Abstract
Peripheral blood and tissue eosinophilia are a prominent feature in allergic diseases and during helminth infections. Eosinophil recruitment also frequently occurs upon mycobacterial infections, particularly in lung granuloma. However, the mechanism by which eosinophils interact with mycobacteria remains largely unknown. Because eosinophils recently have been shown to be involved in innate immune responses, we investigated the direct interactions of eosinophils with Mycobacterium bovis BCG as a study model. We show that live BCG attracts human eosinophils and induces reactive oxygen species (ROS) synthesis, granule protein release, and tumor necrosis factor (TNF)–α secretion. Using anti-TLR2 neutralizing antibodies before exposure of eosinophils to BCG, we showed a critical role of TLR2 signaling in ROS and eosinophil peroxidase release. BCG-induced eosinophil activation is mediated through the p38 mitogen-activated protein (MAP) kinase and nuclear factor (NF)–κB pathways. In addition, a mycobacterial wall component, lipomannan, induced a TLR2-dependent eosinophil activation. In addition, we showed that eosinophils express and produce α-defensins upon stimulation with BCG and lipomannan and that α-defensins could inhibit mycobacterial growth in synergy with eosinophil cationic protein. These results suggest a role for human eosinophils as direct effectors in TLR2-mediated innate immunity against mycobacteria and confer to these cells potent cytotoxic functions through defensin and eosinophil cationic protein production.
Introduction
Tuberculosis is the most prevalent infectious disease worldwide, accounting for 3 million deaths annually. Control of Mycobacterium tuberculosis bacillus (MTB) infection requires the development of a Th1-type CD4 T-cell response and activation of alveolar macrophages, leading to the formation of lung granuloma.1 Initial recognition of mycobacteria by the innate immune system through pathogen recognition receptors (PRRs) such as Toll-like receptors (TLRs) contributes to triggering this adaptive immune response.2 Indeed, cooperation between TLR2, TLR4, and TLR9 may contribute to resistance against mycobacteria,3 and the authors of several studies have shown that mycobacterial components act as TLR agonists. Indeed, lipomannans (LM) and lipoarabinomannans (LAM), lipoglycans that ubiquitously are found in the wall of mycobacteria, are involved in the release of proinflammatory or anti-inflammatory cytokines.4
Whereas mycobacterial infections are rather associated to Th1 responses, the occurrence of Th2 cytokine responses also has been reported in human tuberculosis. It is suggested that these Th2 responses might depress macrophage immunity and lead to increased susceptibility to tuberculosis.5 Th2-driven immunity is associated with cell types that seldom are studied during mycobacterial infections. Among them, eosinophils, which are now considered as multifunctional leukocytes, are involved in inflammatory processes as well as in modulation of innate and adaptive immunity.6 Indeed, besides the well-known involvement of eosinophils in helminth infections, evidence is scant of their role in defenses against other pathogens, such as virus, fungi, or bacteria.7,8 Eosinophilia has been associated with pulmonary tuberculosis in patients with human immunodeficiency virus-1 (HIV-1)9 and in patients with concomitant intestinal helminth infections.10 Moreover, tissue eosinophilia also has been observed after the Bacillus Calmette-Guérin (BCG) vaccination at the site of tuberculin injection.11 Eosinophil recruitment within mycobacterial granuloma has been found in different animal models.12-18
Eosinophils are potent effector cells as the result of the release of several cytotoxic mediators upon activation. Cytoplasmic-specific granules contain high amounts of cytotoxic proteins, in particular cationic proteins (major basic protein [MBP], eosinophil cationic protein [ECP], eosinophil peroxidase [EPO], and eosinophil-derived neurotoxin [EDN]).19 Cytotoxic potential of eosinophils also arises from their ability to mount a respiratory burst, including superoxide and H2O2 production, which in turn initiates production of more potent oxidants.20,21 Beside cytotoxic mediators, eosinophils not only express and secrete Th2 cytokines such as interleukin (IL)–4, IL-5, and IL-10 but also Th1 and proinflammatory cytokines such as interferon (IFN)–γ22 and tumor necrosis factor (TNF)–α, which typically are released after MTB infection.
Although eosinophils accumulate at sites of mycobacterial infection, their activation and their involvement in the regulation of bacterial growth have not been investigated. In the present study, we used, the BCG strain derived from Mycobacterium bovis as a model to delineate the potential interactions between eosinophils and mycobacteria.
Methods
Eosinophil and neutrophil purification
In accordance with French law for studies involving human biologic samples, blood from healthy and eosinophilic donors was collected after informed consent from volunteers, in accordance with the Declaration of Helsinki, and approval from the Comité Consultatif des Personnes dans la Recherce Biomédicale de Lille (Consultative Committee for Persons in Biomedical Research from Lille; CCPPRB). Eosinophils were isolated from peripheral blood of healthy, allergic, and hypereosinophilic donors.23 Eosinophils were separated from peripheral blood mononuclear cells (PBMCs) by Percoll (GE Healthcare, Little Chalfont, United Kingdom) centrifugation then purified by magnetic selection using immunomagnetic anti-CD16 (Miltenyi Biotec, Bergisch Gladbach, Germany). Eosinophil purity was checked by cytocentrifugated preparations after RAL555 coloration and was found to be greater than 98%. Neutrophils were collected in the positive fraction (purity was > 99%).
M bovis BCG
The M bovis BCG Pasteur strain was obtained from Dr C. Locht (Inserm U629, Institut Pasteur de Lille, France) and maintained at 37°C in Sauton liquid medium. Viable mycobacteria M bovis BCG in logarithmic growth phase were used at concentrations indicated in the figure legends. One absorbance unit at 600 nm for the BCG culture was calculated as 2 × 107 colony-forming units (CFUs). Heat-killing was conducted by the culture of BCG at 70°C for 1 hour.
Lipomannan and lipoarabinomannan from M bovis BCG were purified as previously described.24 Endotoxin contamination of each preparation was determined by the chromogenic Limulus lysate assay (QCL1000; Cambrex Biosciences, Walkersville, MD) and were less than 1 pg/mL in all experiments.
Migration assays
The ability of BCG to induce cell migration was measured by Transwell assay (Costar, High Wycombe, United Kingdom). Eosinophils were first labeled with 10 μmol/L carboxyfluorescein diacetate succimidyl ester (CFSE; Molecular Probes, Eugene, OR) and suspended at 3 × 106 cells/mL in RPMI 1640 (Invitrogen, Carlsbad, CA) with 1% fetal bovine serum (FBS). BCG, LAM, or LM were placed in various concentrations in the lower wells and separated from eosinophils by a polycarbonate filter (pore size 5 μm; Corning, Corning, NY). Migration toward IL-5 (10 ng/mL; Peprotech, Rocky Hill, NJ) was used as positive control. Migration was conducted for 3 hours at 37°C in a humidified 5% CO2 incubator. The number of migrated eosinophils was determined on a FACSCalibur flow cytometer with the CellQuest software (Becton Dickinson).
Release of reactive oxygen species and eosinophil degranulation
A luminol-dependent chemiluminescence system was used to determine eosinophilic production of reactive oxygen species (ROS). In brief, 3 × 105 eosinophils resuspended in RPMI 1640 medium without phenol red (Invitrogen) were activated with stimulus such as BCG, Pam3CSK4, or ultrapure LPS from Escherichia coli 0111:B4 (Invivogen, San Diego, CA). Luminol (25 μg/mL in Tris-HCl 0.01 mol/L, pH 7.4; Sigma-Aldrich, St Louis, MO) was added, and chemiluminescence was immediately measured with a luminometer (Victor Wallac; PerkinElmer, Waltham, MA). Kinetic measurement was performed at 37°C during the course of 2 hours and chemiluminescence was counted for 5 seconds.
To detect EPO, eosinophils (2 × 105 cells in 100 μL) were incubated for 2 hours in RPMI 1640 without phenol red, with stimuli at 37°C in 5% CO2. EPO activity in eosinophil supernatants (50 μL) was measured by the oxidation of H2O2 by luminol (200 μg/mL in Tris-HCl 0.01 mol/L, pH 6). The reaction was amplified by the addition of D-luciferin (160 μM in Tris-HCl 0.01 mol/L, pH 6; Sigma-Aldrich) before chemiluminescence was measured.
For inhibition experiments, eosinophils were preincubated with blocking anti-TLR2 monoclonal antibody (mAb; TL2.1, Alexis, Lausen, Switzerland); blocking anti-TLR4 mAb (HTA125; eBioscience, San Diego, CA); total anti–mouse (mIgG) isotype control (Jackson ImmunoResearch Laboratories, West Grove, PA); MyD88 homodimerization inhibitory peptide (DRQIKIWFQNRRMKWKKRDVLPGT) or peptide control (DRQIKIWFQNRRMKWKK; Imgenex, San Diego, CA); SP 600125, c-Jun N-terminal kinase (JNK) inhibitor (Alexis); PD 98 059, ERK kinase inhibitor (Alexis), SB 203580, p38 MAP kinase (Invitrogen); or BAY 11-7082, NF-κB inhibitor (Calbiochem, San Diego, CA) for 30 minutes at 37°C before the addition of stimulus.
ECP, TNF-α, and α-defensin release
Eosinophils (2 × 106 cells/mL) were activated with the same stimuli as for ROS production. After 18 hours of culture, supernatants were collected. ECP, TNFα, and α-defensin were measured by specific enzyme-linked immunoassay (ELISA) kits from MBL International (Woburn, MA), Diaclone (Wythenshawe, Manchester, United Kingdom), and HyCult Biotechnology (Uden, The Netherlands), respectively. The lower detection limit was 0.125 ng/mL for ECP, 8 pg/mL for TNF-α, and 50 pg/mL for human α-defensins.
Flow cytometric analysis
Human eosinophils (2 × 106/mL) were stimulated for 2 hours in RPMI 1640 with or without BCG as indicated in the figure legends. Cell-surface staining was performed with PE-TLR2 (TL2.1) or PE-TLR4 (HTA125) mAb (eBioscience) or the matched isotype control mPE-IgG2a (Immunotech, Praha, Czech Republic). For intracellular staining, purified eosinophils or neutrophils were first fixed with 2% paraformaldehyde and then permeabilized with 0.01% saponin in phosphate-buffered saline (PBS). Nonspecific binding was blocked with mouse serum for 10 minutes, and the cells were incubated with a mouse anti–HNP1-3 (D21; Hycult Biotechnology) or IgG1 isotype control (Diaclone) for 30 minutes in 0.01% saponin buffer. After washing, cells were incubated with a goat fluorescein isothiocyanate (FITC)–anti–mouse IgG1 secondary antibody (Southern Biotechnology Associates, Birmingham, AL) for 20 minutes. Cells were then immediately analyzed on a FACSCalibur.
Immunofluorescence labeling
Eosinophil-cytocentrifugated preparations were performed, and the cells were fixed in 4% paraformaldehyde and rehydrated in 0.05 mol/L PBS, pH 7.4. Cytospins were washed 3 times in PBS-0.1% bovine serum albumin (BSA). Eosinophils were permeabilized in PBS-1% BSA-0.2% Triton X-100 for 5 minutes on ice. Endogenous fluorescence was blocked by 50 mM NH4Cl, pH 7.4, for 15 minutes. Cells were then incubated with PBS-3% BSA for 30 minutes to prevent nonspecific binding. Cytospins were then incubated overnight at 4°C with mouse anti–HNP1-3 (D21; Hycult Biotechnology) or a mouse IgG1 isotype control (Diaclone) in PBS-3% BSA-5%HSA. Cytospins were blocked using goat serum (30 minutes) and Alexa Fluor 555 goat anti–mouse secondary antibodies (Invitrogen) was added in PBS-3% BSA-5% HSA for 2 hours. Slides were then incubated with biotinylated mouse anti-EPO or anti-MBP (BD Pharmingen, San Diego, CA) for 2 hours. We detected immunoreactivity against EPO or MBP by staining slides with Alexa Fluor 488 streptavidin (Invitrogen) for 2 hours. Cytocentrifugated preparations were mounted with Fluoromount G (Southern Biotechnology Associates) and were examined by the use of a Zeiss AxioImager Z1 microscope and AxioVision software (Zeiss, Thornwood, NY). Fast iterative algorithm was used for deconvolution. Image editing and overlays were performed on Adobe Photoshop version 7.0 (Adobe, San Jose, CA).
For confocal microscopy, we acquired images by using a DM-IRE2 inverted microscope with SP2-AOBS scan-head (Leica, Wetzlar, Germany) at the Imaging Facility of Institut Pasteur de Lille. Acquisitions were performed using a 100×/1.4 NA oil-immersion objective. Three-dimensional pretreatment, analysis, and addition were performed with Leica Confocal Software.
RNA isolation and RT-PCR amplification
Total RNA was isolated with the RNeasy mini kit (QIAGEN, Valencia, CA) from 107 purified cells following the protocol recommended by the manufacturer. Reverse transcription (RT) was performed with SuperScript-Reverse Transcriptase (200 U/μL) as described in the manufacturer's protocol (Invitrogen). cDNA were then amplified with the use of specific primers (Proligo; 20 pmoles/μL). MyD88: (5′-GACTTTGAGTACTTGGAGATCCGG-3′ and 5′-GATGGTGGTGGTTGTCTCTGATGA-3′), annealing temperature 56°C; Toll-interleukin-1 receptor domain-containing adapter protein (TIRAP; 5′-CTGGCTCTCGGCCTAAGAA-3′ and 5′-CATCGCTGGAGGTGCTTTC-3′), annealing temperature 60°C; TRAF6 (5′-GGTCCGGAATTTCCAGGAAA-3′ and 5′-CATTTTAGCAGTCAGCTCCCG-3′), annealing temperature 62°C); α-defensins (5′-CACTCCAGGCAAGAGCTGATGAGGT-3′ and 5′-CATCTACCAGGGAAGACTCTGGGCATT-3′), annealing temperature 64°C. Polymerase chain reaction assays (PCRs) were run for 40 cycles (1 minute at 95°C, 1 minute annealing, and 1 minute at 72°C) with the use of Taq polymerase (Bioprobe, Farmington, CT).
Western blot
Cell lysates were prepared from freshly isolated eosinophils or neutrophils (10 × 106 cells) in lysis buffer (20 mmol/L Tris-HCl, pH 8.0; 120 mol/L NaCl; 1% Triton X-100; 10 mmol/L ethylene diamine tetraacetic acid [EDTA]; 0.05% 2-mercaptoethanol; 1X protease inhibitors). Samples were analyzed on 12% sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) under reducing conditions. The proteins were electrotransferred to nitrocellulose membranes (Bio-Rad). Membranes were blocked with 5% milk in Tris-buffered saline with 0.05% Tween 20 for 1 hour at room temperature and probed with primary rabbit anti–human MyD88 antibody (Cell Signaling) at 4°C overnight. After washing, membranes were incubated with secondary anti–rabbit antibody coupled to horseradish peroxidase (Jackson ImmunoResearch Laboratories) for 1 hour at room temperature, followed by ECL Plus detection (Amersham Biosciences).
In assays determining phosphorylated forms of p38, eosinophils were incubated (2 × 106 cells in PBS) with different BCG/eosinophil ratios for 5, 15, and 30 minutes (37°C, 5% CO2). After stimulation, cells were lysed, and equal amounts of proteins were analyzed with monoclonal rabbit anti–human p38 mitogen-activated protein kinase (MAPK) or antiphosphorylated p38 MAPK antibodies (Cell Signaling). For α-defensin detection, proteins were subjected to SDS-10% PAGE before blotting onto a nitrocellulose membrane, as described previously.
Phagocytosis
Eosinophils were labeled with 10 μmol/L CFSE at 4 × 106 cells/mL in PBS. BCG were labeled with 10 μmol/L PKH26 (Sigma-Aldrich) at a concentration of 108 bacteria/mL. On the day of each experiment, CFSE-labeled eosinophils are incubated with PKH26-labeled BCG at different BCG/eosinophil ratios (5:1, 10:1, 20:1) in RPMI 1640 without phenol red and without serum at 37°C in 5% CO2. After selected incubation times, eosinophils were washed in RPMI to remove nonadherent mycobacteria and fixed in slide after cytospin for analyze. Cells containing fluorescent red mycobacteria were counted by fluorescence microscopy (Leica).
Bactericidal activity of eosinophils
Eosinophils were washed with RPMI without phenol red and diluted to 2.106 mL. Next, a bacterial suspension was diluted from the frozen aliquots in RPMI without phenol red to the appropriate concentration for use in experiments. BCG suspension was placed with the eosinophil suspension at 37°C for different times. Numbers of CFU were determined as follow: dilutions of each sample were plated in duplicates on 7H11 (Difco Laboratories, Detroit, MI) agar plates enriched with oleic acid albumin dextrose complex (OADC) and incubated at 37°C and 5% CO2. After 21 days, the number of CFUs was determined on the plates and expressed in percentage of CFU control ([CFU with eosinophils/CFU with medium] × 100).
For bactericidal activity against intracellular mycobacteria, BCG-infected eosinophils were washed 3 times with antibiotic-free medium. The low-speed centrifugation (300g) selectively pellets cells whereas extracellular bacteria remain in the supernatant. To measure intracellular mycobacterial growth, cells were lysed with 0.3% saponin (Sigma-Aldrich) to release intracellular bacteria. At all time points, an aliquot of unlysed infected cells was harvested and counted. This step allowed an exact quantification of cells as well as the determination of cellular viability by trypan blue exclusion. Recovery of cells was 80% in all experiments, with cell viability regularly exceeding 90% of total cells. Lysates of infected cells containing intracellular mycobacteria were resuspended vigorously, transferred into screw-cap tubes, and sonicated in a preheated (37°C) water bath sonicator for 5 minutes. Aliquots were diluted in Sauton medium and plated on Middlebrook 7H11 (Difco) agar. CFU were counted after 21 days' incubation at 37°C.
The bactericidal activity of purified α-defensins (Hycult Biotechnology) and ECP (Diagnostics Development, Uppsala, Sweden) against BCG was determined by measuring the effect on bacterial colony-forming activity.
For inhibition experiments, eosinophils were preincubated with a blocking anti-α-defensin (NP-1) antibody (MBL), anti-ECP (BD Pharmingen), or isotype control for 30 minutes at 37°C, before the addition of BCG.
Eosinophil granules
Purified eosinophils were lysed in ice-cold buffer (0.25 mol/L sucrose, 200 U/mL heparin). The residual cells and debris were separated from the granules by centrifugation at 300g for 10 minutes. The eosinophil granules were isolated from the supernatant by centrifugation at 10 000g for 15 minutes.
For detection of α-defensins by flow cytometer, eosinophil crystalloid granules were subjected to the same procedure described previously for purified eosinophils. Eosinophil granules were identified by incubation with biotinylated anti-EPO or isotype control for 30 minutes and, after a washing step, with streptavidin-APC (Molecular Probes) for 20 minutes in the presence of saponin.
Statistical analysis
All data were expressed as mean plus or minus SEM. All statistical analyses were performed with the use of SPSS software (SPSS Institute, Chicago, IL). Normality of data samples was assessed with the normality test of Shapiro and Wilk. The parametric Student t test for paired experiments was used to compare 2 variables. Analysis of variance (ANOVA) together with the Dunnett posttest were used for comparisons of more than 2 datasets. A P value of less than .05 was used to indicate statistical significance.
Results
M bovis BCG attracts and activates human eosinophils
In various models of mycobacterial infections, eosinophils are recruited into developing lesions.17,18 We first tested the ability of BCG to induce the migration of purified eosinophils. Chemotactic activity of BCG for eosinophils was assayed with the use of eosinophils alone (0:1) as negative control and recombinant human (rh) IL-5 as positive control. Compared with spontaneous migration, we found that eosinophils migrated significantly more toward live but not heat-killed BCG (Figure 1A). Eosinophil migration was dependent upon increasing BCG/eosinophil ratios. In addition, we observed that LAM and LM purified from M bovis BCG, known as major cell wall lipoglycans, induced a migratory response in human eosinophils in a dose-dependent manner in the range of concentrations from 0.01 to 10 μg/mL (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article).
Eosinophil chemotaxis and activation mediated by M bovis BCG. (A) Eosinophil migration in response to different BCG/eosinophil ratios. Error bars represent plus or minus SEM from 5 independent experiments. (B) ROS generation and EPO release by eosinophils in cell supernatants. Results are expressed as ΔROS or ΔEPO cps (counts per second) values (values from medium stimulation are subtracted from values obtained with each ratio). (C) After 18 hours of incubation, ECP concentrations in the cell-free supernatants were measured. Data are expressed as means plus or minus SEM from the 3 independent experiments with different eosinophil donors. (D) Eosinophils were stimulated for 18 hours at different BCG/ eosinophil ratios. TNF-α levels were quantified in the culture supernatants by ELISA. Results are represented as the mean of 3 independent experiments plus or minus SEM. *P < .05; **P < .01.
Eosinophil chemotaxis and activation mediated by M bovis BCG. (A) Eosinophil migration in response to different BCG/eosinophil ratios. Error bars represent plus or minus SEM from 5 independent experiments. (B) ROS generation and EPO release by eosinophils in cell supernatants. Results are expressed as ΔROS or ΔEPO cps (counts per second) values (values from medium stimulation are subtracted from values obtained with each ratio). (C) After 18 hours of incubation, ECP concentrations in the cell-free supernatants were measured. Data are expressed as means plus or minus SEM from the 3 independent experiments with different eosinophil donors. (D) Eosinophils were stimulated for 18 hours at different BCG/ eosinophil ratios. TNF-α levels were quantified in the culture supernatants by ELISA. Results are represented as the mean of 3 independent experiments plus or minus SEM. *P < .05; **P < .01.
In response to activation, eosinophils are able to synthesize ROS and to mobilize preformed proteins stored within cytoplasmic-specific granules and to produce cytokines.6 We have examined ability of BCG to induce ROS generation by eosinophils. The peak of eosinophil respiratory burst was reached approximately 30 minutes after BCG addition for eosinophilic patients and 60 minutes for normal donors (Figure S2A). At this time point, ROS production by eosinophils was proportional to BCG number (Figure 1B). BCG-induced eosinophilic degranulation also was evaluated by EPO release in supernatants. Dose-dependent EPO release was observed when eosinophils were incubated with increasing BCG/eosinophil ratios (Figure 1B). In addition, weak ROS and EPO release was observed when heat-killed BCG was added (data not shown). Similar results were found for ECP, confirming that BCG triggers eosinophilic degranulation in a dose-dependent manner (Figure 1C).
Because several cytokines also are stored in eosinophil granules, we evaluated the capacity of BCG to induce TNF-α release, a key cytokine participating in the control of mycobacterial infection as well as in granuloma formation.25,26 TNF-α was detected in supernatants from eosinophils incubated for 18 hours with different numbers of BCG (Figure 1D). Furthermore, several chemokines and cytokines, including IL-8, migration inhibition factor (MIF), macrophage inflammatory protein (MIP)-1α, MIP-1β, IL-13, and IL-16, were detected by protein microarray in cell-free supernatants of eosinophils after incubation with BCG (Figure S2B). Taken together, these results indicate that eosinophils can directly respond to BCG by degranulation and cytokine release.
Eosinophil expression of TLR2 and TLR4 is inducible
As reported for macrophages and dendritic cells, TLR2 and TLR4 have been identified as potential receptors for mycobacterial components.2 Expression of TLRs by eosinophils has been recently described recently27 but their precise expression profiles and functions still remain unclear. Herein, we have compared TLR expression by eosinophils from normal donors (NDs) and eosinophilic donors (EDs). Surprisingly, TLR2 and TLR4 were not detected on the surface of eosinophils from normal donors, in contrast to eosinophils from eosinophilic donors, which spontaneously expressed surface TLR2 and TLR4 (Figure 2A). Because TLR expression is known to be up-regulated in human monocytes treated with TLR agonists,28 we investigated whether BCG could also modulate surface expression of TLRs on eosinophils. For 16 healthy donors and eosinophilic donors studied (Table S1), BCG significantly increased TLR2 and TLR4 expression on freshly isolated human eosinophils from most donors (Figure 2A,B). These results show heterogeneous basal expression levels of TLR2 and TLR4 on human eosinophils and induction in vitro in the presence of BCG.
Expression of TLR2 and TLR4 by human eosinophils. (A) Surface expression of TLR2 and TLR4 on human eosinophils incubated with or without BCG (10:1). Results correspond to one representative normal donor (ND, no. 13 of Table S1) and eosinophilic donor (ED, no. 5 of Table S1). Gray histogram and black line represent staining with specific and isotype control antibodies, respectively. The data are displayed by using a logarithmic scale and the change in mean fluorescence intensity (ΔMFI: values from isotype control antibodies are subtracted from values obtained with each condition) are indicated in the plot. (B) Cell-surface TLR2 and TLR4 expressions on purified eosinophils from 16 individual eosinophil donors stimulated with or without BCG (10:1). Group average expression for the indicated markers is represented (−).*P < .05.
Expression of TLR2 and TLR4 by human eosinophils. (A) Surface expression of TLR2 and TLR4 on human eosinophils incubated with or without BCG (10:1). Results correspond to one representative normal donor (ND, no. 13 of Table S1) and eosinophilic donor (ED, no. 5 of Table S1). Gray histogram and black line represent staining with specific and isotype control antibodies, respectively. The data are displayed by using a logarithmic scale and the change in mean fluorescence intensity (ΔMFI: values from isotype control antibodies are subtracted from values obtained with each condition) are indicated in the plot. (B) Cell-surface TLR2 and TLR4 expressions on purified eosinophils from 16 individual eosinophil donors stimulated with or without BCG (10:1). Group average expression for the indicated markers is represented (−).*P < .05.
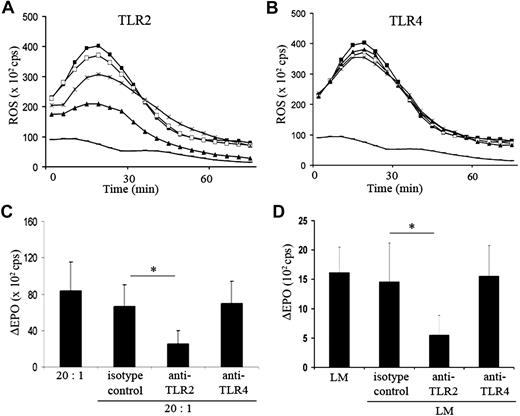
TLR2, but not TLR4, is essential in eosinophil activation by BCG
To further evaluate the functionality of TLRs on eosinophils, these latter were stimulated with either Pam3CSK4 (PAM) or lipopolysaccharide (LPS), respectively TLR2- and TLR4-specific ligands. As shown in Figure S3A, eosinophils from normal and eosinophilic donors released ROS and EPO in response to PAM and LPS and this release was inhibited by blocking anti-TLR2 and anti-TLR4 antibodies, confirming that TLR2 and TLR4 expressed by human eosinophils are functional.
Several reports have described TLR2- and TLR4-dependent activation of macrophages by mycobacterial ligands.29 To investigate the potential involvement of TLRs in eosinophil/BCG interactions, eosinophils were incubated with blocking anti-TLR2 and anti-TLR4 antibodies, and their response to BCG was evaluated by ROS release. Production of ROS in response to BCG was reduced in a dose-dependent manner when eosinophils were preincubated with a blocking anti-TLR2 antibody (with a maximum of 47.3% ± 11.9% inhibition; Figure 3A), whereas no significant inhibition of ROS release was observed with a blocking anti-TLR4 antibody or an isotype control (Figure 3B). Similar levels of inhibition of EPO release was obtained with blocking anti-TLR2 antibody but not with anti-TLR4 antibody (Figure 3C). These data indicate that TLR2, but not TLR4, is involved in eosinophil activation by BCG.
Involvement of TLR2 in the activation of eosinophils by M bovis BCG. (A) Kinetics of BCG-induced ROS release (ratio 10:1, ■) inhibited by an anti-TLR2 blocking antibody 20 μg/mL (▴), 10 μg/mL (*), or an isotype control antibody 20 μg/mL (□). Spontaneous ROS release by eosinophils is indicated (−). Results correspond to 1 representative of 3 experiments and are expressed in counts per second (cps). (B) BCG-induced ROS production (ratio 10:1, ■) inhibited by an anti-TLR4 blocking antibody 20 μg/mL (▴), 10 μg/mL (*), or an isotype control antibody 20 μg/mL (□). Spontaneous ROS release of eosinophils is indicated (−). Results are expressed as ROS cps values and one representative of 3 experiments was shown. (C) Inhibition of BCG-induced EPO release by anti-TLR2 and anti-TLR4 blocking antibodies (20 μg/mL) or an isotype control antibody. ΔEPO cps values (values from medium stimulation are subtracted from values obtained with each antibody). Results are expressed as mean plus or minus SEM (n = 5-6). (D) LM (1 μg/mL)–induced EPO release inhibited by anti-TLR2 or anti-TLR4 blocking antibodies (20 μg/mL) or an isotype control antibody. Results are expressed as ΔEPO cps values and as mean plus or minus SEM (n = 5). *P < .05.
Involvement of TLR2 in the activation of eosinophils by M bovis BCG. (A) Kinetics of BCG-induced ROS release (ratio 10:1, ■) inhibited by an anti-TLR2 blocking antibody 20 μg/mL (▴), 10 μg/mL (*), or an isotype control antibody 20 μg/mL (□). Spontaneous ROS release by eosinophils is indicated (−). Results correspond to 1 representative of 3 experiments and are expressed in counts per second (cps). (B) BCG-induced ROS production (ratio 10:1, ■) inhibited by an anti-TLR4 blocking antibody 20 μg/mL (▴), 10 μg/mL (*), or an isotype control antibody 20 μg/mL (□). Spontaneous ROS release of eosinophils is indicated (−). Results are expressed as ROS cps values and one representative of 3 experiments was shown. (C) Inhibition of BCG-induced EPO release by anti-TLR2 and anti-TLR4 blocking antibodies (20 μg/mL) or an isotype control antibody. ΔEPO cps values (values from medium stimulation are subtracted from values obtained with each antibody). Results are expressed as mean plus or minus SEM (n = 5-6). (D) LM (1 μg/mL)–induced EPO release inhibited by anti-TLR2 or anti-TLR4 blocking antibodies (20 μg/mL) or an isotype control antibody. Results are expressed as ΔEPO cps values and as mean plus or minus SEM (n = 5). *P < .05.
LAM and LM have been widely described as key factors able to modulate the host immune response.30 No ROS production by eosinophils was observed after incubation with LM or LAM purified from BCG (data not shown). However, both molecules induced release of EPO by eosinophils, with LM being a more potent EPO inducer than LAM (Figure S3B). This prompted us to investigate the ability of LM to activate eosinophils. As shown in Figure 3D, EPO release by eosinophils in the presence of 1 μg/mL LM (an optimal concentration determined after dose–response preliminary experiments) was significantly reduced by 66.1% (± 20%) when eosinophils were pretreated with a blocking anti-TLR2 antibody but not with a blocking anti-TLR4 antibody or an isotype control. These results suggest that LM, a purified component of BCG, can induce eosinophil degranulation mainly in a TLR2-dependent manner.
BCG-induced eosinophil activation is dependent on MyD88, p38, and NF-κB
Activation of TLR2 signaling pathway involved recruitment of the intracellular adaptor protein MyD88 (myeloid differentiation factor 88), TIRAP (Toll/IL-1R domain-containing adaptor protein), TRAF6 (TNF receptor–associated factor 6), and leads to the phosphorylation of MAPK or NF-κB.31 We first detected, by RT-PCR, MyD88, TRAF6, and TIRAP mRNA in human eosinophils (Figure 4A). Western blot analysis of cell lysates confirmed the presence of the MyD88 protein in human eosinophils, similarly to neutrophils that were used as positive control (Figure 4B). To elucidate the signaling pathway underlying BCG-induced eosinophil activation, we demonstrated that a MyD88 inhibitory peptide, but not a control peptide, reduced ROS production in BCG-stimulated eosinophils, in a dose-dependent manner (Figure 4C).
MyD88, p38 MAP kinase and NF-κB pathway activation after stimulation of eosinophils with M bovis BCG. (A) MyD88, TIRAP, and TRAF6 expression on eosinophils was analyzed with RT-PCR. (B) Total proteins were extracted from eosinophils and neutrophils and equal protein amounts were analyzed with the use of Western blot for MyD88. The gel from 1 of 2 similar experiments is shown. (C) Measurement of ROS release by eosinophils preincubated with serially diluted MyD88 inhibitor 1 μmol/L (×), 10 μmol/L (▵), or 100 μmol/L (●) or with peptide control (100 μmol/L) (○) at 37°C for 30 minutes, further activated with BCG (10:1). ROS release by BCG (1:10 ■)–activated eosinophils without MyD88 inhibitor and by unstimulated eosinophils (−) were determined. Results are expressed as ROS cps values and 1 representative of 3 experiments was shown. (D) Purified eosinophils were pretreated with inhibitors to JNK1/2 (SP 600125, 0.1 μmol/L), ERK1/2 (PD 98 059, 0.1 μmol/L), p38 MAP kinase (SB 203580, 0.1 μmol/L), or NF-κB inhibitors (BAY 11-7082, 1 μmol/L) for 30 minutes at 37°C, before the addition of BCG (10:1). ROS release by eosinophils was analyzed by chemiluminescence. Bar graph represents the percentage ROS release inhibition. Results are expressed as mean plus or minus SEM (n = 3-4). (E) Purified eosinophils were stimulated with different numbers of BCG for the times indicated, and total cell extracts were analyzed by Western blotting using Abs against phosphorylated or nonphosphorylated forms of p38 MAP kinase. The results are representative of 2 independent experiments. *P < .05.
MyD88, p38 MAP kinase and NF-κB pathway activation after stimulation of eosinophils with M bovis BCG. (A) MyD88, TIRAP, and TRAF6 expression on eosinophils was analyzed with RT-PCR. (B) Total proteins were extracted from eosinophils and neutrophils and equal protein amounts were analyzed with the use of Western blot for MyD88. The gel from 1 of 2 similar experiments is shown. (C) Measurement of ROS release by eosinophils preincubated with serially diluted MyD88 inhibitor 1 μmol/L (×), 10 μmol/L (▵), or 100 μmol/L (●) or with peptide control (100 μmol/L) (○) at 37°C for 30 minutes, further activated with BCG (10:1). ROS release by BCG (1:10 ■)–activated eosinophils without MyD88 inhibitor and by unstimulated eosinophils (−) were determined. Results are expressed as ROS cps values and 1 representative of 3 experiments was shown. (D) Purified eosinophils were pretreated with inhibitors to JNK1/2 (SP 600125, 0.1 μmol/L), ERK1/2 (PD 98 059, 0.1 μmol/L), p38 MAP kinase (SB 203580, 0.1 μmol/L), or NF-κB inhibitors (BAY 11-7082, 1 μmol/L) for 30 minutes at 37°C, before the addition of BCG (10:1). ROS release by eosinophils was analyzed by chemiluminescence. Bar graph represents the percentage ROS release inhibition. Results are expressed as mean plus or minus SEM (n = 3-4). (E) Purified eosinophils were stimulated with different numbers of BCG for the times indicated, and total cell extracts were analyzed by Western blotting using Abs against phosphorylated or nonphosphorylated forms of p38 MAP kinase. The results are representative of 2 independent experiments. *P < .05.
We have then further assessed the role of MAPK and NF-κB by using various selective inhibitors of MAPK pathways, including SB 203580 (p38 MAPK inhibitor), PD 98 059 (ERK inhibitor), SP600125 (JNK inhibitor), and BAY 11-7082. Whereas SB 203580 was able to significantly inhibit BCG-induced ROS release by eosinophils, PD 98 059 and SP 600125 had only a marginal effect (Figure 4D). In addition, we obtained 51% (± 4.3%) inhibition of ROS release by BCG-activated eosinophils with BAY 11-7082. Overall, these results suggest that p38 MAP kinase and NF-κB signaling pathways play a prominent role in BCG-induced ROS release by eosinophils. To confirm that intracellular signaling pathway of eosinophils was activated by BCG, we next investigated the p38 MAPK phosphorylation profile. As shown in Figure 4E, stimulation of eosinophils with BCG resulted in p38 phosphorylation after a 5-minute stimulation. This p38 MAPK phosphorylation decreased after 30 minutes of BCG stimulation. In addition, LM-induced eosinophil activation involved a MyD88 and p38 MAPK pathways, because LM-induced EPO release was inhibited by a MyD88 inhibitor (maximal inhibition 72.8% ± 6.2%) and SB 203580 (maximal inhibition 49.6% ± 16.1%; Figure S4). Of note LY294002, a phosphoinositide kinase-3 (PI3K) inhibitor, had no effect on ROS release by BCG-activated eosinophils (data not shown). Taken together, these findings indicate that BCG can activate eosinophils through MyD88-, p38 MAPK-, and NF-κB–dependent pathways.
Eosinophils control BCG growth
Because of the release of cytotoxic mediators by eosinophils, we next addressed whether eosinophils may displayed phagocytic and antimycobacterial activity. Survival of BCG in the presence of human eosinophils was thus tested. A decrease in mycobacterial survival was observed for all BCG/eosinophil ratios (Figure 5A). Eosinophils were able to restrict BCG growth by 31.8% for 20:1 ratio and 56.9% for 5:1 ratio within 6 hours after the addition of BCG. Because BCG is an intracellular attenuated pathogen, we tested the ability of eosinophils to phagocytose PKH26-BCG by fluorescence microscopy (Figure 5B). Dose-dependent internalization was observed when eosinophils were incubated with increasing BCG/eosinophil ratios. Extracellular mycobacteria were removed by washing, and only remaining eosinophils were lysed and plated at increasing intervals for assessment of viable bacilli. As shown in Figure 5C, for 5:1 ratio, the number of CFUs by intracellular BCG significantly decreased with incubation time, suggesting that eosinophil cytotoxicity could be due in part to release of cytotoxic mediators.
BCG growth inhibition by eosinophils. (A) BCG growth in the presence of eosinophils for the indicated times. Data are shown as the mean of 3 independent experiments plus or minus SEM, expressed in percentage of CFU control ([CFU with eosinophils/CFU with medium] ×100). (B) Quantitive detection of internalized PKH26-BCG by fluorescence microscopy. Eosinophils were incubated with or without BCG for 40 minutes at 37°C. (C) Intracellular BCG growth inhibition with different BCG/eosinophil ratios (5:1, ■; 10:1, ▵; 20:1, ●). Results are expressed as mean plus or minus SEM (n = 3). Significant differences between conditions studied and controls are indicated as followed: *P < .05, **P < .01.
BCG growth inhibition by eosinophils. (A) BCG growth in the presence of eosinophils for the indicated times. Data are shown as the mean of 3 independent experiments plus or minus SEM, expressed in percentage of CFU control ([CFU with eosinophils/CFU with medium] ×100). (B) Quantitive detection of internalized PKH26-BCG by fluorescence microscopy. Eosinophils were incubated with or without BCG for 40 minutes at 37°C. (C) Intracellular BCG growth inhibition with different BCG/eosinophil ratios (5:1, ■; 10:1, ▵; 20:1, ●). Results are expressed as mean plus or minus SEM (n = 3). Significant differences between conditions studied and controls are indicated as followed: *P < .05, **P < .01.
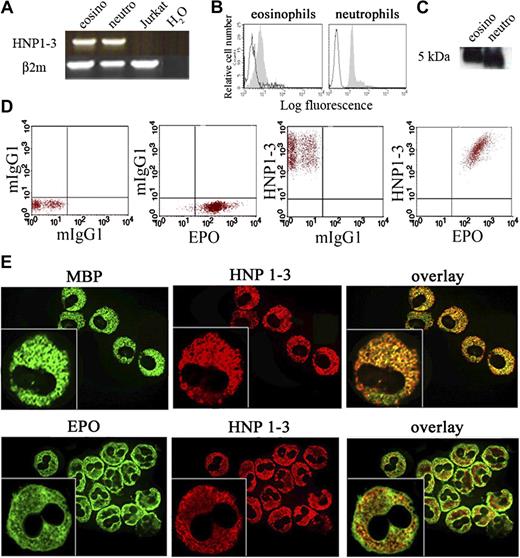
Human eosinophils express α-defensins
To investigate which mediators could contribute to eosinophil cytotoxicity toward BCG, we investigated the expression of defensins, major effector molecules in innate immunity against microbes.32 We did not detect any expression of mRNA β-defensins in unstimulated and BCG-stimulated eosinophils in contrast to neutrophils (data not shown). However, both neutrophils and eosinophils, but not Jurkat T cells, expressed α-defensin (HNP1-3) mRNA (Figure 6A). As shown in Figure 6B and C, α-defensins also were detected in eosinophils by flow cytometry and in cell lysates. The association of α-defensins immunoreactivity with crystalloid granules was shown by flow cytometric analysis on purified EPO+ eosinophil granules (Figure 6D). To determine the intracellular localization site of α-defensins, we conducted a double immunofluorescence staining with antibodies specific for MBP (localized in the granule crystalloid core) and EPO (localized in the granule matrix region; Figure 6E).33 Immunoreactivity against MBP and α-defensins were mostly colocalized, whereas immunoreactivity against EPO and α-defensins only displayed minor colocalization. Taken together, our results showed a constitutive expression of α-defensins in eosinophils. These observations led us to hypothesize that eosinophils may respond to BCG by rapid release of α-defensins.
Expression of α-defensins by human eosinophils. Intracellular α-defensin (HNP1-3) expression on eosinophils (eosino) and neutrophils (neutro) was analyzed with RT-PCR (A), flow cytometry (B), and Western blot (C). (D) α-defensin expression on EPO+ crystalloid granules purified from human eosinophils. Staining with control isotype antibodies is represented. Results correspond to one representative eosinophil donor. (E) Immunofluorescence and confocal (insets) analysis of human eosinophils with the use of Alexa Fluor 555 goat anti–mouse secondary antibody (red) to detect the HNP1-3 immunoreactivity or Alexa Fluor 488 streptavidin (green) to detect immunoreactivity against MBP or EPO.
Expression of α-defensins by human eosinophils. Intracellular α-defensin (HNP1-3) expression on eosinophils (eosino) and neutrophils (neutro) was analyzed with RT-PCR (A), flow cytometry (B), and Western blot (C). (D) α-defensin expression on EPO+ crystalloid granules purified from human eosinophils. Staining with control isotype antibodies is represented. Results correspond to one representative eosinophil donor. (E) Immunofluorescence and confocal (insets) analysis of human eosinophils with the use of Alexa Fluor 555 goat anti–mouse secondary antibody (red) to detect the HNP1-3 immunoreactivity or Alexa Fluor 488 streptavidin (green) to detect immunoreactivity against MBP or EPO.
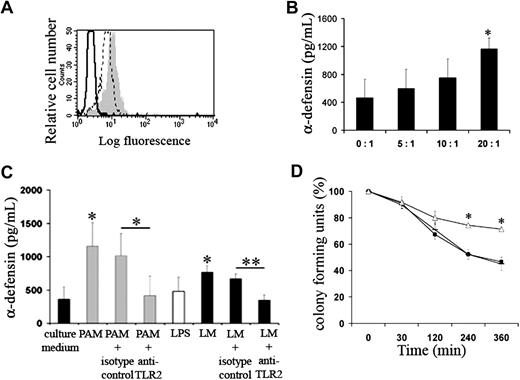
BCG-induced α-defensin and ECP release contributes to eosinophil cytotoxicity
α-defensins immunoreactivity was further increased upon activation by BCG and eosinophil pretreatment with brefeldin A (1 μg/mL; Figure 7A). In addition, our results suggest that BCG-activated eosinophils also released α-defensins in a dose-dependent manner (Figure 7B). After stimulation with PAM or LM, but not LPS, α-defensins were detected in culture supernatants. Production of α-defensins in response to PAM or LM was significantly abolished when eosinophils were preincubated with a blocking anti-TLR2 antibody, whereas no inhibition of α-defensin release was observed with an isotype control, indicating a TLR2-dependent α-defensin release (Figure 7C). Furthermore, preincubation with a blocking anti–α-defensin antibodies partially but significantly increased the BCG growth at the 5:1 ratio, suggesting that α-defensins indeed contribute to eosinophil cytotoxicity toward mycobacteria (Figure 7D). In addition, α-defensin killing activity against BCG was maximal in the presence of purified ECP (Figure S5A). Accordingly, we evaluated effect of a blocking anti-ECP antibody on BCG growth and showed increased survival upon inhibition of ECP release (Figure S5B). However, the presence of resorcinol and diphenyleneiodonium, the corresponding EPO and ROS inhibitors, did not significantly influence BCG growth (data not shown). These results thus suggest that LM is a BCG component accounting for the α-defensin release and that a killing mechanism used by eosinophils to inhibit intracellular BCG growth is α-defensin and ECP-dependent.
α-defensins synthesis and release by human eosinophils in the presence of BCG. (A) α-defensin expression after 2 hours of eosinophil stimulation (gray histogram) or unstimulation (dotted line) with BCG (10:1) in the presence of brefeldin A. Black line represents staining with isotype control. (B) α-defensin levels released by eosinophils activated by BCG were quantified by ELISA in cell culture supernatants. Results are expressed as mean plus or minus SEM (n = 3). (C) After incubation of eosinophils, pretreated by blocking anti-TLR2 antibody or isotype control, with PAM (0.5 μg/mL), LPS (0.1 μg/mL), or LM (1 μg/mL), α-defensin levels were quantified in the culture supernatants by ELISA. Results are represented as the mean of 3 independent experiments plus or minus SEM (D) Intracellular BCG growth inhibition. Eosinophils were treated or not treated with a blocking anti–α-defensin antibody (▵) or an isotype control (−) and were infected with BCG (5:1, ■). Values are mean plus or minus SEM of 3 independent experiments. Significant differences between conditions studied and controls are indicated; *P < .05; **P < .01.
α-defensins synthesis and release by human eosinophils in the presence of BCG. (A) α-defensin expression after 2 hours of eosinophil stimulation (gray histogram) or unstimulation (dotted line) with BCG (10:1) in the presence of brefeldin A. Black line represents staining with isotype control. (B) α-defensin levels released by eosinophils activated by BCG were quantified by ELISA in cell culture supernatants. Results are expressed as mean plus or minus SEM (n = 3). (C) After incubation of eosinophils, pretreated by blocking anti-TLR2 antibody or isotype control, with PAM (0.5 μg/mL), LPS (0.1 μg/mL), or LM (1 μg/mL), α-defensin levels were quantified in the culture supernatants by ELISA. Results are represented as the mean of 3 independent experiments plus or minus SEM (D) Intracellular BCG growth inhibition. Eosinophils were treated or not treated with a blocking anti–α-defensin antibody (▵) or an isotype control (−) and were infected with BCG (5:1, ■). Values are mean plus or minus SEM of 3 independent experiments. Significant differences between conditions studied and controls are indicated; *P < .05; **P < .01.
Discussion
Besides helminth infections, peripheral blood and tissue eosinophilia have been associated with mycobacterial infections.8 Here, we investigated the mechanism of eosinophil–mycobacteria interactions to provide a molecular basis to this observation. The present results indicate that BCG has the propensity to activate eosinophils and that TLR2 plays a major role in the activation process. Contradictory results have been reported regarding TLR expression by human eosinophils. The absence of TLR2 and TLR4 expression was reported in one study,34 whereas other reports evidenced TLR2 and TLR4 mRNA expression35 as well as protein expression of TLR1, 2, 4, 5, 6, and 9 on human eosinophils.27 We have shown an heterogenous donor/patient-dependent TLR2 and TLR4 expression by human eosinophils. Eosinophils from eosinophilic donors but not from healthy donors spontaneously expressed TLR2 and TLR4 at their surface. These observations might explain why eosinophils from eosinophilic donors display a quicker response to BCG than eosinophils from normal donors.
Other receptors, such as CD14, complement receptors and Fcγ receptor expressed by eosinophils,6 could participate to BCG recognition36 and induce TLR expression on eosinophils purified from normal donors after incubation with BCG. Alternatively, it is also possible that TLR expression levels in normal donors are below the detection threshold of flow cytometry and that this low expression is up-regulated upon ligand binding, as it is the case in allergic patients. Spontaneous TLR expression on eosinophils from eosinophilic donors could be explained by in vivo eosinophil priming. Such heterogeneity between eosinophil donors, already evidenced for other membrane receptors including IgE receptors,37 may account for discrepancies in earlier results, which did not discriminate between different clinical status of patients.27,34,35,38,39
Live, but not heat-killed, mycobacteria were able to attract eosinophils in vivo,12 indicating that metabolically active mycobacteria are required. We have shown that live BCG, but not heat-killed BCG, attracted human eosinophils. Our study also identified LM and LAM, 2 heat-stable cell wall–associated lipoglycans, as potent eosinophil migration-inducing factors. However, LAM secretion does require live bacteria to create a gradient allowing for eosinophil-chemotaxis. Furthermore, we cannot exclude that other heat-sensitive secreted compounds are required for optimal chemotaxis. Nevertheless, whether eosinophils recognize and are subsequently activated by mycobacteria remains unclear. Our experiments reveal an important immunostimulatory activity of LM on eosinophils, unlike LAM. These 2 lipoglycans have been reported to exhibit antagonistic activities, and recent studies have suggested that that LM displays stronger proinflammatory responses compared with LAM.4 In addition, we demonstrated a TLR2-dependent eosinophil activation effect by LM. In a murine model of BCG-induced pleurisy, eosinophil recruitment was enhanced by TLR2.18
Both TLR2 and TLR4 are essential to innate immunity against mycobacteria species and were the likeliest PRRs that would have endowed eosinophils with the capacity to be activated by mycobacteria. In the current work, only TLR2 appeared to play a functional role in eosinophil–mycobacteria interactions, because a blocking anti-TLR2 antibody partially suppressed BCG- or LM-induced eosinophils activation. This also suggests that other PRRs could be involved in mycobacteria-induced eosinophil activation such as TLR940 or β-glucan receptor dectin-1.41 However, we cannot rule out the possibility that other mycobacterial cell wall bioactive components, such as trehalose dimycolate (TDM), participate in this process.
To date, a single study has examined the TLR signal transduction.27 Various TLR ligands differentially induced the release of cytokines, chemokines, superoxides, or granular protein. Indeed, TLR7 ligand R837 and TLR2 ligand peptidoglycan activations were dependent on the p38 or ERK MAPK pathway, respectively, and induced IL-1β, IL-6, IL-8, and growth-related oncogene (GRO)-α release by eosinophils. Surprisingly, expression and recruitment of MyD88, the central adapter shared by several TLRs, was never investigated in these studies. We have extended these observations by reporting that TLR-dependent activation of eosinophils through BCG activation required both MyD88, p38 MAPK, and NF-κB molecules.
Although eosinophilia has been evidenced in different mycobacteria-infection models, their contribution in controlling BCG growth is unknown. Our results show that human eosinophils expressed α-defensins, localized within the eosinophil crystalloid granules. Eosinophils are among the few inflammatory cells capable of storing proteins, cytokines, and chemokines in their secretory granules. These stored products may be rapidly mobilized from intracellular sites of storage and released locally during inflammation. In addition, eosinophils could release α-defensins in response to BCG or LM through TLR2 ligation. Interestingly, α-defensins can directly kill BCG in vitro, and α-defensin-producing eosinophils play a key role in BCG growth inhibition. These results are quite surprising because human β-defensin-1 and 2 genes usually are considered to display strong antimycobacterial properties.42,43 Activity of α-defensins toward mycobacterial species seems strain-dependent.44 The potent bactericidal activity of α-defensins against virulent mycobacteria45 is consistent with our data when BCG is used as a model. Because α-defensin release is rapid, it is conceivable that when recruited to infection sites, eosinophils may directly contribute to bacterial killing. Other cytotoxic mediators might also be released by eosinophils because the blocking of α-defensin activity only partially prevented BCG growth. Indeed, it is worth pointing out that when eosinophils were activated with BCG release of both EPO, which has a lytic activity against M tuberculosis,46 and ECP, a ribonuclease that possesses antimicrobial activity against both Gram-negative and Gram-positive strains,47 was observed. Our results indicate that α-defensins and ECP have to be considered as important components of the mechanisms by which eosinophils kill BCG. These results provide evidence that eosinophils harbor a diverse arsenal of cytotoxic components against mycobacteria.
The ability of eosinophils to interact and kill BCG challenges the concept that vaccination with BCG and resistance against acute tuberculosis is dependent on host ability to generate Th1 immunity. Although eosinophils often are intimately linked with Th2-driven immunity, they have been shown to express Th1 cytokines, such as IFN-γ, upon stimulation by CD28.22 However, we failed to detect IFN-γ release by eosinophils in the presence of BCG (data not shown), whereas BCG induced TNF-α, IL-8, MIF, MIP-1α, MIP-1β, IL-13, and IL-16 release. Inflammatory granuloma responses usually are associated with angiogenesis, involving IL-8, and with chemokines, such as MIP, which facilitate the recruitment of inflammatory cells to the site of infection.48 It is noteworthy that LM, but not LAM, has been reported to be strong IL-8 and TNF-α-inducing factor.30
TNF-α is a key macrophage-activating cytokine for intracellular killing of M tuberculosis.49 Both beneficial and deleterious effects of TNF-α have been observed in tuberculosis patients.50 These dual effects have also been attributed to tumor-associated eosinophils.51 However, an increased Th2 immunity has been associated with active tuberculosis.5 In many developing countries, patients infected with M tuberculosis face helminth infection, often associated with eosinophilia and Th2 response.10 Therefore, the Th2-driven immunity could increase susceptibility to tuberculosis and could play a role in a persistent form of the disease. Extensive analysis of tuberculosis-associated eosinophilia and correlation with disease outcome would represent a further goal to better understand the role of eosinophils during tuberculosis infection and progression of the disease.
In conclusion, our results represent the first evidence of the involvement of α-defensins, released by human eosinophils upon TLR2 stimulation in immunity against an intracellular pathogen. This study highlights a mechanism of direct pathogen recognition by human eosinophils, thereby broadening their functional importance as early direct sensors and effectors against bacteria.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr R. Paumelle, C. Cudejko, and N. Dupont for their assistance. We thank Dr C. Locht and C. Rouanet (Inserm U629, Institut de Biologie de Lille, Lille, France) for providing M bovis BCG.
This study was supported by a grant from the Biologie-santé program (Fonctions des éosinophiles et pathologies à éosinophiles). L.K. was supported by a grant from the CNRS, Paris, France (Action Thématique Incitative sur Program Microbiologie Fondamentale). Y.G. was supported by ANR005N/FEDER028F.
Authorship
Contribution: V.D. performed research and wrote the paper; F.L. performed research and statistical analysis; E.H. analyzed data and reviewed the drafts of the paper; S.L. was essential for helping with patient sample purifications; Y.G. and L.K. provided purified mycobacterial components; E.A. and G.W. critically reviewed the manuscript; D.D. provided intellectual input and reviewed drafts of the paper; and M.C. designed and interpreted the experiments.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Monique Capron, Inserm U547, Institut Pasteur de Lille, 1 rue Prof Calmette BP245, 59019 Lille Cedex, France; e-mail: Monique.capron@pasteur-lille.fr.
References
Author notes
*V.D. and F.L. contributed equally to this work.




![Figure 5. BCG growth inhibition by eosinophils. (A) BCG growth in the presence of eosinophils for the indicated times. Data are shown as the mean of 3 independent experiments plus or minus SEM, expressed in percentage of CFU control ([CFU with eosinophils/CFU with medium] ×100). (B) Quantitive detection of internalized PKH26-BCG by fluorescence microscopy. Eosinophils were incubated with or without BCG for 40 minutes at 37°C. (C) Intracellular BCG growth inhibition with different BCG/eosinophil ratios (5:1, ■; 10:1, ▵; 20:1, ●). Results are expressed as mean plus or minus SEM (n = 3). Significant differences between conditions studied and controls are indicated as followed: *P < .05, **P < .01.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/113/14/10.1182_blood-2008-07-166595/4/m_zh80040929990005.jpeg?Expires=1769261152&Signature=epl~ktH5VGu3XT11zQTcGtk0RMMgymhsngL4CLSW5S1mRzF46pbkxXxjW8NHghpNNN76dauZWTRpxyWeqlktYmJUm7zMyyuxI2z8XP~Ilbryi-Fig1XSi~L4OrGyD8gbiGB28E4C2D3zEKduY6Gph8eqSL8zRzZFKRE52g0DYz1Gg1hJLOnG6oAxgU1GjpikJf5sysQfom1DpzrnZBcri5H3NhP17k~h89BB6D6QZqDShQMnyIvvXs~wOFZuC316T8Z8evSL6uawujmkGc7IzoHA50M4YQk0v9QHpLWV5BkztnagDfa~tVy5G8FhSQ-CWaR1EhRSnuPMo4YFKGOzsA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal