Abstract
Imbalance of T-helper cell (Th) differentiation and subsequent cytokine dysregulation is implicated in inflammatory and autoimmune diseases. In particular, 2 cytokines produced by different Th cell populations, interferon-γ (IFN-γ) and interleukin-17 (IL-17), have been shown to play a critical role in autoimmunity. We have examined the roles of these cytokines in a mouse model of systemic autoimmunity resulting from the deletion of IL-2 in which autoimmune hemolytic anemia (AIHA) is a prominent feature. We demonstrate that, in IL-2–knockout (KO) BALB/c mice, elimination of the Th1 cytokine, IFN-γ, delays the development of AIHA. Further, CD4+ T cells from IL-2/IFN-γ–KO mice produce elevated levels of IL-17 compared with wild-type (WT) and IL-2–KO, and these mice eventually develop intestinal inflammation. In contrast, elimination of the Th17 cytokine, IL-17, from IL-2–KO mice fails to suppress early acute AIHA development. These results suggest that in a systemic autoimmune disease with multiple manifestations, Th1 cells drive the early autoantibody response and IL-17–producing cells may be responsible for the more chronic tissue inflammation.
Introduction
The interleukin-2 knockout (IL-2–KO) mouse provides a powerful model for defining the signals involved in the development of spontaneous autoimmune disease in the absence of regulatory T cells. IL-2–KO mice on the BALB/c background develop a systemic autoimmune disease, dying by 5 weeks from complications of autoimmune hemolytic anemia (AIHA).1 The principal immunologic defects in these mice are a deficiency of regulatory T lymphocytes (Tregs) leading to a breakdown of self-tolerance and failure of T-cell homeostasis, resulting in uncontrolled activation and proliferation of CD4+ T cells.2,3 It has been shown that AIHA progression in these animals is mediated by autoantibodies and is dependent on abnormal helper T-cell (Th) activity.1,4,5 We used this mouse model of spontaneous, acute systemic autoimmunity to define the cytokine milieu that influences the development of autoimmune disease.
A tightly controlled balance between activation and suppression normally maintains immune homeostasis. Dysregulated cytokine expression is documented in various autoimmune and inflammatory diseases, and in the expansion of autoreactive T cells.6-10 Our understanding of the cytokine network required to induce, amplify, and control self-reactive lymphocytes continues to evolve. Autoimmune manifestations have traditionally been thought to be mediated by Th1 cells and their abundant interferon-γ (IFN-γ) and tumor necrosis factor (TNF) production. With the more recent identification of the Th17 subset, the role of cytokines in autoimmunity is being re-evaluated. Th17 cells are potent inducers of tissue inflammation, and dysregulated expression of IL-17 appears to initiate organ-specific autoimmunity; this has been best characterized in mouse models of colitis,11 experimental autoimmune encephalomyelitis,12 and rheumatoid arthritis.13 The specific roles and interactions of Th subsets during the development of autoimmunity are a topic of great interest at present.14,15
In this study, we set out to evaluate the contributions of Th1 and Th17 cytokines in the development of inflammation and autoimmunity in the absence of Tregs using the IL-2–KO mouse model. We demonstrate a clear role for IFN-γ in the production of autoantibodies and progression of AIHA. In the absence of IFN-γ, IL-2–KO mice show delayed AIHA but, over time, develop intestinal inflammation, whereas elimination of IL-17 has no impact on the kinetics of AIHA development. Thus, our studies reveal that different cytokines play distinct roles in various manifestations of autoimmunity in the absence of Tregs.
Methods
Mice
Mice lacking IL-2, IFN-γ, IL-17, IL-2/CD28, IL-2/CD40L, IL-2/IFN-γ, and IL-2/IL-17 were used on the BALB/c background. Mice were bred and maintained in our specific pathogen-free facility at the Animal Barrier Facility in accordance with the guidelines of the Laboratory Animal Resource Center of the University of California San Francisco.
Lymphocyte isolation
Lymph nodes (LNs) and spleens were pressed through a nylon mesh filter, red blood cells (RBCs) hypotonically lysed, then lymphocytes washed and resuspended in phosphate-buffered saline (PBS) with 1% fetal bovine serum (FBS).
Antibodies and flow cytometry
Splenocytes and lymphocytes were stained with fluorescently conjugated antibodies (BD Biosciences, San Jose, CA; and eBioscience, San Diego, CA) after Fc-block (anti-CD16/CD32). Flow cytometry was performed on a BD FACSCalibur or a LSR II System (BD Biosciences) and data analyzed using FCS Express (DeNovo Software, Los Angeles, CA).
Complete blood counts
Cardiac punctures were performed after cervical dislocation, and blood drawn into heparinized microhematocrit tubes. Complete blood counts were then evaluated using a Hemavet 950 (Drew Scientific, Wayne, PA).
Intestinal staining
Small intestine and colon sections were stained with hematoxylin and eosin. Slides were viewed with a Zeiss Axioskop 2 plus photomicroscope (Zeiss, Thornwood, NY) using a Plan-APOCHROMAT lens at 10×/0.45 NA and Permount mount medium (Fisher Scientific, Santa Clara, CA). Images were acquired using a Zeiss Axio Cam HRc color camera and were processed with AxioVision software version 3.1 and Adobe Photoshop CSII software (Adobe Systems, San Jose, CA).
ELISAs
Immunoglobulin enzyme-linked immunosorbent assays (ELISAs) were performed as previously described.5 Absorbance was determined with an ELISA plate reader (Molecular Devices, Sunnyvale, CA) at 405 nm. The immunoglobulin concentrations were calculated by comparison against a standard curve of serially diluted IgG1, or IgG2a.
RBC antibody detection
Serum RBC antibody levels were detected using flow cytometry similar to that previously described.16 RBCs were freshly isolated from young mice by terminal bleed and washed 3 times in cold PBS. RBCs were then incubated with anti–murine IgM–fluorescein isothiocyanate (FITC; 1:300 dilution, on ice) or IgG-FITC (1:50 dilution; at 37°C; Jackson ImmunoResearch Laboratories, West Grove, PA). The percentage of RBCs bound by antibody was determined by flow cytometry.
Macrophage phagocytosis assay
Splenic macrophages were seeded on plastic culture plates for 3 hours at 37°C. Plates were washed extensively with warm PBS to remove nonadherent cells. Macrophages were removed by trypsin treatment and replated at equal cell numbers overnight with or without 500 ng/mL lipopolysaccharide (LPS) stimulation. FITC-labeled Escherichia coli BioParticles (Vybrant Phagocytosis Assay Kit; Invitrogen, Carlsbad, CA) were added for the final 2 hours at 37°C according to the manufacturer's instructions. Macrophages were detached by trypsinization, and phagocytosis was analyzed by fluorescence-activated cell sorter (FACS) after staining with anti-F4/80 and CD11b antibodies.
Cytokine production
LN cells were plated in tissue culture plates and stimulated with 50 ng/mL phorbol myristate acetate (PMA) and 500 ng/mL ionomycin for 5 hours. Brefeldin A was added during the final 2 hours. Cells were collected, stained with anti-CD4, IL-17, IL-4, and IFN-γ fluorescently conjugated antibodies, and then evaluated by flow cytometry.
Real-time PCR
RNA was isolated from peripheral LN, mesenteric LN, or descending colon using TRIzol (Invitrogen) or RNeasy Mini Kits (QIAGEN, Valencia, CA). RNA was converted to cDNA using SuperScript III reverse transcriptase (Invitrogen). Amplification of transcripts was performed using SYBR green polymerase chain reaction (PCR) Master Mix (Applied Biosystems, Foster City, CA) and run on an iQ5 Real-Time PCR Thermal Cycler (Bio-Rad, Hercules, CA). Reactions were performed in duplicate and normalized to hypoxanthine phosphoribosyltransferase (HPRT) levels. Primer sequences used: IL-21 (GCCAGATCGCCTCCTGATTA; CATGCTCACAGTGCCCCTTT), retinoid-related orphan receptor-γt (ROR-γt; TGTCCTGGGCTACCCTACTG; GTGCAGGAGTAGGCCACATT), ROR-α (TCTCCCTGCGCTCTCCGCAC; TCCACAGATCTTGCATGGA), IL-23R (TCAGT-GCTACAATCTTCAGAGG; GCCAAGAAGACCATTCCCGA), and IL-1R1 (CTCTTCCCAATCCAGTTCCA; TGCGGGACACTAAGGAGAAA). Primer sequences are described elsewhere for HPRT17 and IFN-γ, IL-17A, IL-17F, t-bet, Gata-3.18
Statistics
Statistical differences between experimental groups were determined by the unpaired Student t test. Bar graphs indicate means, and error bars indicate SDs.
Results
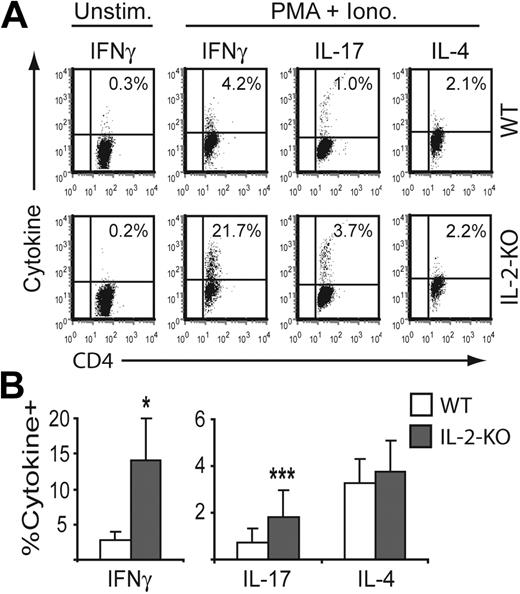
Absence of IL-2 results in elevated production of IFN-γ and IL-17 in CD4+ T cells
As a first step toward defining the cytokines involved in the autoimmune disease of IL-2–KO BALB/c mice, we evaluated the production of several cytokines by CD4+ T cells. Cells were stimulated ex vivo with or without PMA and ionomycin for 5 hours, and cytokine production was measured by intracellular cytokine staining and flow cytometry. IL-2–KO CD4+ T cells exhibited a 5-fold increase in IFN-γ and a 2.5-fold increase in IL-17 production relative to wild-type (WT) CD4+ T cells, whereas IL-4 production remained unchanged in IL-2–KO compared with WT CD4+ T cells (Figure 1). Neither WT nor IL-2–KO CD4+ T cells produced IFN-γ without stimulation; however, IFN-γ mRNA levels were elevated approximately 10-fold over WT levels in nonstimulated cells (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article). We next evaluated the mRNA expression level of transcription factors that drive Th1 (t-bet), Th2 (GATA-3), and Th17 (ROR-γt) differentiation in nonstimulated WT and IL-2–KO LN CD4+ T cells. Elevated IFN-γ expression by IL-2–KO CD4+ T cells was concomitant with an increase in t-bet mRNA, whereas GATA-3 and ROR-γt mRNA levels were comparable between WT and IL-2–KO CD4+ T cells (Figure S1). We have previously shown that deleting either CD28 or CD40L eliminates AIHA development in IL-2–KO mice.5 We next compared IFN-γ cytokine production by IL-2/CD28-KO and IL-2/CD40L-KO CD4+ T cells to that of IL-2–KO and WT CD4+ T cells. Elimination of CD28 or CD40L returned IFN-γ production by IL-2–KO CD4+ T cells to near WT levels (data not shown). Because IL-2/CD28 and IL-2/CD40L-KO mice are free of AIHA, these data are consistent with the hypothesis that elevated expression of IFN-γ may be contributing to autoimmune disease development.
Elevated IFN-γ and IL-17 production in IL-2–KO CD4+ T cells. Lymph node cells from 3- to 4-week-old mice were stimulated with or without 50 ng/mL PMA and 500 ng/mL ionomycin for 5 hours, and cytokine production in CD4+ T cells was evaluated by intracellular cytokine staining. The percentage of cytokine-producing CD4+ T cells was measured by flow cytometry. (A) FACS profiles are representative data from one experiment. (B) Bar graphs represent mean plus or minus SD of 5 mice from independent experiments. *P < .001; ***P < .05.
Elevated IFN-γ and IL-17 production in IL-2–KO CD4+ T cells. Lymph node cells from 3- to 4-week-old mice were stimulated with or without 50 ng/mL PMA and 500 ng/mL ionomycin for 5 hours, and cytokine production in CD4+ T cells was evaluated by intracellular cytokine staining. The percentage of cytokine-producing CD4+ T cells was measured by flow cytometry. (A) FACS profiles are representative data from one experiment. (B) Bar graphs represent mean plus or minus SD of 5 mice from independent experiments. *P < .001; ***P < .05.
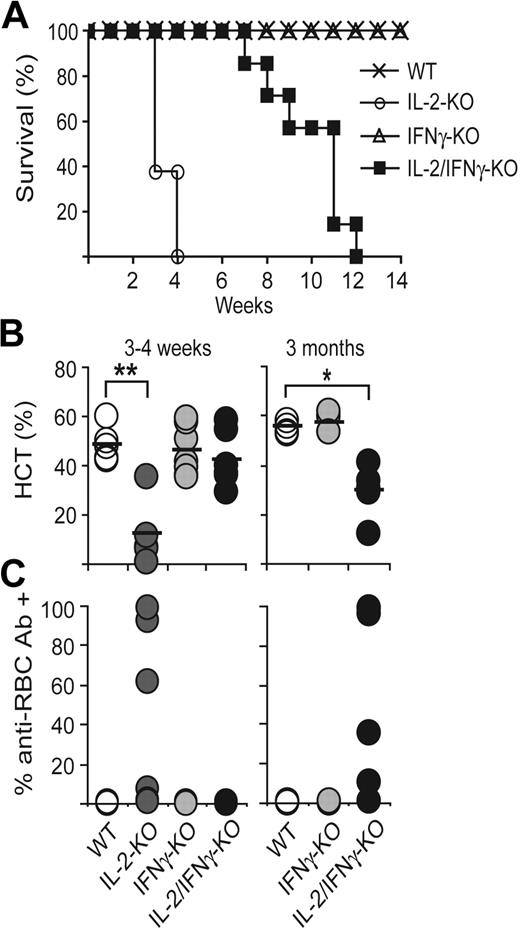
Absence of IFN-γ delays AIHA development and allows intestinal inflammation
To determine whether IFN-γ is critical for the development of AIHA, we crossed the IL-2–KO mice with mice lacking IFN-γ. Survival curves of WT, IL-2–KO, IFN-γ–KO, and IL-2/IFN-γ–KO mice showed that elimination of IFN-γ from IL-2–KO mice increased the median survival to 2.5 months from 3 to 4 weeks for the IL-2–KO mice (Figure 2A). Similar survival results were observed in IL-2–KO mice given a monoclonal antibody against IFN-γ beginning on day 7 after birth, when the T cells are known to be in a resting state (data not shown). Complete blood counts (including RBC counts, hematocrit, and hemoglobin measurements) indicated that IL-2–KO mice developed anemia at 19 to 27 days, whereas in IL-2/IFN-γ–KO mice anemia was markedly delayed, beginning at 2 to 3 months, and less severe (Figure 2B). IL-2–KO mice also developed anti-RBC antibodies at 19 to 27 days, whereas IL-2/IFN-γ–KO mice did not produce detectable anti-RBC antibodies until 60 to 90 days (Figure 2C). As expected, elimination of IFN-γ in IL-2–KO mice markedly reduced serum IgG2a levels at 3 to 4 weeks and at 3 months, whereas IgG1 levels remained elevated at all time points (data not shown). Thus, IFN-γ is required for early autoantibody production; however, even in its absence, pathogenic autoantibodies are ultimately produced if Th cells are profoundly dysregulated.
Elimination of IFN-γ in IL-2–KO mice delays AIHA development but does not alter lymphoproliferation. (A) Survival plots of WT, IL-2–KO, IFN-γ–KO, and IL-2/IFN-γ–KO mice. (B) Hematocrits (HCT) were measured from peripheral blood. (C) RBCs were stained with anti–mouse IgG-FITC to detect bound anti-RBC antibodies. There are no live IL-2–KO mice at 3 months; therefore, no data for these mice are shown at the late time point. Circles represent individual mice; n = 4 to 7 mice per genotype and time point. *P < .001; **P < .005.
Elimination of IFN-γ in IL-2–KO mice delays AIHA development but does not alter lymphoproliferation. (A) Survival plots of WT, IL-2–KO, IFN-γ–KO, and IL-2/IFN-γ–KO mice. (B) Hematocrits (HCT) were measured from peripheral blood. (C) RBCs were stained with anti–mouse IgG-FITC to detect bound anti-RBC antibodies. There are no live IL-2–KO mice at 3 months; therefore, no data for these mice are shown at the late time point. Circles represent individual mice; n = 4 to 7 mice per genotype and time point. *P < .001; **P < .005.
In addition to developing AIHA, IL-2–KO mice also develop a lymphoproliferative disorder, which is marked by the accumulation of activated cells in the LN and spleen (Figure S2A). IL-2/IFN-γ–KO T cells were activated and showed an increase in cell number as early as 3 weeks, similar to the expansion of IL-2–KO T cells, with a large percentage of CD4+ cells expressing decreased CD62L and elevated CD69 and CD44 (Figure S2B). Therefore, although the development of autoimmune manifestations is greatly retarded in IL-2/IFN-γ–KO mice, their lymphocyte populations are expanded and activated with kinetics similar to those of IL-2–KO mice. It is noteworthy that eliminating IFN-γ delays autoantibody production, even in the presence of massively expanded Th lymphocytes, emphasizing the critical role of the Th1 response in production of pathogenic autoantibodies.
To determine why the IL-2/IFN-γ–KO mice died at 2 to 3 months, we performed necropsies on these animals. The mice exhibited intestinal bleeding and rectal prolapse beginning at 6 to 10 weeks. At autopsy, these mice typically showed a rigid, inflamed colon and small intestine, and rectal prolapse. Microscopic examination of IL-2/IFN-γ–KO mice showed evidence of extensive inflammation of the distal colon with ulceration (Figure 3). Semi-quantitative real-time PCR evaluation of the descending colon shows elevated mRNA levels of IL-17A and IL-17F in IL-2–KO and IL-2/IFN-γ–KO mice, and elevated IFN-γ only in IL-2–KO mice, indicating that cells within the colon express elevated levels of these cytokine transcripts. It is probable that death in the IL-2/IFN-γ–KO mice is secondary to T cell–mediated intestinal inflammation.
Colitis development in IL-2/IFN-γ–KO mice. Hematoxylin and eosin stains of the descending colon from 27-day-old IL-2–KO (A) and IFN-γ–KO (B) mice, and a 72-day-old IL-2/IFN-γ–KO (C) mouse with a prolapsed rectum. Arrow indicates area of ulceration and underlying inflammation. (D) Cytokine RNAs were examined in the descending colon by real-time PCR. Data were normalized to HPRT and WT was set to 1.
Colitis development in IL-2/IFN-γ–KO mice. Hematoxylin and eosin stains of the descending colon from 27-day-old IL-2–KO (A) and IFN-γ–KO (B) mice, and a 72-day-old IL-2/IFN-γ–KO (C) mouse with a prolapsed rectum. Arrow indicates area of ulceration and underlying inflammation. (D) Cytokine RNAs were examined in the descending colon by real-time PCR. Data were normalized to HPRT and WT was set to 1.
Finally, young mice lacking IL-2 or both IL-2 and IFN-γ show approximately a 50% reduction in the frequency of Foxp3+ T cells in peripheral lymphoid organs (Figure S3). Thus, IFN-γ does not affect the Treg defect in IL-2–KO mice. However, Treg percentages decrease progressively with age in the IL-2/IFN-γ–KO mice. This decrease in Treg percentage over time, combined with expansion of self-reactive T cells, probably allows ongoing inflammation in the intestine.
IFN-γ–induced increase in macrophage phagocytosis in the absence of IL-2
We also asked whether IFN-γ was contributing to the development of AIHA in ways other than its role in autoantibody production. Macrophage function is enhanced by cytokines, including IFN-γ.19 Because AIHA is an autoantibody-mediated disease in which opsonized RBCs are cleared by phagocytes, we hypothesized that the IL-2/IFN-γ–KO mice may exhibit reduced phagocytosis of opsonized RBCs. To evaluate phagocytic activity, we purified splenic macrophages and assessed their ability to ingest FITC-conjugated E coli particles with or without LPS stimulation. Nonstimulated splenic macrophages from IL-2–KO mice demonstrated a 2- to 6-fold increased uptake of E coli particles compared with WT, IFN-γ–KO, or IL-2/IFN-γ–KO macrophages (Figure 4; P < .05). Upon stimulation, the macrophages from all mice increased their capacity to phagocytose particles. However, in the absence of IFN-γ, phagocytosis was markedly reduced compared with IL-2–KO macrophages (P = .06). Thus, both decreased autoantibody production and decreased phagocytosis probably contribute to the delay in AIHA disease resulting from IFN-γ elimination.
IL-2–KO macrophages have augmented phagocytosis activity. Splenic macrophages were seeded into tissue-culture plates overnight with and without LPS simulation. (A) Representative experiment showing E coli particle uptake by nonstimulated CD11b+ macrophages. The number in parentheses represents the mean fluorescent intensity (MFI). (B) Ratio of the MFI of E coli particle uptake by CD11b+ cells relative to nonstimulated WT cells is shown. Bar graph represents the mean plus or minus SD of 5 independent experiments. E coli particle uptake by unstimulated IL-2–KO CD11b+ cells is statistically different from all other genotypes (P < .05).
IL-2–KO macrophages have augmented phagocytosis activity. Splenic macrophages were seeded into tissue-culture plates overnight with and without LPS simulation. (A) Representative experiment showing E coli particle uptake by nonstimulated CD11b+ macrophages. The number in parentheses represents the mean fluorescent intensity (MFI). (B) Ratio of the MFI of E coli particle uptake by CD11b+ cells relative to nonstimulated WT cells is shown. Bar graph represents the mean plus or minus SD of 5 independent experiments. E coli particle uptake by unstimulated IL-2–KO CD11b+ cells is statistically different from all other genotypes (P < .05).
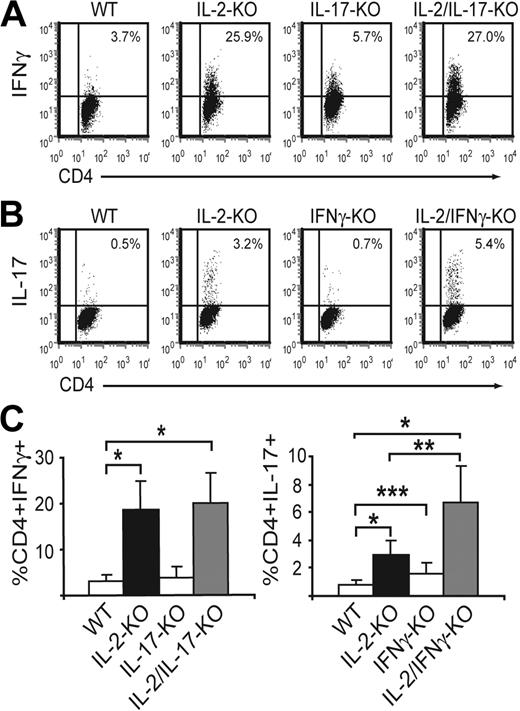
Cytokine production by CD4+ T cells
Because IFN-γ and IL-17 appear to be reciprocally regulated in some disease models, such as antigen-induced arthritis,20 and during mycobacterium infection of IFN-γ–KO mice,21 we evaluated cytokine production by CD4+ T cells from WT, IL-2–KO, IL-2/IFN-γ–KO, and IL-2-IL-17–KO mice after PMA and ionomycin stimulation for 5 hours ex vivo (Figure 5). Both IL-2–KO and IL-2/IL-17–KO CD4+ T cells produced comparably elevated levels of IFN-γ relative to WT or IL-17–KO CD4+ T cells. IL-2–KO CD4+ T cells expressed elevated IL-17 levels. Strikingly, elimination of IFN-γ from IL-2–KO mice increased IL-17 production relative to IL-2–KO alone. Finally, IFN-γ–KO CD4+ T cells also produced higher levels of IL-17 compared with WT CD4+ T cells, but IL-17 production in IFN-γ–KO CD4+ T cells was lower than in IL-2–KO CD4+ T cells. Thus, both IL-2 and IFN-γ inhibit Th17 responses, whereas IL-17 does not appear to reciprocally suppress the Th1 response.
Altered IL-17 and IFN-γ production in CD4+ T cells. Mesenteric LN cells from 3- to 4-week-old mice were stimulated with 50 ng/mL PMA and 500 ng/mL ionomycin for 5 hours, and cytokine-producing CD4+ T cells were measured by intracellular staining. (A) FACS profiles are representative data from one experiment. (B) Bar graphs represent mean plus or minus SD of 5 to 8 mice from 3 or 4 independent experiments. *P < .001; **P < .005; ***P < .05.
Altered IL-17 and IFN-γ production in CD4+ T cells. Mesenteric LN cells from 3- to 4-week-old mice were stimulated with 50 ng/mL PMA and 500 ng/mL ionomycin for 5 hours, and cytokine-producing CD4+ T cells were measured by intracellular staining. (A) FACS profiles are representative data from one experiment. (B) Bar graphs represent mean plus or minus SD of 5 to 8 mice from 3 or 4 independent experiments. *P < .001; **P < .005; ***P < .05.
Because IL-17 is elevated in IL-2/IFN-γ–KO mice, we next sought to determine the mechanism of increased IL-17 production. The transcription factors ROR-γt and ROR-α promote Th17 cell differentiation,22,23 whereas IL-23R and IL-1R1 are both up-regulated on Th17 cells.24-26 IL-21 is produced by Th17 cells and promotes the differentiation of these cells.26 We evaluated the expression of these genes by RT-PCR in mesenteric LN CD4+ T cells from 21-day-old mice, with and without stimulation by PMA and ionomycin. IL-17A, IL-17F, and IL-21 mRNA levels were elevated in IL-2–KO CD4+ T cells compared with WT, and further elevated in IL-2/IFN-γ–KO CD4+ T cells (Figure S4). In contrast, there was no difference in the mRNA levels of ROR-γt, ROR-α, IL-23R, or IL-1R1 between WT, IL-2–KO, IFN-γ–KO, or IL-2/IFN-γ–KO CD4+ T cells (data not shown). These data suggest that, by day 21, when cells from IL-2–KO and IL-2/IFN-γ–KO mice are activated and expanded, these transcription factors and cytokine receptors may not be involved in the elevated production of IL-17. Instead, it is possible that elevated IL-21 levels function to maintain the differentiation of Th17 cells at this stage of disease.
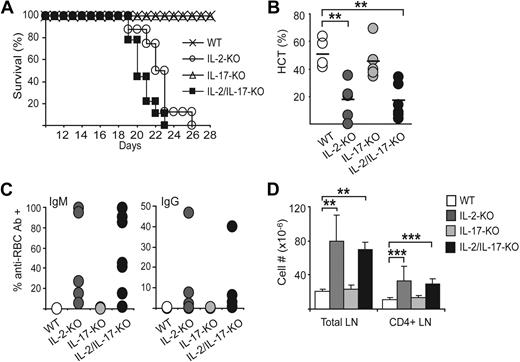
IL-17 plays no role in AIHA but may be involved in colitis development
To evaluate the role of IL-17 in this autoimmune disease, we crossed IL-2–KO mice with mice lacking IL-17A. Survival studies indicate that IL-2/IL-17–KO mice die between 19 and 23 days (Figure 6A), similar to the IL-2–KO mice. IL-2/IL-17–KO mice also demonstrated the hallmarks of AIHA development seen in IL-2–KO mice. RBC numbers and hematocrit and hemoglobin levels were decreased in IL-2/IL-17–KO mice, similar to levels found in IL-2–KO mice (Figure 6B). IL-2/IL-17–KO mice developed anti-RBC antibodies both bound to the RBCs and free in the serum beginning at 19 days, as is seen in IL-2–KO mice (Figure 6C; and data not shown). The percentage of RBCs coated with antibodies and the titer of antibodies were similar between IL-2–KO and IL-2/IL-17–KO mice. Elimination of IL-17 from IL-2–KO mice did not alter the elevated levels of IgG2a and IgG1 found in IL-2–KO serum. In both mice, IgG2a and IgG1 levels were elevated (data not shown).
IL-17 is not critical for AIHA development in IL-2–KO mice. (A) Survival plots of WT, IL-2–KO, IL-17–KO, and IL-2/IL-17–KO mice. (B) Hematocrit (HCT) values were measured from terminal blood draws. (C) RBCs were stained with anti–mouse IgM or IgG-FITC to evaluate the level of bound anti-RBC antibodies. (D) Bar graphs represent the number (×10−6) of total LN and CD4+ T cells at 3 to 4 weeks. Circles represent individual mice. Bar graphs represent mean plus or minus SD; n = 5 to 9 mice per genotype and time point. **P < .005; ***P < .05.
IL-17 is not critical for AIHA development in IL-2–KO mice. (A) Survival plots of WT, IL-2–KO, IL-17–KO, and IL-2/IL-17–KO mice. (B) Hematocrit (HCT) values were measured from terminal blood draws. (C) RBCs were stained with anti–mouse IgM or IgG-FITC to evaluate the level of bound anti-RBC antibodies. (D) Bar graphs represent the number (×10−6) of total LN and CD4+ T cells at 3 to 4 weeks. Circles represent individual mice. Bar graphs represent mean plus or minus SD; n = 5 to 9 mice per genotype and time point. **P < .005; ***P < .05.
In addition to developing AIHA, IL-2/IL-17–KO mice also developed a lymphoproliferative disorder similar to that found in IL-2–KO mice. Lymphoproliferation was observed by an increase in the accumulation of activated cells in the LN and spleen. The increase in total lymphocytes was the result of an expansion of CD4+ and CD8+ T cells and B cells (Figure 6D; and data not shown). Lymphocytes were activated as indicated by an increased percentage of CD44-high and CD62L-low CD4+ T cells (data not shown). Finally, mice lacking IL-2, or IL-2 and IL-17, show a similar reduction in the number of Foxp3+ T cells in peripheral lymphoid organs (data not shown), indicating that IL-17 does not affect the Treg defect. Together, these data demonstrate that IL-17 is not required for the development of the early lethal, autoantibody-mediated systemic autoimmunity occurring in the absence of IL-2 and Tregs. Elevated IL-17 may be important in the tissue-mediated autoimmunity and inflammation found in the IL-2/IFN-γ–KO mice. However, the IL-2/IL-17–KO mice die from AIHA at an early age and do not survive long enough to develop colitis.
Discussion
AIHA is a disease caused by autoantibodies against several antigens expressed on the surface of RBCs. Once formed, these autoantibodies bind to the surface of RBCs marking them for destruction through Fc-mediated phagocytosis and complement-mediated lysis. AIHA can occur alone but is most often seen in association with other autoimmune diseases, cancer, drug treatment regimens, transfusion, and pregnancy. Although the incidence of AIHA is relatively low at 1 in 80 000 (∼ 3400 people in the United States every year), this disease produces a life-threatening anemia of rapid onset, leading to its high mortality rate of 11.2%.27 Thus, it is a serious systemic autoimmune disease for which there are no workable therapies other than splenectomy and general immunosuppressive and anti-inflammatory drugs.
AIHA is often observed as a first sign of general autoimmunity in humans. Although there is no analogous human example of complete IL-2 deficiency, there are many human diseases (including systemic lupus erythematosus, multiple sclerosis, Crohn, and diabetes28-32 ) in which autoimmunity is attributed to decreased regulatory T-cell numbers or suppressive function, or a decrease in IL-2–receptor expression resulting from inherited genetic mutations.33,34 Mouse models of AIHA have demonstrated a critical role for Tregs in controlling AIHA,35 and a paucity of Treg numbers is thought to be one factor in AIHA onset in humans.36,37 Therefore, the decreased number of Tregs present in the IL-2–KO mouse mimics what is found in human AIHA. In addition, AIHA in humans is often associated with inflammatory diseases, resembling the lymphoproliferation seen in the IL-2–KO mouse. Thus, there is accumulating evidence that the IL-2–KO mouse model may provide valuable information relevant to human autoimmune disease, including AIHA.
Here we have demonstrated that AIHA is attributable to expanded CD4+ T cells of a Th1 phenotype, whereas lymphocyte infiltration and destruction of the intestine during colitis may be the result of IL-17–producing CD4+ T cells that emerge because of the decreased number of Tregs in the IL-2–KO mouse. Both Th1 and Th17 cells are expanded in the IL-2–KO mouse, suggesting that these mice might be prone to both AIHA and colitis development. However, IL-2–KO mice die of AIHA before the slower-manifesting intestinal inflammation develops into colitis. In the absence of IFN-γ, the IL-2–KO mice develop significantly delayed AIHA, allowing time for intestinal infiltration and subsequent inflammation in the presence of expanded IL-17–producing CD4+ T cells.
A contribution for Th1 cells in AIHA in IL-2–KO mice was clearly demonstrated in our study, as elimination of IFN-γ drastically delayed disease onset and severity, and mice eventually died of colitis. IFN-γ is required for the early, spontaneous activation of self-reactive lymphocytes in IL-2–KO mice. RBC-directed autoreactivity is significantly impaired in the absence of Th1-mediated proinflammatory cytokine production, at least partially through the loss of IgG2a antibodies and macrophage phagocytosis activities. Fossati-Jimack et al evaluated the pathogenicity of 4 IgG isotypes of one RBC autoantibody and demonstrated that the IgG2a isotype had the highest capacity to interact with the phagocytic receptors, FcγRI and FcγRIII, and was the most pathogenic in vivo.38 It is possible that the delay in AIHA in the IL-2/IFN-γ–KO mice is the result of the absence of IgG2a anti-RBC autoantibodies. However, the late development of AIHA in the absence of IFN-γ suggests that Th1-independent antibody isotypes are also capable of destroying red cells, albeit less than the Th1-dependent IgG2a.
Inflammatory bowel disease, including ulcerative colitis and Crohn's disease, is a chronic inflammatory condition of the gastrointestinal tract. An association between AIHA and colitis is well documented, with a prevalence of 0.2% to 1.8% in patients with ulcerative colitis.39-41 As in AIHA, decreased Treg function or number is associated with development of colitis. In humans, there is an inverse correlation between active ulcerative colitis and the frequency of peripheral Tregs.42 In mouse models of colitis, adoptive transfer of Tregs can cure established intestinal inflammation.43 Finally, IL-2–KO mice on the C57BL/6 background are prone to both colitis and AIHA.4
It has been previously shown that IFN-γ plays a critical role in lymphocyte and macrophage infiltration into the liver and intestine.44-46 Our data indicate that IFN-γ is not required for intestinal inflammation as has been observed in dextran sulfate sodium-induced colitis and other mouse models of autoimmune disease.43,46 Instead, in our system, lymphocytes infiltrate the intestine in the absence of IFN-γ, bypassing the need for this Th1 cytokine, possibly because of the massive lymphoproliferation and T-cell activation in IL-2–KO mice.
Whereas a large percentage of CD4+ T cells in the IL-2–KO mice were Th1 cells, there was also a distinct population of cells producing IL-17. Th17 cells have been shown to be potent inducers of tissue inflammation, and dysregulated IL-17 plays a role in the induction of collagen-induced arthritis,13 experimental autoimmune encephalomyelitis,47 and colitis,11 but has not been previously evaluated in the autoimmune disease found in IL-2–KO mice. It has been found recently that IL-2 inhibits Th17 differentiation, and Th17 CD4+ T-cell polarization is promoted in the absence of IL-2.48 Therefore, in the IL-2–KO autoimmune model, Th17 differentiation is probably promoted by an absence of IL-2 and a lack of regulation because of the reduction in Tregs relative to effector cells.
IL-17–producing cells are not required for the induction or maintenance of AIHA in IL-2–KO mice. Our data demonstrate that AIHA is still induced at similar kinetics in the absence of IL-17. Neither the rate of induction nor the severity of disease was altered in our model. Thus, our data indicate that IFN-γ, but not IL-17, is required for the early induction of AIHA. So although IL-17 cells are present in expanded numbers in the IL-2–KO mice, these cells are not playing a role in the development of AIHA. We suggest that, instead, the expanded Th17 population in the IL-2–KO mice probably contributes to the other inflammatory and autoimmune manifestations present in the IL-2–KO mice. It has been previously demonstrated that IFN-γ inhibits Th17 differentiation in vitro, and supporting this idea in vivo, elimination of IFN-γ in the IL-2–KO mice resulted in a further increase in Th17 CD4+ T cells producing IL-17. We found that, contrary to our expectations, ROR-γt, ROR-α, IL-23R, and IL-1R1 mRNA levels were not elevated in CD4+ T cells from IL-2–KO or IL-2/IFN-γ–KO mice despite increased IL-17 production by these cells. It remains possible that these transcription factors and cytokine signaling pathways are important in the initiation of Th17 differentiation in these mice; however, once the CD4+ T cells are already activated, expanded and producing elevated levels of IL-17, these genes are no longer involved in the maintenance of IL-17 production. Instead, we suggest that elevated IL-21 production functions to promote Th17 differentiation and IL-17 production during this stage of disease in the IL-2–KO and IL-2/IFN-γ–KO mice.
IL-2/IFN-γ–KO develop intestinal inflammatory bowel disease with elevated IL-17A and IL-17F mRNA levels found in the descending colon, suggesting that the expanded Th17 population may be important in initiating or propagating the intestinal inflammation in these animals. We suggest that IFN-γ induces AIHA, whereas IL-17 contributes to tissue-specific inflammation and autoimmunity (colitis) in the absence of IL-2 and Tregs.
Taken together, the Treg deficiency caused by IL-2 deletion leads to a systemic autoimmune disease which, in the BALB/c strain, is dominated by an acute autoantibody-mediated hemolytic anemia. The key determinant of this disease manifestation is an uncontrolled Th1 response that is eliminated when IFN-γ is removed. IFN-γ promotes the production of opsonizing anti-RBC antibodies and stimulates the phagocytic activity of splenic macrophages, both actions probably contributing to AIHA. If IFN-γ is deleted, a slower disease develops in which colitis is a prominent feature. This lesion is associated with enhanced IL-17 production, suggesting that the tissue inflammation is caused by Th17 cells. Thus, different manifestations of systemic autoimmunity in this mouse model are probably attributable to dysregulated production of different cytokines.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Drs Jeff Bluestone, Mark Anderson, and Cliff Lowell and members of the Abbas laboratory for helpful discussions, Dr Jean Olson and Christine Lin for assistance with microscopy, Dr Alejandro Villarino for RT-PCR primer sequences, Shu-wei Jiang for cell sorting, and Carlos Benitez for mouse typing.
This work was supported by the National Institutes of Health (grants P01AI35297 and R01AI073656).
National Institutes of Health
Authorship
Contribution: K.K.H. designed and performed research, analyzed data, generated figures, and wrote the manuscript; W.F.K. and E.G. performed research; and A.K.A. supervised the research design and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Abul K. Abbas, Department of Pathology, University of California San Francisco, M-590, 505 Parnassus Avenue, San Francisco, CA 94143; e-mail: abul.abbas@ucsf.edu.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal