination of CRP and VWF-III is sufficient to support extensive platelet deposition at 3000s−1, with slight additional effect of GFOGER. Measurement of thrombus height after specific receptor blockade or use of altered proportions of peptides indicates a signaling rather than adhesive role for glycoprotein VI, and primarily adhesive roles for both α2β1 and the VWF axis.
Introduction
The interaction of platelets with subendothelial collagen is critical to thrombus formation after vascular injury or atherosclerotic plaque rupture. Initial association of platelets with the damaged vessel wall occurs via von Willebrand factor (VWF) immobilized on exposed collagen and the platelet glycoprotein (Gp)Ib/V/IX complex.1 The transient nature of this interaction allows subsequent engagement of the platelet collagen receptors, integrin α2β12 and GpVI,3 with their recognition motifs in collagen, mediating firm platelet adhesion and activation. The relationship between these 3 adhesive axes in flowing blood has been the subject of extensive debate yet remains to be precisely defined.4-13
Blocking antibodies have been used to examine the effects of differential receptor adhesion. In particular, the role of α2β1 in platelet thrombus formation in flowing human blood is controversial, with some groups demonstrating that α2β1 is critical for platelet adhesion,4,10,14 whereas others have suggested a more limited role.6 Blockade of either GpVI or GpIb/V/IX reduced platelet thrombus formation,6,10,15,16 although in one of these studies,10 significant primary platelet adhesion at 1000s−1 remained under both conditions.
Recruitment of plasma VWF to experimental surfaces is shear-dependent and involves VWF dimers binding directly to collagen or multimerizing on preadsorbed VWF.6,17 Where collagen has been used as substrate, the surface density of each platelet-binding axis cannot be varied independently; and where a VWF coating has been used, the orientation of VWF, because it is random, may be nonoptimal. Moreover, any conformational change in VWF that might occur consequent to its deposition on collagen under shear is absent.
We have developed synthetic triple-helical collagen-mimetic peptides, GFOGER, specific for α2β1,18-20 and collagen-related peptide (CRP), specific for GpVI.21-23 The peptide VWF-III, containing the binding motif in collagen III for the VWF A3 domain, was shown to support platelet capture only at intermediate shear (300s−1) and, in solution, to inhibit static platelet adhesion to collagen.24 Its potential to support platelet adhesion and activation under higher shear, where VWF is strictly required, remains unknown. Individually, receptor-binding peptides have been used as antagonists of α2β1 and GpVI during platelet adhesion to collagen and to atherosclerotic plaque under higher shear.10,25 Recently, GpVI- and α2β1-binding motifs were combined in triple-helical peptides,26 revealing a need for high-affinity integrin-binding sites for full thrombus deposition, but these authors did not examine high shear or analyze thrombus morphology in detail. The present study was designed to extend our understanding of thrombus deposition on surfaces composed of discrete triple-helical peptides, to define the reactivity of collagen for VWF and for the platelet collagen receptors.
The introduction of the parallel-plate flow chamber offered control of blood flow over experimental thrombogenic surfaces.27,28 The present work, using combinations of peptides specific for each collagen-binding axis, extends control to the design of the collagenous substrate in such a flow chamber, operating between 100s−1 and 3000s−1. This comprehensive approach allows the contributions of each receptor system to be resolved.
Methods
This study received ethical approval from the Cambridge Human Biology Research Ethics Committee, and informed consent was obtained as applicable, according to the Declaration of Helsinki. Peptides were synthesized as described.18,21 The peptides used in these experiments include the CRP: GCO(GPO)10GCOG-amide (where O indicates hydroxyproline); GFOGER: GPC(GPP)5GFOGER(GPP)5GPC-amide; VWF-III: GPC(GPP)5GPRGQOGVMGFO(GPP)5GPC-amide, GPP10: GPC(GPP)10-GPCG-amide; GPO1: GCP(GPP)4GPO(GPP)5GCPG-amide; GPO2: GCP-(GPP)4(GPO)2(GPP)4GCPG-amide; GPO4: GPC(GPP)3(GPO)4(GPP)3GCPG-amide; GPO6: GCP(GPP)2(GPO)6(GPP)2GCPG-amide. GFOGER was also labeled with rhodamine (GFOGER-Rh) after solid phase peptide assembly (0.1 mmol scale), and removal of the final Nα-Fmoc protecting group. 5(6)-Carboxytetramethylrhodamine (0.6 mmol) was coupled for 16 hours to the peptide resin in dimethylformamide using N,N′-diisopropylcarbodiimide (0.6 mmol) and N-hydroxybenzotriazole (0.6 mmol). Cleavage, simultaneous side-chain deprotection, isolation, and purification were performed as for other peptides. Bovine tendon collagen I fibers were from Ethicon. Acid-soluble monomeric type I calf skin collagen was from Devro. The anti-GpVI scFv antibody 10B12 was selected from the Cambridge Antibody Technology (now MedImmune) phage display libraries as described previously.29 The anti-α2 monoclonal antibody 6F1 was a gift from Prof Coller (Mount Sinai Hospital, New York, NY). The anti-VWF A3 domain antibody RU5 has been described previously.30 The integrin αIIbβ3 inhibitory compound, GR144053 (4-[4-[4-(aminoiminomethyl)phenyl]-1-piperazinyl]-1-piperidineacetic acid trihydrochloride hydrate), was from Novabiochem. Phe-Pro-Arg-chloromethylketone (PPACK) was obtained from Cambridge Biosciences. Other chemicals were from Sigma-Aldrich.
Blood donation
Blood from healthy volunteers free from medication for 2 weeks was collected into 40μM PPACK and supplemented hourly with 10μM PPACK. Blood was incubated with 1μM 3,3′dihexyloxacarbocyanine iodide (DiOC6) for 15 minutes before use.
Whole blood perfusion experiments
Whole blood perfusion studies were performed as described10 with some modification. Glass coverslips (thickness no. 1, Menzel-Glaser) were coated with collagen or peptide. Each peptide, dissolved in 0.01M acetic acid, was coated at 0.1 mg/mL in a mixture containing a total of 0.3 mg/mL of peptide. For surfaces where only 1 or 2 active peptides were applied, the total peptide concentration was made up to 0.3 mg/mL with the inert homolog GPP10. Fibrous Ethicon collagen was coated at 0.1 mg/mL. Coverslips were covered with peptide solution and held in a humid chamber overnight at 4°C. After removal of excess fluid, they were blocked with 1% bovine serum albumin in HEPES buffer (36mM NaCl, 2.7mM KCl, 5mM N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid, 10mM glucose, 2mM MgCl2, 2mM CaCl2). The coverslip, in a 125- μm-deep flow chamber, was mounted on an FV300 laser-scanning confocal microscope (Olympus) and washed for 1 minute with HEPES buffer containing 100U/mL heparin. Blood was drawn through the chamber for 5 minutes using a syringe pump at calculated wall shear rates of 100, 300, 1000, and 3000s−1, corresponding to venous, arterial, arteriolar, and stenotic conditions, respectively; then residual blood was flushed using HEPES buffer before image acquisition. Where indicated, blood was preincubated for 15 minutes at 37°C with blocking antibodies. To visualize collagen coated onto coverslips before flow experiments, 0.1 mg/mL of fibrillar type I collagen was incubated with 10 μg/mL of GFOGER-Rh for 30 minutes at room temperature.
Image acquisition and analysis
Z-stacks (vertical sequences of images of a given field of view with step changes (ΔZ) of 0.69 μm and encompassing the entire thrombus height) were collected using an Olympus UplanFLN 40× NA1.30 oil immersion objective, a field size of 360 μm × 360 μm, and a confocal aperture of 60 μm. Z-stacks were exported to ImageJ1.35 (National Institutes of Health) for analysis. The coverslip plane, which yielded the primary measurement of surface coverage as a percentage of the field area, was defined as the Z-plane image with the largest platelet area. Thresholding the coverslip plane optimized contrast, a manipulation applied to all remaining images. Thrombus volume was calculated using the Cavalieri principle31 as the sum of the detected surface areas of all images of the Z-stack, multiplied by ΔZ. Dividing this value by the field area (giving units of μm3/ μm2) provides a free-standing measure of thrombus formation that can easily be compared between laboratories. Although a volume measurement, this parameter has the units of microns, and we refer to it as mean thrombus height. A separate measure of the absolute height of the thrombus, ZV50, was calculated as the Z-height at which the thrombus volume was half-maximal. A schematic representation of this concept is shown in Figure 3A and supplemental Figure 1E and further described in the supplemental Methods (available on the Blood Web site; see the Supplemental Materials link at the top of the online article). Inspection of Figure 3A reveals ZV50 as the height at which the cumulative increase of Z-stack volumes is half of the maximal volume. This value reports the height of center-of-mass of the thrombi and is normalized to the thrombus rather than the field area (supplemental Results). We used ImageJ to count the noncontiguous individual features per field (N). Thrombus morphology was further assessed by calculating the mean width of objects within the field: lines of single pixel thickness in the y-axis of the chamber were drawn, and pixels corresponding to thrombus or background were recorded.
Experimental design and statistics
From each surface, images were collected from 3 adjacent fields, each 5 mm from the blood inlet and arranged perpendicular to the axis of flow (shown in supplemental Figure 1A). Mean data from these 3 fields were used for calculations (outlined in the previous paragraph). Each experimental condition was tested using blood from 3 to 7 different donors (shown in the figure legends). Differences among mean values were identified using analysis of variance, and post-hoc comparisons used Student-Newman-Keuls or Student t tests with residual degrees of freedom and residual mean square to calculate pooled SD.
Results
Peptide substrates support platelet adhesion and thrombus formation at different shear rates
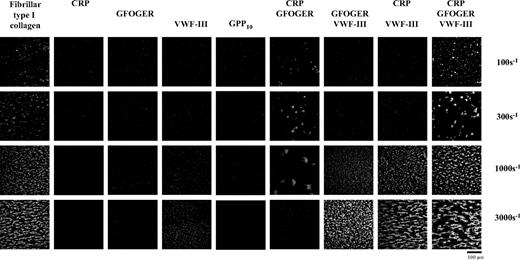
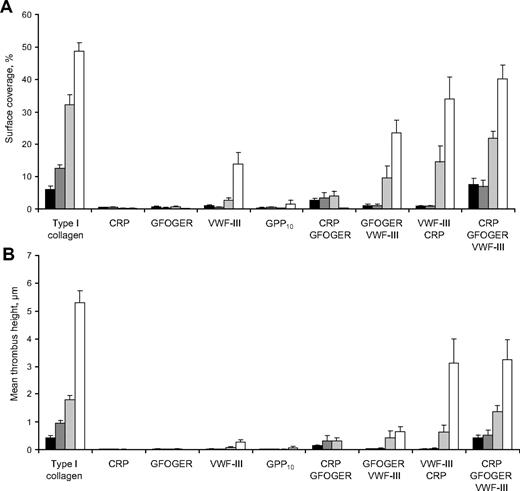
Blood was perfused over surfaces coated with collagen I fibers, or with combinations of synthetic triple-helical peptides, CRP, GFOGER, and VWF-III, as described in “Methods.” Platelets rapidly adhered to collagen fibers and formed discrete thrombi. Thrombus formation increased with wall shear rate (Figures 1–2), surface coverage from 6.1% plus or minus 0.9% at 100s−1 to 48.7% plus or minus 2.5% at 3000s−1 (P < .001), and mean thrombus height from 0.4 plus or minus 0.1 μm at 100s−1 to 5.3 plus or minus 0.4 μm at 3000s−1 (P < .001). Similar effects were seen using a combination of CRP, GFOGER, and VWF-III as substrate, although thrombus formation tended to be lower than observed on collagen I fibers at the highest shear rate. On this mixed peptide substrate, surface coverage increased with shear rate, from 7.6% plus or minus 1.8% at 100s−1 to 40.3% plus or minus 4.1% at 3000s−1 (P < .001), and mean thrombus height increased from 0.4 plus or minus 0.1 μm at 100s−1 to 3.3 plus or minus 0.7 μm at 3000s−1 (P < .001). No single peptide was able to support firm platelet adhesion at any shear rate tested, although VWF-III supported platelet rolling at higher shear rates. The increased surface coverage at 3000s−1 on VWF-III reflects loosely attached, rolling platelets. GPP10 proved inert, supporting lower incidence of single platelets than any other peptide. At the lower shear rates of 100s−1 and 300s−1, CRP and GFOGER in combination were required for significant thrombus deposition. Surface coverage and mean thrombus height were comparable at both shear rates. The inclusion of VWF-III with CRP and GFOGER resulted in substantially increased surface coverage and mean thrombus height. No other combinations of peptides supported measurable platelet adhesion at these shear rates.
Combinations of synthetic triple-helical peptides support differential platelet deposition under various shear rates. Slides were coated with combinations of collagen peptides as indicated, and perfused with DiOC6-labeled whole human blood for 5 minutes at the stated shear rates. Representative images showing thrombus deposition on surfaces having different peptide compositions are shown.
Combinations of synthetic triple-helical peptides support differential platelet deposition under various shear rates. Slides were coated with combinations of collagen peptides as indicated, and perfused with DiOC6-labeled whole human blood for 5 minutes at the stated shear rates. Representative images showing thrombus deposition on surfaces having different peptide compositions are shown.
Quantitative analysis of thrombus deposition on combinations of synthetic triple-helical peptide surfaces under shear conditions. Image analysis of platelet deposition and thrombus formation yielded different parameters of platelet adhesion and thrombus formation after perfusion of DiOC6-labeled whole blood over peptide-coated surfaces at the given shear rates for 5 minutes; n = 6 or 7. (A) Thrombus or platelet surface coverage (%). (B) Mean thrombus height (μm). Data are mean ± SEM. Shear rates:  indicates 100s−1;
indicates 100s−1;  , 300s−1;
, 300s−1;  , 1000s−1; and ▭, 3000s−1.
, 1000s−1; and ▭, 3000s−1.
Quantitative analysis of thrombus deposition on combinations of synthetic triple-helical peptide surfaces under shear conditions. Image analysis of platelet deposition and thrombus formation yielded different parameters of platelet adhesion and thrombus formation after perfusion of DiOC6-labeled whole blood over peptide-coated surfaces at the given shear rates for 5 minutes; n = 6 or 7. (A) Thrombus or platelet surface coverage (%). (B) Mean thrombus height (μm). Data are mean ± SEM. Shear rates:  indicates 100s−1;
indicates 100s−1;  , 300s−1;
, 300s−1;  , 1000s−1; and ▭, 3000s−1.
, 1000s−1; and ▭, 3000s−1.
At 1000s−1, all combinations of 2 peptides were able to support platelet deposition, resulting in similar mean thrombus height, but all 3 peptides together supported higher surface coverage and mean thrombus height than VWF-III together with CRP, VWF-III with GFOGER, or GFOGER with CRP.
At 3000s−1, VWF-III was absolutely required for platelet adhesion and thrombus formation. In combination with CRP, VWF-III supported the same extent of thrombus formation as all 3 peptides together, measured by either parameter. GFOGER in combination with VWF-III supported less surface coverage than all 3 peptides together. However, mean thrombus height was considerably lower.
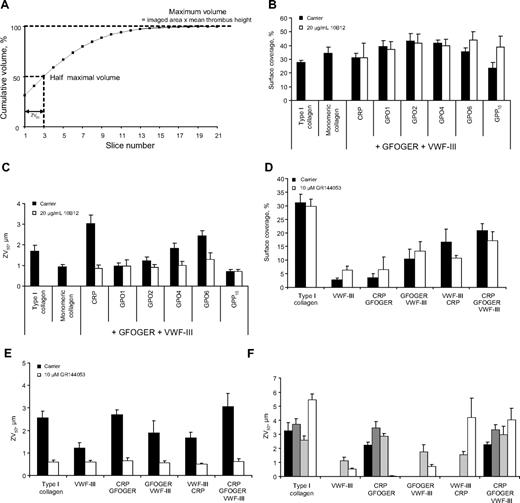
A novel parameter of thrombus formation, ZV50, reports platelet-platelet interactions under flow conditions
To test the hypothesis that the height of the thrombus correlates with the extent of platelet-platelet interactions, and thus reports the degree of platelet activation, we coated surfaces with fibrillar or monomeric collagen, or mixtures of GFOGER and VWF-III with 1 CRP-like peptide from a set containing increasing numbers of GPO triplets, and perfused these surfaces with blood at 1000s−1. Surface coverage revealed no significant differences among these substrates. However, ZV50 increased sequentially with increasing numbers of GPO triplets in the CRP-like peptides (Figure 3B-C). The ZV50 for nonactivatory monomeric collagen was comparable with that of the control substrate (GPP10 with GFOGER and VWF-III). Pretreatment with the anti-GpVI scFv, 10B12, abrogated the effect of the CRP-like peptides. Pretreatment of whole blood with the αIIbβ3 antagonist, GR144053, resulted in strikingly uniform ZV50 values of approximately 0.6 plus or minus 0.02 μm irrespective of surface composition without affecting surface coverage significantly (Figure 3D-E; supplemental Figure 4). This value of ZV50 approximates to the half-height of a platelet and suggests that largely single platelets are present on the slide. These observations demonstrate that ZV50 quantifies the extent of platelet activation under flow conditions.
ZV50 describes the activation state of adhered platelets in flowing human blood. Fibrillar collagen, monomeric collagen, or combinations of GFOGER, VWF-III, and one of a panel of CRP-like peptides containing increasing numbers of GPO triplets were used to coat slides. These were perfused with DiOC6-labeled whole human blood for 5 minutes at a shear rate of 1000s−1 with or without preincubation with 20 μg/mL of the anti-GpVI 10B12 or 10μM of the αIIbβ3 inhibitory compound, GR144053. (A) Schematic diagram showing the derivation of ZV50 and mean thrombus height. Consecutive volumes of each slice were accumulated sequentially until a value of 50% of the total volume was reached. This value corresponds to ZV50. Mean thrombus height is the thrombus volume per unit area of coverslip imaged (supplemental Figure 1). (B-C) Thrombus formation onto peptide mixtures of GFOGER and VWF-III with one of a panel of CRP-like peptides after treatment with 10B12. (D-E) Thrombus formation onto peptide combinations after treatment with GR144053. (B,D) Surface coverage (%). (C,E) ZV50 (μm). (F) ZV50 values obtained for combinations of CRP, GFOGER, and VWF-III peptides after blood flow at different shear rates. Data are mean ± SEM. Shear rates:  indicates 100s−1;
indicates 100s−1;  , 300s−1;
, 300s−1;  , 1000s−1; and ▭, 3000s−1.
, 1000s−1; and ▭, 3000s−1.
ZV50 describes the activation state of adhered platelets in flowing human blood. Fibrillar collagen, monomeric collagen, or combinations of GFOGER, VWF-III, and one of a panel of CRP-like peptides containing increasing numbers of GPO triplets were used to coat slides. These were perfused with DiOC6-labeled whole human blood for 5 minutes at a shear rate of 1000s−1 with or without preincubation with 20 μg/mL of the anti-GpVI 10B12 or 10μM of the αIIbβ3 inhibitory compound, GR144053. (A) Schematic diagram showing the derivation of ZV50 and mean thrombus height. Consecutive volumes of each slice were accumulated sequentially until a value of 50% of the total volume was reached. This value corresponds to ZV50. Mean thrombus height is the thrombus volume per unit area of coverslip imaged (supplemental Figure 1). (B-C) Thrombus formation onto peptide mixtures of GFOGER and VWF-III with one of a panel of CRP-like peptides after treatment with 10B12. (D-E) Thrombus formation onto peptide combinations after treatment with GR144053. (B,D) Surface coverage (%). (C,E) ZV50 (μm). (F) ZV50 values obtained for combinations of CRP, GFOGER, and VWF-III peptides after blood flow at different shear rates. Data are mean ± SEM. Shear rates:  indicates 100s−1;
indicates 100s−1;  , 300s−1;
, 300s−1;  , 1000s−1; and ▭, 3000s−1.
, 1000s−1; and ▭, 3000s−1.
On type I collagen fibers, ZV50 varied little with shear up to 1000s−1, but increased from 3.3 plus or minus 0.6 μm at 100s−1 to 5.4 plus or minus 0.4 μm at 3000s−1 (P < .001, Figure 3F). There was no significant difference between ZV50 values obtained on a mixture of CRP, GFOGER, and VWF-III at different shears. This suggests a similar degree of platelet activation by the peptide substrate under these conditions and, in turn, that the shear-dependent increase in surface coverage can be attributed to increased platelet adhesion. With CRP and GFOGER at shear rates up to 1000s−1, ZV50 was comparable. At 1000s−1, all combinations of 2 or more peptides resulted in similar ZV50 measurements. At 3000s−1, ZV50 on CRP with VWF-III and on all 3 peptides were comparable.
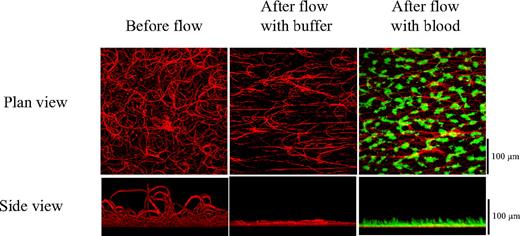
Fibrous collagen extends into the lumen of the flow chamber
To investigate the influence of collagen fiber organization on platelet adhesion, we visualized fibers by accretion of fluorescent peptide. At rest, the fibers extended more than 100 μm into the lumen of the flow chamber (Figure 4) but became flattened to approximately 20 μm after perfusion with buffer at 1000s−1. After perfusion with blood, the fibers tended to align with the direction of flow and to extend 5 or 6 μm into the thrombus layer.
Fibrillar collagen extends into the lumen of the flow chamber. Fibrillar collagen fibers were deposited onto a glass slide and stained using fluorescent peptide. Z-stacks were taken, and the profile of the fibers was obtained before and after flow at 1000s−1. (Top) Plan view. (Bottom) Side elevation.
Fibrillar collagen extends into the lumen of the flow chamber. Fibrillar collagen fibers were deposited onto a glass slide and stained using fluorescent peptide. Z-stacks were taken, and the profile of the fibers was obtained before and after flow at 1000s−1. (Top) Plan view. (Bottom) Side elevation.
Peptide substrates support thrombogenesis with characteristic morphologies at different shear rates
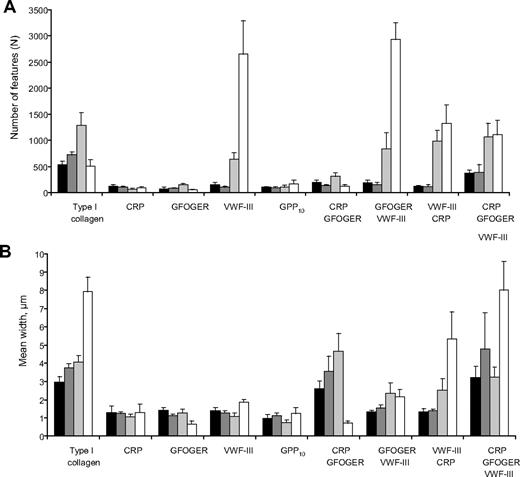
To investigate the effects of different peptide substrates on thrombus complexity, we extracted further parameters from the coverslip plane image, including the number (N) and mean width of detectable thrombi. On a fibrous collagen I substrate, N increased between 100s−1 to 1000s−1 but decreased at 3000s−1, shown in Figure 5A. Similar data were obtained using a combination of CRP, GFOGER, and VWF-III. At lower shear, a combination of all 3 peptides was the only substrate on which N was significantly greater than on the inert peptide control. At 1000s−1 and 3000s−1, many features were detected on VWF-III, reflecting platelet rolling across the surface. At 3000s−1, GFOGER with VWF-III yielded comparable numbers of features as VWF-III alone. On fibrous collagen I, mean width remained relatively constant from 100s−1 to 1000s−1 but increased abruptly at 3000s−1 (Figure 5B). Similar profiles were seen for surfaces coated with all 3 peptides. At 3000s−1 on GFOGER with VWF-III, mean width was reduced compared with using VWF-III with CRP or all 3 peptides. At 1000s−1, the mean width on CRP with GFOGER was greater than on CRP with VWF-III or GFOGER with VWF-III. The correlations between different parameters of thrombus formation are shown in supplemental Figure 3A through D.
Further parameters of thrombus morphology. Image analysis of objects (single platelets or thrombi) deposited on different peptide substrates at various shear rates yielded simple morphologic parameters, which quantitate the complexity of platelet adhesion and thrombus formation after 5 minutes of DiOC6-labeled whole blood flow at different shear rates. (A) Number of objects detected (N). (B) Mean width (μm). Shear rates:  indicates 100s−1;
indicates 100s−1;  , 300s−1;
, 300s−1;  , 1000s−1; and ▭, 3000s−1.
, 1000s−1; and ▭, 3000s−1.
Further parameters of thrombus morphology. Image analysis of objects (single platelets or thrombi) deposited on different peptide substrates at various shear rates yielded simple morphologic parameters, which quantitate the complexity of platelet adhesion and thrombus formation after 5 minutes of DiOC6-labeled whole blood flow at different shear rates. (A) Number of objects detected (N). (B) Mean width (μm). Shear rates:  indicates 100s−1;
indicates 100s−1;  , 300s−1;
, 300s−1;  , 1000s−1; and ▭, 3000s−1.
, 1000s−1; and ▭, 3000s−1.
Blocking platelet collagen receptors inhibits thrombus formation
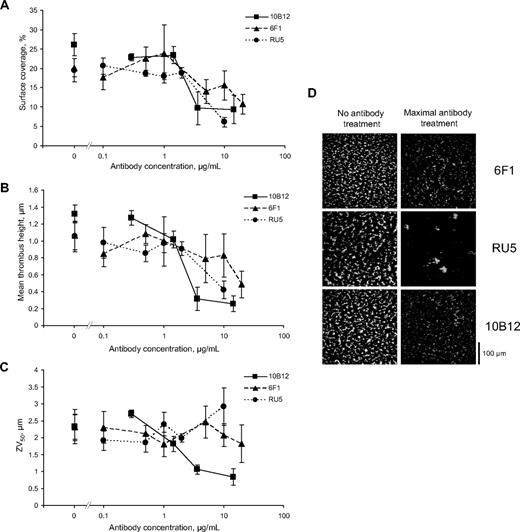
To investigate the authenticity of the peptides as ligands for their cognate receptors, blood was preincubated with specific blocking antibodies and was perfused at a shear rate of 1000s−1 over a substrate composing CRP, GFOGER, and VWF-III. Blockade of GpVI using 10B12 resulted in a dose-dependent reduction in surface coverage (Figure 6A) and mean thrombus height (Figure 6B). The anti-VWF A3 domain antibody, RU5 (10 μg/mL), and the anti-α2 antibody, 6F1 (20 μg/mL), each inhibited surface coverage and mean thrombus height. Treatment with 10B12 but not 6F1 or RU5 resulted in a dose-dependent decrease of ZV50 (Figure 6C).
Inhibitory antibodies targeting the major platelet collagen-binding axes reduce thrombus formation on a mixed peptide substrate under flow conditions. A surface consisting of CRP, GFOGER, and VWF-III was perfused for 5 minutes with DiOC6-labeled whole blood at a shear rate of 1000s−1 after treatment as indicated with the following antibodies: 10B12, 6F1, and RU5, which block GpVI, integrin α2 subunit, and VWF A3 domain, respectively. (A) Thrombus or platelet surface coverage (%). (B) Mean thrombus height (μm). (C) ZV50 (μm). (D) Representative images showing thrombus surface coverage after treatment with maximal concentration of antibody or in the absence of treatment.
Inhibitory antibodies targeting the major platelet collagen-binding axes reduce thrombus formation on a mixed peptide substrate under flow conditions. A surface consisting of CRP, GFOGER, and VWF-III was perfused for 5 minutes with DiOC6-labeled whole blood at a shear rate of 1000s−1 after treatment as indicated with the following antibodies: 10B12, 6F1, and RU5, which block GpVI, integrin α2 subunit, and VWF A3 domain, respectively. (A) Thrombus or platelet surface coverage (%). (B) Mean thrombus height (μm). (C) ZV50 (μm). (D) Representative images showing thrombus surface coverage after treatment with maximal concentration of antibody or in the absence of treatment.
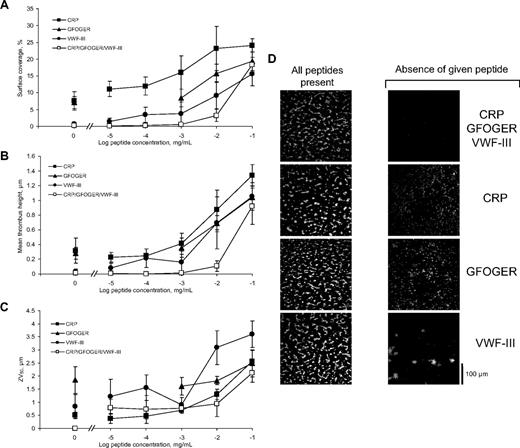
Reduction of peptide coating concentration inhibits thrombus formation differentially
To investigate the effect of reduced surface density of each receptor-reactive peptide, the inert GPP10 was progressively substituted for each active peptide during coating, and surfaces were tested at a shear rate of 1000s−1. Replacing 90% of all3 peptides with GPP10 caused a dramatic decrease in thrombus deposition, and a further order of magnitude reduction completely abolished platelet adhesion (Figure 7A-D). Holding GFOGER and VWF-III coating concentrations constant, a 10-fold reduction in CRP had no effect on surface coverage but decreased with further reduction in CRP concentration. Basal surface coverage of 10% to 15% was reached after 1000-fold reduction in CRP coating level. In contrast, mean thrombus height and ZV50 decreased with log (coating concentration), reaching a basal level as before. Progressive reduction in surface coverage, mean thrombus height, and ZV50 was seen with reducing VWF-III, leading to much lower basal levels, at 100- to 10 000-fold reduction in coating concentration. Removal of GFOGER from a mixture of all 3 peptides also caused a dose-dependent reduction in surface coverage, mean thrombus height, and ZV50, with basal levels reached at a concentration of 1 μg/mL. It is striking that substantially greater platelet adhesion remained in the absence of CRP than of either GFOGER or VWF-III.
Varying the concentration of one of a mixture of all 3 peptides alters platelet adhesion and thrombus formation under flow conditions. The relative coating concentrations of the different peptide types were altered to investigate the effect of different levels of receptor-ligand engagement on platelet deposition and thrombus formation, with 100 μg/mL as the control concentration of each peptide in the mixture. (A-D) The indicated component of the mixture was serially diluted with inert GPP10; then surfaces were prepared as described. (E-H) The concentration of a given peptide was increased from 100 μg/mL to 800 μg/mL in a mixture with 100 μg/mL each of the other peptide types. The resulting peptide substrate was perfused for 5 minutes with DiOC6-labeled whole blood at a shear rate of 1000s−1. (A,E) Surface coverage (%). (B,F) Mean thrombus height (μm). (C,G) ZV50 (μm). (D,H) Representative images showing thrombus deposition on peptide substrates deficient in the indicated peptide.
Varying the concentration of one of a mixture of all 3 peptides alters platelet adhesion and thrombus formation under flow conditions. The relative coating concentrations of the different peptide types were altered to investigate the effect of different levels of receptor-ligand engagement on platelet deposition and thrombus formation, with 100 μg/mL as the control concentration of each peptide in the mixture. (A-D) The indicated component of the mixture was serially diluted with inert GPP10; then surfaces were prepared as described. (E-H) The concentration of a given peptide was increased from 100 μg/mL to 800 μg/mL in a mixture with 100 μg/mL each of the other peptide types. The resulting peptide substrate was perfused for 5 minutes with DiOC6-labeled whole blood at a shear rate of 1000s−1. (A,E) Surface coverage (%). (B,F) Mean thrombus height (μm). (C,G) ZV50 (μm). (D,H) Representative images showing thrombus deposition on peptide substrates deficient in the indicated peptide.
Increasing surface peptide concentration reveals primarily adhesive roles for α2β1 and GpIb/V/IX
Increasing the concentration of a given coating peptide was investigated to clarify the roles of the different receptors in platelet adhesion and activation at a shear rate of 1000s−1. A mixture of 700 μg/mL of the inert peptide GPP10 with 100 μg/mL each of CRP, GFOGER, and VWF-III (1 mg/mL in total) was used to coat coverslips. Under these conditions, thrombus formation was virtually abolished (Figure 7E-H). Increasing the concentration of GFOGER to 800 μg/mL in a mixture with 100 μg/mL each of CRP and VWF-III resulted in an increase in surface coverage and mean thrombus height. Increasing the concentration of VWF-III to 800 μg/mL in a mixture with 100 μg/mL each of CRP and GFOGER gave similar increases. In contrast, increasing CRP to 800 μg/mL in a mixture with 100 μg/mL each of GFOGER and VWF-III resulted in reduced surface coverage and mean thrombus height. ZV50 remained at a constant level on all surfaces where thrombus was present.
Discussion
To eliminate the intrinsic variability of fibrous collagen preparations from the study of thrombus deposition in vitro, we developed receptor-specific synthetic collagen fragments. Varying their presence in the surface coating of a flow chamber provides independent control over the different adhesion receptors, allowing us to define their roles in a unique and unambiguous way. We demonstrate synergism between platelet collagen-binding receptors during thrombus formation under conditions representative of physiologic flow. Our data are consistent with a signaling, but not adhesive, role for GpVI. We also demonstrate a prominent role for GpIb/V/IX in platelet adhesion at higher shear observed under arteriolar or stenotic conditions and a primarily adhesive role for α2β1 at low venous or arterial shear. Our data also show novel roles in thrombus formation for α2β1 at high shear and GpIb/V/IX at low shear.
Inspection of surface coverage, mean thrombus height, and ZV50 data demonstrate the value of the image analysis procedures. Generally, such studies have presented only surface coverage,7,10,15,26,32,33 a parameter that can be misleading as it reports adhesion of platelets regardless of their activation state. The previously observed linear relationship between thrombus volume and surface coverage10 may apply only to deposition of fully competent platelets onto a replete peptide substrate or fibrous collagen. Deficiency or blockade of any specific receptor axis may result in a different relationship, as, for example, with a VWF-III coating, which recruits a monolayer of adherent platelets but cannot induce an activation-dependent increase in thrombus volume. Measurement of total thrombus volume in addition to surface coverage6,34 provides more insight into the activation state of adherent platelets. However, volume alone cannot discriminate between a few discrete, large thrombi (as deposited onto a surface coated with CRP and GFOGER) and a uniform monolayer of single platelets; valuable information about the activation process is lost. ZV50, introduced here, reflects the height of thrombi; thus, the average extent of platelet aggregate formation, regardless of surface coverage. For example, an increased ZV50 of thrombi is obtained after deposition onto CRP-like peptides with various GPO triplet content.23 Further, we observed low ZV50 in thrombi formed on monomeric collagen, reflecting its limited activatory properties.35 Regardless of the adhesive substrate, the αIIbβ3 inhibitor, GR144053, suppressed ZV50 to a uniform value, suggesting that ZV50 may sensitively report reduced αIIbβ3 function that might result from antiplatelet therapy or hemostatic deficiency, for example. This analytical approach, together with the introduction of defined and reproducible collagenous substrates, will lend itself to the investigation of platelet behavior in both a research and clinical setting.
Analysis of these simple, relatively low-resolution, whole field parameters, surface coverage, mean thrombus height, and ZV50 provides a rapid assessment of platelet behavior, whereas more intricate and comprehensive analysis can be performed using N and mean width.
It is only by comparing different parameters that we can draw conclusions about the roles of different collagen receptors. The high value for N observed on VWF-III at 3000s−1 indicates adhesion of single platelets without activation. This is confirmed by inspecting the ZV50 and mean width data, which show that the position of the center-of-mass of the thrombus on this substrate is comparable with the half-height of a single platelet and that the width of the features is equivalent to only 1 or 2 platelets. Both observations indicate single, nonactivated platelets. However, inspection of surface coverage alone would lead to the erroneous conclusion that VWF-III alone was sufficient for firm platelet adhesion and thrombus formation.
The use of fluorescently labeled peptides, which adsorb to the collagen fiber surface, allows us to visualize the tangled and inhomogeneous nature of the collagen fiber layer, which may, by offering larger surface area of collagen to the platelet than a peptide coating, contribute to its greater activity. We may also infer that variation in length and diameter of collagen fibers between preparations is probably a confounding factor in the standardization of such experiments, emphasizing the value of a flat, uniform peptide coating.
No single peptide supported firm platelet adhesion at any shear rate. This indicates that the corresponding receptor systems must cooperate to support thrombus deposition on peptide-coated surfaces. Platelets are found on VWF-III-coated surfaces at high shear, but these are loosely attached and do not represent true thrombi. At low venous and arterial shear, only a combination of CRP with GFOGER supports the formation of large thrombi. This ability of α2β1 to secure a growing thrombus is most clearly demonstrated by the high mean width. The morphology of thrombi formed on this surface can be explained by the stochastic nature of platelet adhesion. The probability that a given platelet will adhere to a CRP/GFOGER substrate at 1000s−1 is low. However, when adhesion does occur, engagement of GpVI ensures platelet activation. The bound platelet then acts as a nucleus to recruit other platelets from the flowing blood to form a large, discrete thrombus. VWF-III can substitute for neither GFOGER nor CRP in these binary peptide combinations at low shears, indicating that the adhesion afforded by the relatively sparse α2β1 is stronger than the interaction of surface-recruited VWF with the abundant GpIb/V/IX at this shear, and also that signaling through GpIb/V/IX is weak compared with that through GpVI. These data demonstrate that α2β1 is probably an important receptor in vivo at low shear in veins and arteries where the shear-dependent activation of VWF is minimal. Our data also show an increase in mean width at 3000s−1 when GFOGER is added to a mixture of CRP and VWF-III. This suggests a role for α2β1 in encouraging lateral thrombus growth at high shear rates. Video time courses (not shown) indicate that, at 3000s−1, large thrombi never form on a CRP/GFOGER surface, rather than forming and being lost by embolization. At arteriolar shear (1000s−1), the effect of VWF-III becomes more apparent, with all binary peptide combinations supporting thrombus deposition, although suboptimally compared with all 3 peptides together.
VWF-III, alone of these 3 peptides, is necessary but not sufficient for firm platelet deposition at high shear, with substantial surface coverage occurring on all VWF-III-containing surfaces. Thus, plasma VWF can be recruited by VWF-III in a conformation that is able to bind platelets. Our data also demonstrate a role for GpIb/V/IX at low shear. At 100s−1 and 300s−1, addition of VWF-III to CRP and GFOGER results in increases in surface coverage, mean thrombus height, and N, all suggesting an increased probability of platelet adhesion at these shears in the presence of VWF that has attracted little attention hitherto.
Submaximal coverage occurs on a VWF-III/GFOGER surface at high shear, and the low ZV50, low mean width, and high N indicate the presence of a monolayer of single platelets or small aggregates. Thus, GFOGER supports adhesion but not adequate platelet activation; nor can VWF supply the latter requirement despite its clear involvement in adhesion at high shear. Immobilized VWF A1 domain, interacting with GpIb/V/IX, has been shown to support α2β1 activation and platelet adhesion to collagen at 1500s−1 in the absence of plasma,36 resulting in the deposition of a platelet monolayer but not large thrombi, indicating inability of ligated GpIb/V/IX to elicit full platelet activation. The failure of GpVI to complete the activation process most probably reflects the use of monomeric collagen in these experiments, illustrating the importance of polymeric GpVI ligands in this setting. The corollary, that polymeric fibers support good thrombus deposition, is consistent with their ability to support GpVI dimerization, recently reported to be required for both platelet activation and adhesion.37
The present work shows that, although α2β1 with VWF-ligated GpIb/V/IX can support substantial platelet adhesion and thrombus formation on collagenous substrates, the involvement of GpVI enhances the activation process. This shows that signals arising through α2β1 and GpIb/V/IX, even in concert, do not fully activate αIIbβ3. However, the use of the high-affinity α2β1 ligand, GFOGER, shows that α2β1 contributes to thrombus growth, even at high shear in the presence of strong activation of αIIbβ3 via GpVI, and the greater consequent contribution of the VWF-αIIbβ3 interaction. Subtle measurement (mean width) is needed to prove the role of α2β1.
The effects of replacement of peptides with GPP10 within a coating mixture, are instructive. Dilution of either GFOGER or VWF-III causes a dose-dependent reduction in surface coverage, suggesting a direct relationship between peptide-coating concentration and platelet adhesion. In contrast, 10-fold dilution of CRP alone within a ternary mixture has no effect on surface coverage, although mean thrombus height is reduced at 1000s−1, showing that substantially reduced surface density of CRP cannot support full platelet activation and that the primary role of CRP is activatory rather than adhesive. Conversely, specific increase of an individual peptide in the surface coating at the expense of both other peptides indicates that excess CRP markedly reduces thrombus deposition, whereas excess of either VWF-III or GFOGER enhances thrombus formation. Thus, in the presence of low levels of both other peptides, CRP is unable to offer the necessary adhesion to support full thrombus formation, whereas residual activatory levels of CRP can exploit the extra adhesive capacity provided by a greater proportion of VWF-III or GFOGER, leading to greater thrombus deposition. This insight will inform the development of composite synthetic substrates that combine reactive motifs as described here, which will replace the heterogeneous and irreproducible collagen preparations currently used in thrombosis research. The present findings validate the use of such peptides.
An important conclusion from this work is that, despite the documented capacity of both GpIb/V/IX and α2β1 to induce activation of platelets, even in combination these 2 axes provide an insufficient stimulus for full thrombus deposition under shear. These adhesion receptors may elicit signals that share some downstream elements with the established GpVI pathway,38,39 but despite their relative abundance compared with GpVI, they must couple to intracellular signaling pathways less efficiently, indicating a different (primarily adhesive) role in thrombus deposition.
In conclusion, our data are consistent with the established role of GpIb/V/IX in the initial VWF-dependent capture of platelets, but we show here that α2β1 is required for optimal thrombus attachment to the substrate and subsequent thrombus growth. The roles of GpVI and α2β1 are more prominent at low venous and arterial shear (up to 300s−1), whereas GpIb/V/IX reinforces this activity at all shears and becomes increasingly important at more than or equal to 1000s−1. Notwithstanding this interpretation, α2β1 consolidates thrombus deposition even at stenotic shear rates (3000s−1). GpVI plays an activatory role at all shear rates but contributes little to direct platelet adhesion.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr G. Jarvis for assistance with data handling.
This work was supported by the British Heart Foundation and the Medical Research Council.
Authorship
Contribution: N.P. designed experiments, performed research, analyzed data, and wrote the manuscript; A.M.C.S. performed some research; N.R., P.A.S., and P.G.d.G. contributed vital reagents; and R.W.F. designed experiments and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Nicholas Pugh, University of Cambridge, Department of Biochemistry, Hopkins Bldg, Tennis Court Rd, Cambridge, CB1 2QW, United Kingdom; e-mail: np306@cam.ac.uk.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal