Abstract
It is currently considered that idiopathic minimal change nephrotic syndrome is an immune-mediated glomerular disease. Its association with classical Hodgkin lymphoma minimal change nephrotic syndrome (cHL-MCNS) suggests a molecular link, which remains to be elucidated. We analyzed the expression of cmaf inducing protein (c-mip) in lymphomatous tissues and kidney biopsy samples of patients with cHL-MCNS (n = 8) and in lymphomatous tissues of patients with isolated cHL (n = 9). Because c-mip affects the regulatory loop involving Fyn, we investigated possible structural defects in this signaling pathway, using laser capture microdissection, reverse transcription polymerase chain reaction, and Western blotting. We found that c-mip was selectively expressed in Hodgkin and Reed-Sternberg (HRS) cells and podocytes of patients with cHL-MCNS but is undetectable in patients with isolated cHL. We demonstrated that c-mip was specifically involved in the negative regulation of early proximal signaling through its interaction with phosphoprotein associated with glycosphingolipid-enriched microdomains and Fyn. We showed that the up-regulation of c-mip in cHL-MCNS was associated with a possible Fyn defect in HRS cells and podocytes. Moreover, we showed that c-mip was up-regulated in Fyn-deficient podocytes. c-mip may be a useful marker of cHL-MCNS and its induction reflects the dysregulation of proximal signaling.
Introduction
Classical Hodgkin lymphoma (cHL) is one of the most common malignant lymphoma in Western countries. It is characterized by the presence of malignant cells called Hodgkin and Reed-Sternberg (HRS) cells, which are embedded in a reactive cellular background consisting of T cells, histiocytes, eosinophils, and plasma cell infiltrates.1 HRS cells are not all derived from the same cell type. The majority (> 98%) are derived from germinal center or postgerminal center B cells, with a very small minority (< 2%) from T cells.2,3
Minimal change nephrotic syndrome (MCNS) is the most frequent glomerular disease, which can occur during the course of cHL.4 MCNS is an acquired glomerular disease of unknown origin, characterized by heavy proteinuria without inflammatory lesions or cell infiltrations. The pathogenesis of this disorder remains poorly understood; however, experimental studies and clinical observations suggest an immune origin.5 It is currently thought that MCNS is caused by a putative circulating factor, which increases glomerular capillary permeability and leads to podocyte cytoskeleton disorganization and proteinuria.6 However, in the case of cHL-associated MCNS (cHL-MCNS), the nature of such a putative glomerular permeability factor of HRS cell or reactive T-lymphocyte origin remains elusive.4
In a previous study of the molecular mechanisms underlying idiopathic MCNS (I-MCNS), we have isolated a new gene named for c-maf–inducing protein (c-mip).7 The naturally occurring isoform encodes an 86-kDa protein. The predicted protein structure of c-mip includes an N-terminal region containing a pleckstrin homology domain, a middle region containing several interacting docking sites including a 14-3-3 module, a protein kinase C domain, and an Src homology 3 domain similar to the p85 regulatory subunit of phosphatidylinositol 3-kinase, and a C-terminal region containing a leucin-rich repeat domain. The functional role of c-mip appears complex and is not clearly understood. We have recently shown that c-mip interacts with RelA and inhibits its nuclear translocation, resulting in down-regulation of NF-κB activity.8 We have also reported that c-mip interacts with filamin A, suggesting its involvement in cytoskeleton organization.9
In a recent retrospective study, we described the medical history of 21 patients with cHL-MCNS. Extensive immunohistochemical analysis of the lymph nodes for 8 of these patients did not provide any evidence for a B- or T-cell origin for HRS cells. The co-occurrence of MCNS and cHL, although rare, is not fortuitous but the mechanisms by which cHL induces podocyte disease remains unknown.10 In light of recent results suggesting a crucial role for c-mip in the pathogenesis of MCNS, we studied its presence in patients with Hodgkin lymphoma with or without associated MCNS.
Methods
Patients
Of the 8 patients with cHL-MCNS described previously,10 7 patients had available renal biopsy and lymphomatous tissue samples and were thus included in this study. MCNS and cHL occurred simultaneously in 2 cases (patients no. 1 and no. 2); MCNS occurred before cHL in 3 patients (patient no. 3 to patient no. 5) and after cHL in the 2 remaining patients (patients no. 6 and no. 7). The clinical, biologic, and histologic characteristics of these patients are summarized in Table 1. An additional patient with the simultaneous occurrence of both diseases was included in this study (patient no. 8). This patient was treated with a VBVP (vinblastine, bleomycin, etoposide and prednisone) chemotherapy regimen for cHL (clinical stage IIA,a) revealed by MCNS. A binephrectomy was performed 3 years after initial presentation because of steroid-resistant MCNS, rapid deterioration of renal function, and major denutrition, requiring the beginning of periodic hemodialysis. This patient did not have a previous history of opportunistic infection before the occurrence of cHL-MCNS but experienced multiple severe bacterial, fungal, and viral infections occurring after starting chemotherapy. All experiments were conducted with approval from the INSERM research ethics committee in accordance with international ethics codes and guidelines.
Clinical, biologic, and pathologic data for patients with cHL-MCNS
| Patient no. . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . |
|---|---|---|---|---|---|---|---|---|
| Sex | M | M | M | F | M | F | F | M |
| MCNS occurrence, mo/y | 07/1999 | 12/1990 | 06/1995 | 05/1995 | 03/1999 | 02/2000 | 06/2002 | 12/2000 |
| cHL occurrence, mo/y | 07/1999 | 12/1990 | 09/1995 | 11/1997 | 10/1999 | 08/1997 | 04/2002 | 12/2000 |
| Urinary protein level, g/d | 16 | 13.3 | 17 | 13 | 5.36 | 4.5 | 3 | 9 |
| Serum albumin, g/L | 8.9 | 14.8 | 19 | 10 | 12 | 10 | 13.8 | 12.8 |
| Ann Arbor staging | I | III | II | III | II | II | III | II |
| Systemic symptoms, A/B | A | B | A | A | B | A | A | A |
| Inflammatory syndrome, a/b | b | b | b | b | b | a | b | a |
| WHO classification | ns | ns | ns | ns | ns | ns | ns | ns |
| MCNS remission | Yes | Yes | SRNS | Yes | SRNS | SDNS | Yes | SRNS |
| cHL remission | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Patient no. . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . |
|---|---|---|---|---|---|---|---|---|
| Sex | M | M | M | F | M | F | F | M |
| MCNS occurrence, mo/y | 07/1999 | 12/1990 | 06/1995 | 05/1995 | 03/1999 | 02/2000 | 06/2002 | 12/2000 |
| cHL occurrence, mo/y | 07/1999 | 12/1990 | 09/1995 | 11/1997 | 10/1999 | 08/1997 | 04/2002 | 12/2000 |
| Urinary protein level, g/d | 16 | 13.3 | 17 | 13 | 5.36 | 4.5 | 3 | 9 |
| Serum albumin, g/L | 8.9 | 14.8 | 19 | 10 | 12 | 10 | 13.8 | 12.8 |
| Ann Arbor staging | I | III | II | III | II | II | III | II |
| Systemic symptoms, A/B | A | B | A | A | B | A | A | A |
| Inflammatory syndrome, a/b | b | b | b | b | b | a | b | a |
| WHO classification | ns | ns | ns | ns | ns | ns | ns | ns |
| MCNS remission | Yes | Yes | SRNS | Yes | SRNS | SDNS | Yes | SRNS |
| cHL remission | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
MCNS indicates minimal change nephrotic syndrome; cHL, classical Hodgkin lymphoma; M, male; F, female; ns, nodular sclerosis; a/A, absence; b/B, presence; WHO, World Health Organization; SRNS, steroid-resistant nephrotic syndrome; and SDNS steroid-dependent nephrotic syndrome.
The control group consisting of 9 patients with cHL without known renal disease was matched for age, Ann Arbor staging, and histologic subtype with the study group. All patients in the control and study groups were negative for HIV. Control cases were obtained from patient files of the Department of Pathology, Henri Mondor Hospital. All patients underwent a histologic study of the lymph nodes to confirm the diagnosis of cHL, which was based on the presence of HRS cells in an appropriate cellular background of reactive leucocytes, histiocytes and in some cases, fibrosis. The histologic subtypes were defined according to the World Health Organization classification of cHL (nodular sclerosis, mixed cellularity, and lymphocyte-rich and lymphocyte-depleted cHL).11 Laboratory tests for features of inflammatory syndrome including C-reactive protein, sedimentation rate, and fibrinogen levels were carried out. Systemic symptoms—fever, weight loss, and night sweats—were recorded for each patient. Diagnostic criteria for MCNS required the presence of nephrotic syndrome associated with minimal change glomerular lesions identified by light microscopy and negative immunofluorescence or the presence of immunoglobulin (Ig)M deposits in the mesangium upon histologic examination of kidney biopsy specimens. Microdissected glomeruli were obtained from frozen kidney tissue of patient no. 8, and from normal kidney tissue provided by our pathology department for control subjects.
In situ hybridization and immunohistochemistry
Reactive lymphoid tissue, normal adult thymus, and spleen were used as control tissues. Fyn-deficient mice (B6;129S7-Fyntm1Sor/j, stock number 2385) were obtained from The Jackson Laboratory. In situ hybridization (ISH) experiments were performed as described previously.12 The c-mip probe corresponds to positions 313-1072 of the cDNA coding sequence. For immunohistochemistry analysis, kidney samples were fixed for 16 hours in Dubosq Brazil, then dehydrated and embedded in paraffin. Antigen retrieval was performed by immersing the slides in boiling 0.01M citrate buffer in a 500 W microwave oven for 15 minutes. Endogenous peroxidase activity was blocked with 0.3% H2O2 in methanol for 30 minutes. Slides were incubated with the blocking reagents containing avidin-biotin solution for 30 minutes and normal blocking serum for 20 minutes. For detection of c-mip, slides were incubated overnight with polyclonal antibody at a final concentration of 15 μg/mL, then with biotinylated secondary antibody. Incubation with anti-Fyn antibody (Abcam) was performed according to the instructions provided by the manufacturer. We used an avidin-biotinylated horseradish peroxidase complex (Vectastain ABC Reagent; Vector Laboratories) with 3,3′-diaminobenzidine (Sigma-Aldrich) as a chromogen, for visualization of the immunoreaction. Slides were counterstained with hematoxylin. Primary antibody was omitted for negative control.
Laser capture microdissection
A series of 10-μm thick sections were cut from frozen tissue specimens using a Leica CM3050 cryostat at −20°C, and mounted onto slides coated with a thermoplastic membrane (Glass PEN-membrane slides; Leica Microsystems). Nuclei were stained with Mayer hematoxylin solution. Glomerular structures were selectively dissected using the AS LMD laser microdissection microscope (Leica Microsystems). Five 10-μm cryosections from each patient were used to microdissect 80 glomeruli each. Microdissected fragments were dropped into screw-cap vials containing 50 μL of extraction buffer. RNA was extracted from microdissected glomeruli with a PicoPure RNA Isolation Kit (Arcturus).
Cell-line culture and transfection
We used 2 well-characterized HRS cell lines originating from patients with nodular sclerosis (L428) or mixed cellularity subtype (KMH2), which we obtained from the Deutsche Culture Collection (DSMZ). Previous phenotypic and genotypic studies of HRS cell lines have shown that the L428 and KMH2 cell lines have a B-cell origin.13 All cell lines were grown in RPMI 1640 medium with Glutamax 1 supplemented with penicillin, streptomycin, 1% pyruvate, and 10% fetal calf serum, at 37°C in an atmosphere containing 5% CO2.
HRS cells (3 × 106 per condition) were transiently transfected with c-mip expression plasmid (1 μg/106 cells) or empty vector by electroporation using a Gene pulser X cell (Bio-Rad) set at 950 μF and 230 V. Cells were allowed to recover overnight and were harvested 20 hours after transfection for protein extraction and immunochemical analysis.
Reverse transcription–polymerase chain reaction
Total RNA was isolated using an RNeasy Kit (QIAGEN). Reverse transcription-polymerase chain reaction (RT-PCR) was performed as described previously.14 cDNA was prepared from whole lymphomatous tissue of patients with cHL with or without MCNS and from HRS cell lines. The transcripts Fyn, c-mip, FAT, neuropilin (NP1), and GAPDH were amplified using the primers listed in Table 2. PCR products were resolved on a 1.5% agarose gel and stained with SYBR Green.
Sequence of primers and PCR conditions
| mRNA . | Primer . | Accession no. . | Expected size, bp . | Annealing temp, °C . | PCR cycles . |
|---|---|---|---|---|---|
| GAPDH | F: ACCACAGTCCATGCCATCAC | AF261085 | 446 | 60 | 32 |
| R: TCCACCACCCTGTTGCTGTA | |||||
| Fyn | F: GAATTTAGATAATGGGCTGTGTGCAATGTAAGGAT | NM_153047 | 1605 | 60 | 34 |
| R: ACCCGGTTACAGGTTTTCACCAGGT | |||||
| C-mip | F: GGCCATGGATGTGACCAGCAGCTC | AK096598 | 2330 | 60 | 34 |
| R: TGGGAGCTTCACCAGGCTTCGGTGTAGC | |||||
| FAT | F: CAGCGACTCCATCCAGAAGCCTAGCTG | NM_005245 | 450 | 60 | 35 |
| R: CGAGGCATGTCTCTAGGAGGGTGGATG | |||||
| Neuropilin-1 | F: CTGATTCAGGCTCCGGACCCATACCAGAG | BC007737 | 684 | 60 | 35 |
| R: CTCCTGATTCCATGCCCAGAGCTTCCA |
| mRNA . | Primer . | Accession no. . | Expected size, bp . | Annealing temp, °C . | PCR cycles . |
|---|---|---|---|---|---|
| GAPDH | F: ACCACAGTCCATGCCATCAC | AF261085 | 446 | 60 | 32 |
| R: TCCACCACCCTGTTGCTGTA | |||||
| Fyn | F: GAATTTAGATAATGGGCTGTGTGCAATGTAAGGAT | NM_153047 | 1605 | 60 | 34 |
| R: ACCCGGTTACAGGTTTTCACCAGGT | |||||
| C-mip | F: GGCCATGGATGTGACCAGCAGCTC | AK096598 | 2330 | 60 | 34 |
| R: TGGGAGCTTCACCAGGCTTCGGTGTAGC | |||||
| FAT | F: CAGCGACTCCATCCAGAAGCCTAGCTG | NM_005245 | 450 | 60 | 35 |
| R: CGAGGCATGTCTCTAGGAGGGTGGATG | |||||
| Neuropilin-1 | F: CTGATTCAGGCTCCGGACCCATACCAGAG | BC007737 | 684 | 60 | 35 |
| R: CTCCTGATTCCATGCCCAGAGCTTCCA |
F indicates forward; R, reverse; and bp, base pair.
Preparation of glomerular extracts, immunoprecipitation, and Western blot analysis
Primary antibodies used in this study included, anti-CBP/PAG (sc-25 748; Santa Cruz Biotechnology), anti-Csk (Cell Signaling Technology), anti-Fyn (BD Biosciences), and anti-phosphotyrosine clone 4G10 (Upstate Biotechnology Associates). The anti-c-mip polyclonal antibody was produced in our laboratory by immunizing rabbits with acrylamide gel sections containing the c-mip protein.
Kidney fractions enriched in glomeruli were isolated using a graded sieving method. Cell protein extracts were prepared in lysis buffer (NaCl 150mM, 10mM Tris HCl [pH 7.5], 2mM DTT, 10% glycerol, 1mM ethylenediaminetetraacetic acid, 1% Nonidet P-40, 1mM of protease inhibitors, 1mM NaF, and 1mM sodium orthovanadate). Glomerular protein extracts were prepared in lysis buffer (50mM Tris Hcl [pH 7.5]), 150mM NaCl, 2mM ethylenediaminetetraacetic acid, 1%× Nonidet P-40, 0.5% sodium deoxycholate, 0.1% SDS, 1mM phenylmethylsulfonyl fluoride, 1mM of protease inhibitors, 1mM NaF, 1mM sodium orthovanadate). Immunoprecipitation was performed overnight at 4°C. Immunoprecipitates were resolved by SDS-PAGE and analyzed by Western blot with the indicated antibodies.
Results
Expression of c-mip in podocytes from patients with cHL and MCNS
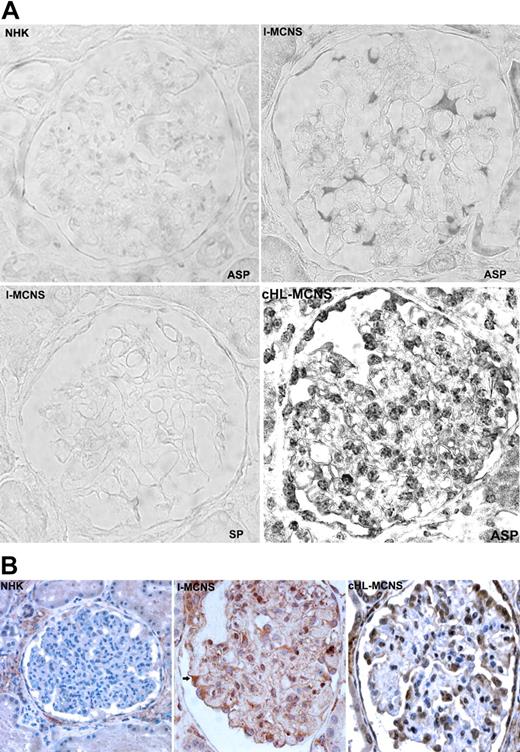
We have previously reported the clinical study of a series of patients with cHL-MCNS.10 In this present study, we examined whether a possible molecular link may exist between I-MCNS and cHL-MCNS. Our initial studies of c-mip expression in glomerular diseases showed that c-mip is induced in podocytes of patients with MCNS disease. The availability of biopsy specimens from patients with cHL-MCNS led us to investigate whether c-mip could be expressed in this entity. We performed ISH analyses on kidney biopsy specimens from 8 patients with cHL-MCNS and from 12 patients with I-MCNS. Incubation with a c-mip antisense probe revealed an intense signal in the glomeruli, which was mainly restricted to cells surrounding the capillary loops, suggestive of labeling in podocytes (Figure 1A), whereas no signal was seen with a c-mip sense probe. We also observed intense signal in parietal epithelial cells in 8 cHL-MCNS cases. Staining intensity appeared to be higher than in I-MCNS samples, with labeling detected throughout each glomerulus. Immunohistochemistry analysis showed that the distribution of c-mip protein correlated with the location of podocytes (Figure 1B). Within podocytes, c-mip was detected in the nuclear and cytoplasmic compartments. We conclude that, as observed for I-MCNS, podocytes in cHL-MCNS exhibited an up-regulation of c-mip at the mRNA and protein levels.
c-mip is up-regulated in the glomeruli of 8 patients with cHL-MCNS. (A) The top panel is representative ISH of c-mip transcript in serial sections from normal human kidney (NHK) and kidney biopsy specimens of patients with I-MCNS and cHL-MCNS. ASP indicates antisense probe; and SP, sense probe. (B) Representative immunohistochemistry on serial sections of normal human kidney and kidney biopsy samples from patients with I-MCNS and cHL-MCNS at an original magnification of ×40. c-mip up-regulation was detected in the podocytes of all patients with cHL-MCNS.
c-mip is up-regulated in the glomeruli of 8 patients with cHL-MCNS. (A) The top panel is representative ISH of c-mip transcript in serial sections from normal human kidney (NHK) and kidney biopsy specimens of patients with I-MCNS and cHL-MCNS. ASP indicates antisense probe; and SP, sense probe. (B) Representative immunohistochemistry on serial sections of normal human kidney and kidney biopsy samples from patients with I-MCNS and cHL-MCNS at an original magnification of ×40. c-mip up-regulation was detected in the podocytes of all patients with cHL-MCNS.
Expression of c-mip in lymphomatous tissue from patients with cHL, with or without associated MCNS
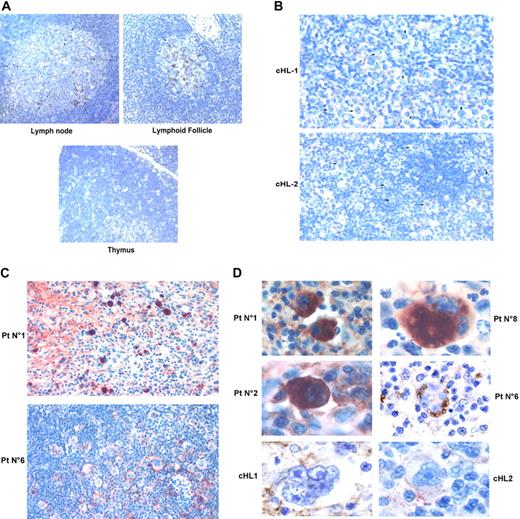
In light of our previous findings consistent with changes in T cell function in I-MCNS,15 we investigated whether c-mip was produced in lymphoid organs. In normal lymphoid tissues, the expression of c-mip was mostly negative in the thymus and in the red pulp of the spleen, with only a few scattered positive lymphoid cells observed (Figure 2A and data not shown). By contrast, c-mip was detected in lymph nodes and in lymphoid follicles within the white pulp of spleen (Figure 2A). Signal was mainly restricted to the transitional zone of the lymphatic follicle, which corresponds to the area of B- and T-cell cooperation.16 In lymphoid follicles, c-mip was selectively produced in the core of the follicle, a B cell–dependent area (Figure 2A). We then analyzed c-mip in lymphomatous tissue from 8 patients with cHL-MCNS and 9 patients with isolated cHL. We did not detect c-mip in lymph nodes from isolated cHL patients (n = 9), either in HRS cells, or in the reactive lymphocytes surrounding them (Figure 2B,D). On the other hand, c-mip labeling was particularly intense in HRS cells of 8 patients with cHL-MCNS (100%), with no significant signal detected in the surrounding reactive cellular infiltrates (Figure 2C-D). The percentage of positive HRS cells in cHL-MCNS patients varied from 10% to 90%. The highest level of c-mip immunoreactivity in HRS cells was observed in lymph nodes of patients with simultaneous occurrence of cHL and MCNS (Table 1). Within HRS cells, c-mip was either detected in the cytoplasm in the Golgi area of neoplastic cells, or at the plasma membrane (Figure 2C-D). Altogether, these findings show that cHL-MCNS is associated with an overexpression of c-mip in both HRS cells and podocytes and may represent a molecular signature of cHL-MCNS.
Up-regulation of c-mip in lymph nodes of 8 patients with cHL-MCNS is restricted to HRS cells. (A) Immunohistochemistry analysis of c-mip in normal lymphoid tissues (thymus, lymphoid follicle of the spleen and lymph nodes). Note that c-mip is not seen in normal tissues, except in the transitional zone of node tissue and in the lymphoid follicle (indicated by arrows) at an original magnification of ×20. (B) Representative image showing c-mip in lymphomatous tissues from 2 patients with isolated cHL at an original magnification of ×20. HRS cells are indicated by arrows. Note that c-mip is undetectable in lymphomatous tissues from isolated cHL. (C) Representative expression of c-mip in lymphomatous tissues from 2 patients with cHL-MCNS at an original magnification of ×20. c-mip shows intense staining in cHL-MCNS, restricted to HRS cells. (D) Localization of c-mip in HRS cells from 4 patients with cHL-MCNS. No staining was detected in the HRS cells of 2 patients with isolated cHL at an original magnification of ×100. c-mip up-regulation in HRS cells was found in all patients with cHL-MCNS, whereas no immunostaining was observed for c-mip in 9 control cases with isolated cHL
Up-regulation of c-mip in lymph nodes of 8 patients with cHL-MCNS is restricted to HRS cells. (A) Immunohistochemistry analysis of c-mip in normal lymphoid tissues (thymus, lymphoid follicle of the spleen and lymph nodes). Note that c-mip is not seen in normal tissues, except in the transitional zone of node tissue and in the lymphoid follicle (indicated by arrows) at an original magnification of ×20. (B) Representative image showing c-mip in lymphomatous tissues from 2 patients with isolated cHL at an original magnification of ×20. HRS cells are indicated by arrows. Note that c-mip is undetectable in lymphomatous tissues from isolated cHL. (C) Representative expression of c-mip in lymphomatous tissues from 2 patients with cHL-MCNS at an original magnification of ×20. c-mip shows intense staining in cHL-MCNS, restricted to HRS cells. (D) Localization of c-mip in HRS cells from 4 patients with cHL-MCNS. No staining was detected in the HRS cells of 2 patients with isolated cHL at an original magnification of ×100. c-mip up-regulation in HRS cells was found in all patients with cHL-MCNS, whereas no immunostaining was observed for c-mip in 9 control cases with isolated cHL
Given the malignant origin of the HRS cells, we sought to determine whether the c-mip gene exhibited any sequence changes. The gene encoding c-mip spans 268 kb on chromosome 16 and includes 21 exons encoding for an mRNA of 4.6 kb. The coding sequence consists of 2319 nucleotides. We purified c-mip mRNA from the podocytes and lymph node tissues of one patient with cHL-MCNS with high c-mip expression levels (patient no. 8). Analysis of the coding sequence of the transcript did not reveal any mutation (data not shown).
c-mip affects proximal signaling pathways in HRS cells
Proteins containing a pleckstrin homology domain, such as c-mip, are recruited into lipid rafts (LR) after the activation of membrane receptors involved in several signaling pathways including those of protein tyrosine kinase and Ras.17 We have previously demonstrated that c-mip interacts with Fyn in vitro and in vivo in various cell systems, including human embryonic kidney cells and podocytes (S.-y.Z., D.S., manuscript in revision, November 2009). Our understanding of the proximal regulation of Fyn comes primarily from T-cell studies; little is known about this regulation in podocytes.18,19
In physiologic situations, T cells are maintained in a resting state by an active mechanism involving the phosphorylation of phosphoprotein associated with glycosphingolipid-enriched microdomains (PAG) by Fyn within the LR.20,21 Activated PAG recruits Csk, a cytoplasmic protein tyrosine kinase, which phosphorylates the major pool of Fyn on tyrosine 528 (Fyn-Y528), enabling the intramolecular folding of the protein into its inactive conformation.22 The PAG/Fyn interaction appears to be essential for the function of PAG. Indeed, levels of PAG phosphorylation and subsequent interaction with Csk are dramatically reduced in Fyn-deficient T cells.21 Upon T-cell activation, CD45 moves into LR and dissociates the PAG-Fyn complex, resulting in PAG dephosphorylation, dissociation of the PAG-Csk complex and inactivation of Csk.23 Fyn released from its Csk inhibitor, binds to membrane receptors, such as the TCR δ-chain, and activates downstream targets, including phosphatidylinositol 3-kinase and Akt. Thus, depending on its partners, Fyn may have a dual effect on signaling, exerting inhibitory effects on unstimulated cells through its interaction with and phosphorylation of PAG, and stimulatory effects upon its dissociation from PAG and its interaction with activated receptors. These considerations along with previous results regarding the functional effects of c-mip on podocyte signaling led us to investigate whether c-mip interacts with PAG and/or Csk.
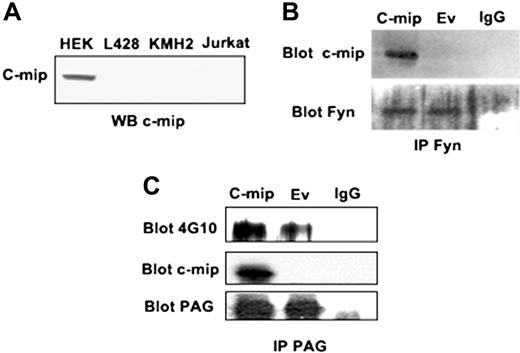
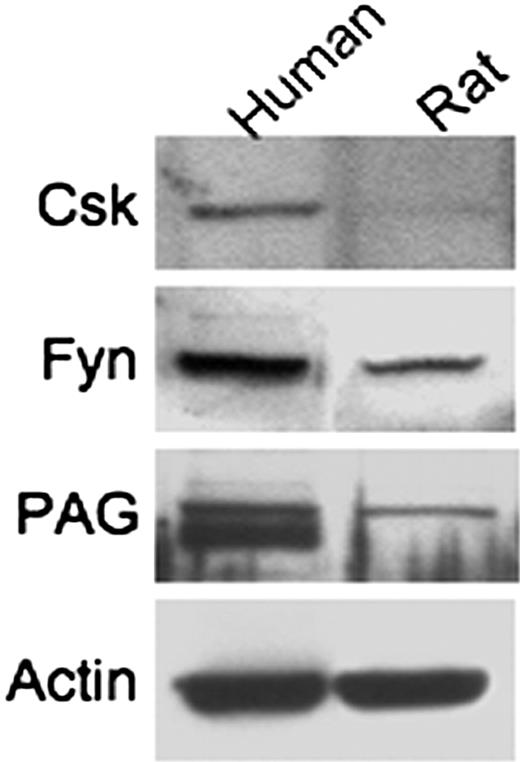
HRS cell lines, which do not constitutively produce c-mip (Figure 3A), were transfected with c-mip or empty vector, and then processed for immunoprecipitation and Western blot analyses. We found that c-mip interacted with endogenous Fyn in the HRS cell line (Figure 3B). Western blotting with the phosphotyrosine antibody 4G10 showed that c-mip also interacted with endogenous PAG and increased its phosphorylation (Figure 3C). On the other hand, we did not detect any interaction between c-mip and Csk. These results suggest that c-mip facilitates the negative regulation of early proximal signaling through activation of PAG. Given that active Fyn is required for PAG activation and that c-mip enhances the inhibitory role of Fyn, up-regulation of c-mip in HRS cells and podocytes may be caused by a break in the negative feedback loop, due to the inability of Fyn to exert its function. We therefore hypothesized that the regulation of the Fyn-PAG axis may be altered in HRS cells and in podocytes from patients with cHL-MCNS. To explore this possibility, we firstly analyzed the expression of PAG and Csk in podocytes. We found that Fyn, PAG, and Csk were present in human and rat glomerular extracts, suggesting that like in lymphocytes, the regulatory loop is operational in human podocytes (Figure 4).
c-mip interacts with PAG and Fyn in HRS cell lines. (A) Western blot detection of c-mip protein in lysates from HRS and Jurkat cell lines. Human embryonic kidney (HEK) cells were transfected with a c-mip expression plasmid and were used as positive controls. Immunoprecipitation of endogenous Fyn (B) and PAG/Cbp (C) from HRS cell lines cotransfected with the c-mip expression plasmid or empty vector (Ev).
c-mip interacts with PAG and Fyn in HRS cell lines. (A) Western blot detection of c-mip protein in lysates from HRS and Jurkat cell lines. Human embryonic kidney (HEK) cells were transfected with a c-mip expression plasmid and were used as positive controls. Immunoprecipitation of endogenous Fyn (B) and PAG/Cbp (C) from HRS cell lines cotransfected with the c-mip expression plasmid or empty vector (Ev).
Expression of Fyn signaling regulatory loop in human and rat glomeruli. The presence of Csk, Fyn, and PAG was analyzed by Western blotting on glomerular extracts.
Expression of Fyn signaling regulatory loop in human and rat glomeruli. The presence of Csk, Fyn, and PAG was analyzed by Western blotting on glomerular extracts.
Up-regulation of c-mip in cHL-MCNS patients is associated with Fyn deficiency in both HRS cells and podocytes
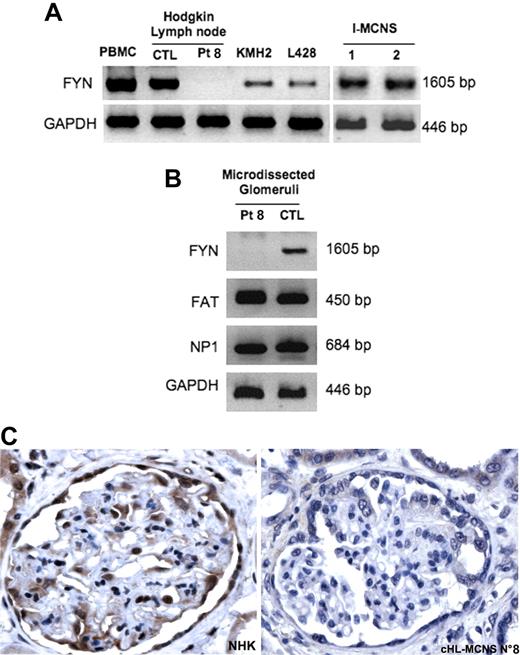
We hypothesized that c-mip induction may be associated with a defect of Fyn, because c-mip is a partner of Fyn, which is expressed in both podocytes and HRS cells.24,25 To test this hypothesis, we studied the expression of Fyn transcript using semiquantitative RT-PCR. Fyn transcript levels did not differ between lymph node tissue from patients with cHL and peripheral blood mononuclear cells (PBMC) from normal subjects (Figure 5A). However, we were unable to detect Fyn transcript in lymph node tissue from a patient with cHL-MCNS (patient no. 8), whereas it was found in HRS cell lines and in PBMC from 2 patients with an I-MCNS relapse (Figure 5A). We next analyzed the expression of Fyn in microdissected glomeruli from patient no. 8. Again, we did not detect any Fyn transcripts, whereas expression was easily observed in microdissected glomeruli from normal human kidneys (Figure 5B). By contrast, NP1 and FAT transcripts were produced normally in podocytes from this patient (Figure 5B). These results suggest that c-mip was recruited in response to changes in the proximal signaling negative regulatory loop in cHL-MCNS patients, which may involve a defect in Fyn expression. To confirm our observations, we performed immunohistochemistry analysis on kidney biopsy sample from this patient using anti-Fyn antibody (Figure 5C). By contrast to normal glomeruli, which exhibited strong immunostaining in podocytes with Fyn antibody, we did not detect any Fyn protein expression in glomeruli from this patient with cHL-MCNS. Altogether, these findings suggest that changes in proximal signaling induced by a potential defect in Fyn are likely to be involved in the up-regulation of c-mip in podocyte.
Absence of Fyn detection in lymphomatous tissue and in microdissected glomeruli from one patient with cHL-MCNS. (A) Analysis of Fyn expression by RT-PCR in normal PBMC, in lymphomatous tissue from patient no. 8 and a control patient with isolated cHL, in the PBMC of 2 patients with an I-MCNS relapse and in HRS cell lines. (B) Analysis of Fyn expression in microdissected glomeruli from patient no. 8 and a control patient without glomerular disease. Notably, transcripts for FAT and NP1 were easily detected in the microdissected glomeruli. (C) Immunohistochemistry analysis of Fyn protein in normal human kidney (left panel) and in a kidney biopsy specimen from patient no. 8 (right panel). Note the absence of Fyn protein from podocytes of patient no. 8.
Absence of Fyn detection in lymphomatous tissue and in microdissected glomeruli from one patient with cHL-MCNS. (A) Analysis of Fyn expression by RT-PCR in normal PBMC, in lymphomatous tissue from patient no. 8 and a control patient with isolated cHL, in the PBMC of 2 patients with an I-MCNS relapse and in HRS cell lines. (B) Analysis of Fyn expression in microdissected glomeruli from patient no. 8 and a control patient without glomerular disease. Notably, transcripts for FAT and NP1 were easily detected in the microdissected glomeruli. (C) Immunohistochemistry analysis of Fyn protein in normal human kidney (left panel) and in a kidney biopsy specimen from patient no. 8 (right panel). Note the absence of Fyn protein from podocytes of patient no. 8.
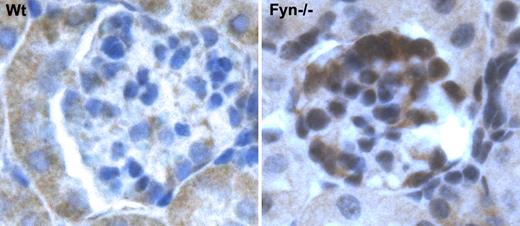
Fyn-deficient mice exhibited an up-regulation of c-mip in podocytes
The results presented here suggest that up-regulation of c-mip in the podocytes of patients with cHL-MCNS may be due to a Fyn defect. We thus analyzed c-mip protein in Fyn-deficient mice.26 These mice were proteinuric at 1 month of age and previous ultrastructural studies have shown that podocyte foot processes are altered.24 Immunohistochemistry analysis showed significant induction of c-mip in 1-month-old Fyn null mice, but not in wild-type littermates (Figure 6). This result supports our in vivo data from patient no. 8.
c-mip is up-regulated in Fyn-deficient mice. Immunohistochemistry analysis of c-mip in serial sections from normal and Fyn-deficient mice kidneys at an original magnification of ×40.
c-mip is up-regulated in Fyn-deficient mice. Immunohistochemistry analysis of c-mip in serial sections from normal and Fyn-deficient mice kidneys at an original magnification of ×40.
Discussion
It is currently considered that MCNS is an immune-mediated glomerular disease. Its association with cHL suggests there that is a molecular link between these 2 disorders. In this study, we demonstrated, for the first time, that c-mip is selectively induced both in podocytes and in HRS cells in patients with cHL-MCNS but is not detected in patients with isolated cHL, suggesting its potential involvement in the pathophysiology of this association. We showed that (1) c-mip interacted with PAG and Fyn; (2) c-mip transcript from lymphomatous tissue and podocytes did not carry any mutation in the coding sequence; and (3) the up-regulation of c-mip in cHL-MCNS may be associated with a defect in Fyn, which is normally expressed in isolated cHL.25
Although the expression of c-mip in I-MCNS is clearly established, it is important to note that its expression level in podocytes and HRS cells of patients with cHL-MCNS is much higher than in the cells of patients with I-MCNS. This suggests that the changes of proximal signaling are more severe in cHL-MCNS and may result from a protein defect.
Fyn plays a major role in podocyte proximal signaling. However, as for the nephrin signaling pathway, the mechanisms that regulate its activity in these cells are largely unknown. In lymphocytes, many studies have shown that Fyn is inactivated upon its dissociation from PAG and subsequent binding with Csk.26-28 It has been shown that Fyn-deficient mice display proteinuria even in the rag−/− genetic background, suggesting that podocyte damage is independent of immune mechanisms.29
The role of c-mip in the negative regulation of proximal signaling is underscored by its ability to interact with Fyn and PAG. We show that c-mip, like active Fyn, increases the phosphorylation of PAG. In cHL-MCNS, it is possible that c-mip compensates for the deficiency in Fyn by reducing cell activity through enhanced negative proximal signaling. c-mip is mainly restricted to the transitional zone of B-cell follicles and lymphoid follicles in normal hematopoietic tissues, suggestive of a role in B-cell/helper T-cell cooperation and in B-cell function. Despite previous clinical and experimental studies suggesting a disorder of a T function, recent data suggest that B cells may be involved in the pathogenesis of MCNS. Rituximab, a chimeric monoclonal antibody, which inhibits B-cell proliferation and differentiation, has recently been used successfully in patients with steroid-dependent MCNS.30 Although speculative, we cannot exclude that B cells may be involved in the pathogenesis of MCNS. Early studies have demonstrated an impairment of Ig production during MCNS relapse, in which IgG levels are severely reduced with unbalance of IgG subclasses, suggesting that intrinsic B-cell properties and class switch recombination may be primarily altered.31
This patient cohort shows clear up-regulation of c-mip in cHL-MCNS. However, only one patient, with a demonstrable defect in Fyn, likely to account for the steroid resistance seen in MCNS, offers us a clue as to the underlying mechanisms. We cannot exclude the possibility that another protein involved in the negative regulation of proximal signaling could be defective in other patients. In a previous study, Fyn was found to be expressed in HRS cells in 42% of the cHL cases analyzed.25 We therefore screened for Fyn expression in the lymphocytes of patients with I-MCNS. We found that the transcript expression is normal in these patients, contrasting with observations for our patient with cHL-MCNS. Nevertheless, c-mip up-regulation probably reflects a defect in the negative regulation of proximal signaling. The identification of Fyn and c-mip binding partners in podocytes will be essential for a thorough understanding of the pathophysiology of this disease.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We are grateful to Dr François Combarnous, Dr Raymonde Bouvier, and Dr Aurelia Liutkus (Nephrology Department, Lyon, France) for help with the care and follow-up of patient no. 8. We thank Dr Yves Allory and Dr Karen Leroy (Pathology Department, Henri Mondor Hospital, Créteil, France) for providing us with control renal tissues and mRNA samples from patients with isolated cHL.
This work was supported in part by an Avenir Program from Inserm, a grant from the French Kidney Foundation, and the Association pour l'Utilization du Rein Artificiel (AURA). V.A. is a recipient of an Inserm Poste.
Authorship
Contribution: V.A., S.-y.Z., C.C.-B., C.R-M., V.O., M.C., and M.B. performed the experiments; A.P. and D.S. designed the research; P.L. contributed to the management of the project; V.A., S.-y.Z., C.C.-B., A.P., and D.S. analyzed the data; and V.A. and D.S. wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Dil Sahali, Inserm, U955, Equipe 21, Creteil, France; e-mail: dil.sahali@inserm.fr.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal