Abstract
Background: Angiogenesis plays an important role in the pathogenesis of acute myeloid leukemia (AML) and vascular endothelial growth factor (VEGF) is an essential positive regulator of this process. Placental growth factor (PlGF) is a member of VEGF family that exerts its angiogenic action by synergizing with VEGF. There is also evidence that PlGF may be survival factor for angiogenic endothelial cells. The role of PlGF in patients with acute leukemia have not been investigated at all.
Material and methods: We measured the plasma concentrations of VEGF and PlGF in 61 patients with newly diagnosed AML and 22 healthy controls using the ELISA assay. Additionally, in AML patients we correlated the plasma levels of angiogenic cytokines with the number of viable (CEC) and apoptotic (CECAnnV+) circulating endothelial cells, known prognostic factors, response to induction therapy as well as overall survival (OS). The AML group consisted of 34 women and 27 men with a median age of 49 years (range 25–76 years). All patient received standard induction chemotherapy (according to 3+7 protocol). Statistical analysis included the following variables: VEGF and PlGF levels, age, sex, performance status, cytogenetic risk group according SWOG, presence of multilineage dysplasia, WBC and PLT count, hemoglobin level, LDH activity, % of bone marrow blasts and CEC as well as CECAnnV+ number.
Results: The PlGF and VEGF median levels (23,6 pg/ml and 45,1 pg/ml respectively) were significantly higher in the AML at diagnosis than in the healthy subjects (9,5 pg/ml; p<0,0001 and 25,2 pg/ml; p<0,03 respectively). Moreover, the VEGF level at diagnosis in patients who did not respond to induction chemotherapy was significantly higher than in patients who achieved complete remission (CR) (84,7 vs 31,2 pg/ml; p<0,01). The significant negative correlation between the VEGF and percentage of apopototic CECAnnV+ was also observed.
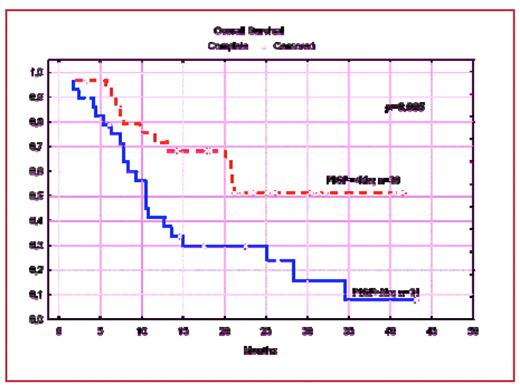
Median follow-up was 12,1 months (range: 1– 43 months). 50 patients (82%) achieved CR. The CR rate in low and high VEGF expressors was respectively 86% and 70% (p=0.07). The CR rate in high- and low PlGF expressors did not differ significantly (74% and 80% respectively). In univariate analysis poor cytogenetics was the only factor associated with increased risk of treatment failure. The median time of OS in analysed group was 15 months. In the univariate analysis high (over median) PlGF levels was associated with shorter OS (p=0.005) (Figure1).
Shorter OS was also associated with age>40 years (p=0.009), failure to achieve CR (p=0.009) and higher (>50%) bone marrow infiltration with leukemic blasts (p=0.005). In the multivariate Cox proportional hazard model the elevated PlGF plasma level was strongly associated with shorter OS (p<0.007). The other factors found to influence shorter OS were: high bone marrow infiltration with leukemic blasts (p=0.02), age>40 years (p=0.04), failure to achieve CR (p=0.04).
Conclusions: In conclusion we can state that the high plasma concentration of PlGF is associated with poor prognosis in AML patients. Observed in our study significantly higher PlGF level in AML patients compared to healthy controls may indicate that this angiogenic cytokine plays an important, independent of VEGF role in pathogenesis of AML
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal