Abstract
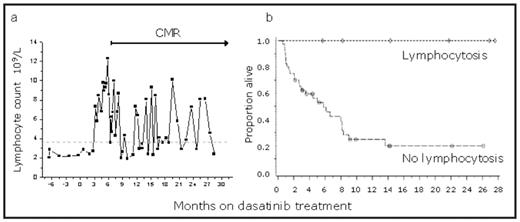
Tyrosine kinase inhibitors (TKIs) targeting the BCR-ABL fusion protein are an effective therapy for Philadelphia chromosome positive (Ph+) leukemia. Dasatinib, a 2nd generation pan-TKI, also inhibits wild-type kinases, which may result in unexpected clinical responses. Recent data suggest that dasatinib has a potent immunosuppressive effect on T- and NK-cells in vitro. In contrast, we have noticed a marked expansion of lymphocytes in blood in a subset of dasatinib patients, but its clinical significance and molecular mechanisms are unclear. In this multicenter study, 19 Ph+ leukemia patients with marked lymphoproliferation in blood while on dasatinib (9 CML CP, 2 CML AP, 2 CML BC, 6 Ph+ALL) were identified. Clonality, immunophenotype, and intracellular signaling was analyzed and related clinical information was collected. In addition, prevalence and prognostic significance of the phenomenon was retrospectively assessed in a Phase II clinical study on 46 Ph+ ALL patients. An abrupt lymphocytosis (peak count range 4–20×109/L) with large granular lymphocyte (LGL) morphology was observed after a median of 3 months from the start of therapy (range 1–8 months). In most patients, LGL lymphocytosis was long-lasting and continued throughout dasatinib therapy, albeit with marked fluctuations in absolute lymphocyte count (Fig. 1a). In all evaluable patients (n=4), lymphocyte counts normalized after drug discontinuation. All patients were previously exposed to imatinib without similar changes in lymphocyte count or morphology. By immunophenotyping, 14 patients had a cytotoxic T-cell and 5 patients a NK-cell phenotype. After initiation of dasatinib therapy, the CD4/CD8 ratio shifted, expression of activation antigens HLA-DR and CD57 increased, expression of homing antigen CD62L decreased and relative numbers of regulatory T-cells were significantly decreased (p<0.001). All patients with T-LGL phenotype had mono/oligoclonal rearrangements in TCR g/d genes. Quantitative allele-specific oligonucleotide PCR analysis from samples before and during dasatinib therapy indicated that LGL lymphocytosis results from expansion of a pre-existing terminal memory cell clone (CD8+CD62Llow). By using single-cell profiling of nodal phosphoproteins (ERK1/2, STAT1, STAT3, STAT5, STAT6) by multi-color FACS, we showed that during dasatinib therapy LGL patients were more responsive to cytokine or growth factor stimuli (IL-2, IL-4, IL-6, IFNs, GM-CSF), when compared to dasatinib patients without lymphocytosis or to healthy controls. This indicates alternative signaling pathway usage not inhibited by dasatinib and/or cytokine hypersensitivity. Dasatinib-related severe adverse effects were common in patients with LGL lymphocytosis. Pleural effusions and/or pulmonary infiltrates were seen in 13/19 patients, modest CMV reactivation in 9/19 patients, colitis in 11/19 patients and long lasting mild fever in 14/19 patients. Accumulation of pheno- and genotypically identical cytotoxic T-cells was also detected in pleural effusion and colitis biopsy samples. Adverse effects were temporally related to dasatinib therapy and emerged after the appearance of LGL lymphocytosis. All patients with relapsed poor prognosis leukemia (Ph+ ALL n=5, blastic phase CML n=2) achieved durable complete molecular responses (CMR) during dasatinib therapy, CMR still ongoing in 3 patients (follow-up 18+ months). In the confirmatory Phase II dasatinib study in Ph+ ALL (START-L), patients with lymphocytosis had superior survival compared to patients without lymphocytosis (Fig. 1b). In conclusion, we propose that by inhibiting immunoregulatory kinases, dasatinib may induce a reversible state of aberrant immune reactivity in a distinct subset of patients and result in anti-leukemia and anti-host responses driven by cytotoxic T/NK LGL cells. Further studies pinpointing the mechanisms, such as the target antigens on the malignant cells and activation pathways are ongoing.
Disclosures: Ekblom:BMS: Consultancy. Garzon:BMS: Employment. Shah:BMS, Novartis: Consultancy. Simonsson:BMS, Novartis: Consultancy, Research Funding. Steegmann:BMS, Novartis, Wyeth: Consultancy, Honoraria, Research Funding. Porkka:BMS, Novartis: Consultancy, Honoraria, Research Funding.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal