Abstract
The positive regulatory domain I (PRDM1) is a master regulator of terminal B-cell differentiation. However, PRDM1 is not B-cell specific. To determine its role in T-cell lymphoma, PRDM1 expression was investigated in 60 patients. PRDM1α and PRDM1β transcripts were detected in laser-microdissected T-lymphoma cells in 27 and 14 patients, respectively, mostly in cases with IRF4 expression. PRDM1β was associated with increased c-MYC expression. PRDM1β-positive patients displayed advanced Ann Arbor stage and high-risk International Prognostic Index and were linked to short survival times. In vitro, PRDM1β was related to resistance to chemotherapeutic agents and could be down-regulated by the proteasome inhibitor bortezomib. Kinetic studies showed that bortezomib down-regulation of PRDM1β preceded decreased IRF4 and c-MYC expression. An earlier retaining of cytoplasmic IκBα in bortezomib-treated cells was revealed, concomitant with blockade of NF-κB nuclear translocation. These results demonstrate the involvement of PRDM1β in T-cell lymphoma, with possible therapeutic interference by the proteasome inhibitor.
Introduction
The positive regulatory domain I (PRDM1) belongs to the PRDM gene family of transcriptional repressors and is required for terminal B-cell differentiation into plasma cells.1 However, the involvement of PRDM1 in hematopoietic development is not restricted to the B-cell lineage. Recent studies have implicated PRDM1 in the regulation of T-cell activation and homeostasis.2,3 PRDM1 was also detected in a subset of T-cell lymphomas,4 while the significance of PRDM1 expression in this disease remains to be investigated.
PRDM1 has 2 isoforms: PRDM1α and PRDM1β. Generated from the same gene by alternative transcription initiation, PRDM1β differs from PRDM1α by the lack of 101 NH2-terminal amino acids, resulting in a disrupted PR domain and loss of repressive function on multiple target genes.5 Recently, we have shown that PRDM1β is associated with chemoresistance in B-cell lymphoma, which could be overcome by nonchemotherapeutic agent rituximab through NF-κB inactivation.6 Here we identify the role of PRDM1β in T-cell lymphoma and its modulation in vitro by the proteasome inhibitor bortezomib.
Methods
Patients
Sixty de novo T-cell lymphoma patients (32 male and 28 female, ages 18 to 70 [median, 43] years) were included. Their main characteristics are summarized in Table 1. This study was approved by the Shanghai Institute of Hematology-Rui Jin Hospital Institutional Review Board. Informed consent was obtained from all patients in accordance with the Declaration of Helsinki.
PRDM1 expression in T-cell lymphoma
| . | No. . | PRDM1 (%) . | IRF4 (%) . | Laser-microdissected cells . | ||
|---|---|---|---|---|---|---|
| PRDM1α (%) . | PRDM1β (%) . | IRF4 (%) . | ||||
| Histologic typing (World Health Organization classification) | ||||||
| Peripheral T-cell lymphoma | 23 | 10 (43.5) | 15 (65.2) | 14 (60.9) | 7 (30.4) | 15 (65.2) |
| Anaplastic large-cell lymphoma | 9 | 5 (55.6) | 8 (88.9) | 7 (77.8) | 4 (44.4) | 8 (88.9) |
| T/NK nasal-type lymphoma | 12 | 3 (25.0) | 8 (66.7) | 4 (33.3) | 2 (16.7) | 8 (66.7) |
| T-angioimmunoblastic lymphoma | 5 | 1 (20.0) | 2 (40.0) | 2 (40.0) | 1 (20.0) | 2 (40.0) |
| T-lymphoblastic lymphoma | 11 | 0 | 0 | 0 | 0 | 0 |
| Ann Arbor stage | ||||||
| I to II | 12 | 2 (16.7) | 6 (50.0) | 4 (33.3) | 0 | 6 (50.0) |
| III to IV | 48 | 17 (35.4) | 27 (56.3) | 23 (47.9) | 14 (29.2) | 27 (56.3) |
| No. of sites of extranodal involvement | ||||||
| 0 to 1 | 29 | 10 (34.5) | 18 (62.2) | 13 (44.8) | 6 (20.7) | 18 (62.2) |
| 2 to 3 | 31 | 9 (29.0) | 15 (48.4) | 14 (45.2) | 8 (25.8) | 15 (48.4) |
| Serum LDH level | ||||||
| Normal or lower | 23 | 9 (39.1) | 14 (60.9) | 10 (43.5) | 6 (26.1) | 14 (60.9) |
| Higher than normal | 37 | 10 (27.0) | 19 (51.4) | 17 (45.9) | 8 (21.6) | 19 (51.4) |
| IPI score | ||||||
| Low risk to intermediate low risk | 23 | 5 (21.7) | 13 (56.5) | 9 (39.1) | 2 (8.7) | 13 (56.5) |
| Intermediate high risk to high risk | 37 | 14 (37.8) | 20 (54.1) | 18 (48.6) | 12 (32.4) | 20 (54.1) |
| . | No. . | PRDM1 (%) . | IRF4 (%) . | Laser-microdissected cells . | ||
|---|---|---|---|---|---|---|
| PRDM1α (%) . | PRDM1β (%) . | IRF4 (%) . | ||||
| Histologic typing (World Health Organization classification) | ||||||
| Peripheral T-cell lymphoma | 23 | 10 (43.5) | 15 (65.2) | 14 (60.9) | 7 (30.4) | 15 (65.2) |
| Anaplastic large-cell lymphoma | 9 | 5 (55.6) | 8 (88.9) | 7 (77.8) | 4 (44.4) | 8 (88.9) |
| T/NK nasal-type lymphoma | 12 | 3 (25.0) | 8 (66.7) | 4 (33.3) | 2 (16.7) | 8 (66.7) |
| T-angioimmunoblastic lymphoma | 5 | 1 (20.0) | 2 (40.0) | 2 (40.0) | 1 (20.0) | 2 (40.0) |
| T-lymphoblastic lymphoma | 11 | 0 | 0 | 0 | 0 | 0 |
| Ann Arbor stage | ||||||
| I to II | 12 | 2 (16.7) | 6 (50.0) | 4 (33.3) | 0 | 6 (50.0) |
| III to IV | 48 | 17 (35.4) | 27 (56.3) | 23 (47.9) | 14 (29.2) | 27 (56.3) |
| No. of sites of extranodal involvement | ||||||
| 0 to 1 | 29 | 10 (34.5) | 18 (62.2) | 13 (44.8) | 6 (20.7) | 18 (62.2) |
| 2 to 3 | 31 | 9 (29.0) | 15 (48.4) | 14 (45.2) | 8 (25.8) | 15 (48.4) |
| Serum LDH level | ||||||
| Normal or lower | 23 | 9 (39.1) | 14 (60.9) | 10 (43.5) | 6 (26.1) | 14 (60.9) |
| Higher than normal | 37 | 10 (27.0) | 19 (51.4) | 17 (45.9) | 8 (21.6) | 19 (51.4) |
| IPI score | ||||||
| Low risk to intermediate low risk | 23 | 5 (21.7) | 13 (56.5) | 9 (39.1) | 2 (8.7) | 13 (56.5) |
| Intermediate high risk to high risk | 37 | 14 (37.8) | 20 (54.1) | 18 (48.6) | 12 (32.4) | 20 (54.1) |
Tissue samples
Lymphoma tissue samples were immediately cut into 2 parts: 1 part fixed in formaldehyde and processed for paraffin embedding, and the other snap frozen and stored at − 80°C. Systematic microscopic control of the lymphoma lesion was performed for each block.
Cell culture
T-lymphoma cell lines HUT78, HUT102, and MOLT4 (American Type Culture Collection, Manassas, VA) were treated with chemotherapeutic agents, bortezomib (25 nM; Millennium Pharmaceuticals, Cambridge, MA) or pyrrolidine dithiocarbamate (PDTC, 20 μM; Sigma-Aldrich, St Louis, MO), which specifically inhibits NF-κB activation.7 Methotrexate-resistant subclone was selected from the original MOLT4 by exposure to increasing concentrations of methotrexate, as described by Fotoohi et al.8
Immunohistochemistry and immunofluorescence assay
Immunohistochemical analysis was performed on 5-μm paraffin sections with an indirect immunoperoxidase method, using antibodies against PRDM1,6 IRF4 (1:40; Dako, Glostrup, Denmark), and c-MYC (1:100; Santa Cruz Biotechnology, Santa Cruz, CA). Immunofluorescence assay was performed as previously reported.9
Laser microdissection
Frozen sections (7 μm each) were incubated in RNAse-free conditions with anti-CD3 antibody (1:50; Dako) and fluorescein-conjugated goat anti–mouse IgG antibody (1:50; Jackson ImmunoResearch Laboratories, West Grove, PA) each for 5 minutes. Laser microdissection of fluorescent cells was immediately performed (Leica Microsystems, Wetzlar, Germany) for RNA extraction.
Semiquantitative reverse-transcription polymerase chain reaction (PCR), sequence analysis, and Western blot
As previously reported,6 the NF-κB (P65) and IκBα antibodies were obtained from Santa Cruz Biotechnology. The phosphorylated form of IκBα (p-IκBα) antibody was purchased from Cell Signaling (Beverly, MA).
Statistical analysis
Patient characteristics were compared using χ2 and Fisher exact test. Kaplan-Meier and log-rank test were performed to estimate the survival functions. Overall survival was measured from the time of diagnosis to the date of death or last contact. Event-free survival was calculated from the time of diagnosis to the date of progression, death, or last contact. P values less than .05 were considered significant. All statistical analyses were performed on SAS 8.2 software (SAS Institute, Cary, NC).
Results and discussion
T-lymphoma cells expressed PRDM1
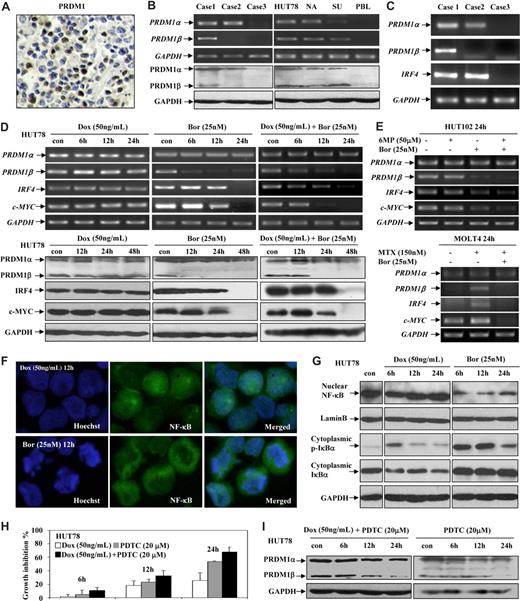
By immunohistochemistry, nuclear PRDM1 expression (Figure 1A) was observed in 19 (31.7%) of 60 patients. According to histologic type, PRDM1 was found in peripheral T-cell lymphoma (10/23, 43.5%), anaplastic large-cell lymphoma (5/9, 55.6%), T/natural killer (NK) nasal-type lymphoma (3/12, 25.0%), and T-angioimmunoblastic lymphoma (1/5, 20.0%) (Table 1). T-lymphoblastic lymphoma did not express PRDM1, as shown by Garcia et al.4
PRDM1 was expressed in T-cell lymphoma and could be down-regulated by bortezomib through NF-κB inactivation. (A) Nuclear PRDM1 protein expression was revealed by immunohistochemistry on lymphoma tissue. Leica AS LMD (Leica Microsystems), 40×/0.6 CORR XT, air/0.6, hematoxylin-eosin stain, Video camera 3CCD Hitachi HV-Dz0P, Leica AS LMD software, version 4.4. (B) PRDM1 mRNA and protein expression were detected by semiquantitative PCR on lymphoma cells and Western blot on lymphoma tissue, respectively. PRDM1 isoforms were expressed in laser-microdissected lymphoma cells and T- and B-lymphoma cell lines (NA indicates namalwa; SU, SU-DHL-4), but not in peripheral blood lymphocytes (PBLs). (C) Laser-microdissected lymphoma cells showed coexpression of PRDM1 and IRF4. (D) In HUT78 cells resistant to doxorubicin (Dox), PRDM1β, IRF4, and c-MYC expression was reduced by bortezomib (Bor) both at transcriptional (top panel) and protein (bottom panel) level. (E) In HUT102 cells resistant to 6-mercaptopurine (6MP, 50 μM), PRDM1β, IRF4, and c-MYC expression was also reduced by bortezomib (Bor, 25 nM) (top panel). In MOLT4 cells, when methotrexate resistance was developed (MTX, 150 nM), PRDM1β was expressed, and subsequently reduced by bortezomib (Bor, 25 nM) (bottom panel). (F) Immunofluorescence study revealed that NF-κB (P65) was located mainly in nucleus in doxorubicin (Dox)–treated HUT78 cells, while in cytoplasm in those treated with bortezomib (Bor). Leica AS LMD, 100×/1.3 oil, oil/1.3, Immunofluorescent stain, Video camera 3CCD Hitachi HV-Dz0P (Hitachi, Tokyo, Japan), Leica AS LMD software, version 4.4. (G) Bortezomib (Bor) blocked NF-κB nuclear translocation and retained the phosphorylated form of IκBα (p-IκBα) and IκBα in the cytoplasm of HUT78 cells. Lamin B was used as a nuclear protein control. (H and I) Addition of NF-κB inhibitor PDTC increased the antiproliferative effect of doxorubicin (Dox) on HUT78 cells (H) and induced PRDM1β down-regulation (I).
PRDM1 was expressed in T-cell lymphoma and could be down-regulated by bortezomib through NF-κB inactivation. (A) Nuclear PRDM1 protein expression was revealed by immunohistochemistry on lymphoma tissue. Leica AS LMD (Leica Microsystems), 40×/0.6 CORR XT, air/0.6, hematoxylin-eosin stain, Video camera 3CCD Hitachi HV-Dz0P, Leica AS LMD software, version 4.4. (B) PRDM1 mRNA and protein expression were detected by semiquantitative PCR on lymphoma cells and Western blot on lymphoma tissue, respectively. PRDM1 isoforms were expressed in laser-microdissected lymphoma cells and T- and B-lymphoma cell lines (NA indicates namalwa; SU, SU-DHL-4), but not in peripheral blood lymphocytes (PBLs). (C) Laser-microdissected lymphoma cells showed coexpression of PRDM1 and IRF4. (D) In HUT78 cells resistant to doxorubicin (Dox), PRDM1β, IRF4, and c-MYC expression was reduced by bortezomib (Bor) both at transcriptional (top panel) and protein (bottom panel) level. (E) In HUT102 cells resistant to 6-mercaptopurine (6MP, 50 μM), PRDM1β, IRF4, and c-MYC expression was also reduced by bortezomib (Bor, 25 nM) (top panel). In MOLT4 cells, when methotrexate resistance was developed (MTX, 150 nM), PRDM1β was expressed, and subsequently reduced by bortezomib (Bor, 25 nM) (bottom panel). (F) Immunofluorescence study revealed that NF-κB (P65) was located mainly in nucleus in doxorubicin (Dox)–treated HUT78 cells, while in cytoplasm in those treated with bortezomib (Bor). Leica AS LMD, 100×/1.3 oil, oil/1.3, Immunofluorescent stain, Video camera 3CCD Hitachi HV-Dz0P (Hitachi, Tokyo, Japan), Leica AS LMD software, version 4.4. (G) Bortezomib (Bor) blocked NF-κB nuclear translocation and retained the phosphorylated form of IκBα (p-IκBα) and IκBα in the cytoplasm of HUT78 cells. Lamin B was used as a nuclear protein control. (H and I) Addition of NF-κB inhibitor PDTC increased the antiproliferative effect of doxorubicin (Dox) on HUT78 cells (H) and induced PRDM1β down-regulation (I).
Using semiquantitative PCR, PRDM1α and PRDM1β transcripts were identified in laser-microdissected lymphoma cells (Figure 1B) of 27 and 14 patients, respectively. PRDM1α mRNA was detected in a higher number of patients (27/60) than PRDM1 protein (19/60). A similar discrepancy was also reported in B-cell lymphoma.10 Although systematic sequencing of PRDM1 in 30 patients with adequate frozen tissue samples revealed no mutation, other genetic/epigenetic inactivation as well as defects in protein translation or stability might contribute to the lack of PRDM1 protein expression. Instead, PRDM1β mRNA was detected in 14 of 19 cases positive for PRDM1 protein. The constant association between PRDM1β mRNA and PRDM1 protein led us to further consider the role of this altered isoform in T-cell lymphoma.
IRF4 was significantly related to PRDM1 transcripts: it was higher in PRDM1α+PRDM1β+ (14/14, 100%) and PRDM1α+PRDM1β− cases (11/13, 84.6%), than in PRDM1α−PRDM1β− cases (8/33, 24.2%; P = .008 and P = .024, respectively). Laser-microdissected lymphoma cells revealed IRF4 coexpressing with PRDM1α and PRDM1β (Figure 1C). Responsible for B-cell differentiation, IRF4 is expressed in neoplastic activated T cells and regulates T-cell function and transformation.11-14 This IRF4-PRDM1 coexpression confirmed that PRDM1 happens with IRF4 in T-cell lymphoma.
PRDM1β reflected poor disease outcome
PRDM1β, but not PRDM1α, was significantly related to advanced Ann Arbor stage (P = .033), high-risk International Prognostic Index (P = .035, Table 1), and shorter survival times. The 3-year event-free survival and overall survival rates (± SE percentage) were significantly shorter for PRDM1α+PRDM1β+ patients (23.1% [± 11.7%] and 55.6% [± 14.9%]) than for PRDM1α+PRDM1β− cases (48.5% [± 16.6%] and 87.5% [± 11.7%]) (P = .040 and P = 0.018, respectively). Therefore, like its analog PRDM2 (RIZ) and PRDM3 (MDS1-EVI1) genes, each expressing a truncated protein missing the PR domain and critical for oncogenesis,17,18 PRDM1β indicated poor disease outcome in T-cell lymphoma.
Proteasome inhibitor bortezomib down-regulated PRDM1β through NF-κB inactivation
HUT78 cells were resistant to doxorubicin, but sensitive to bortezomib. In a 6-hour incubation with bortezomib, either alone or with doxorubicin, PRDM1β, but not PRDM1α, was down-regulated. IRF4 and c-MYC were also decreased after 12-hour treatment. Their protein levels followed a similar reduction, observed from 12 to 24 hours after treatment (Figure 1D). In addition, such alternation was also revealed in 6-mer-captopurine–resistant HUT102 cells and methotrexate-resistant MOLT4 subclone (Figure 1E). Bortezomib, the first proteasome inhibitor used in the clinic, has recently been reported as effective in T-cell lymphoma.19-21 PRDM1β down-regulation, with the subsequent inhibition of c-MYC and IRF4, could be one of the possible molecular mechanisms of its action.
PRDM1 is a downstream target of NF-κB,22 whose activation induces T-lymphoma cell resistance to chemotherapy.23,24 Nuclear localization of NF-κB, required for target gene transactivation, was studied by immunofluorescence assay and showed an inhibition after 12-hour treatment of bortezomib (Figure 1F). This was confirmed on Western blot, with decrease of nuclear NF-κB protein (Figure 1G). Further analysis of cytoplasmic IκBα revealed striking differences: it decreased under doxorubicin, while increasing under bortezomib treatment. Together, increasing cytoplasmic IκBα, concomitant with blockade of NF-κB nuclear translocation, suggested NF-κB inactivation in T-lymphoma cells treated with bortezomib.25
To further test this hypothesis, we associated PDTC, a NF-κB inhibitor, with doxorubicin in T-lymphoma cell cultures. Growth inhibition (Figure 1H) and the parallel decrease of PRDM1β (Figure 1I) could be reproduced when treated with bortezomib. We thus confirmed that NF-κB activity was responsible for PRDM1β down-regulation by bortezomib.
In conclusion, abnormal PRDM1β expression was correlated with poor disease outcome in T-cell lymphoma patients. Bortezomib could down-regulate PRDM1β through NF-κB inactivation. The value of proteasome inhibitor as a therapeutic strategy should be further assessed in T-cell lymphoma, especially those cases refractory to conventional chemotherapy.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported in part by the Chinese National Key Program for Basic Research (973:2004CB518600), the Chinese National High Tech Program (863:2006AA02A301 and 863:2006AA02A405), the National Natural Science Foundation of China (30750335), the Key Discipline Program of Shanghai Municipal Education Commission (Y0201), the Shanghai Commission of Science and Technology (44107025), the Shanghai Rising Star Program (05QMX1429), the Program for New Century Excellent Talents in University, the Scientific Research Foundation for the Returned Overseas Chinese Scholars, the Program de Recherches Avancées (PRA B 06-01), and the Samuel Waxman Cancer Research Foundation Laboratory, the Co-PI Program of Shanghai Rui Jin Hospital/Medical School of Shanghai Jiao Tong University.
Authorship
Contribution: W.-L.Z., Z.C., A.J., and S.-J.C. designed the research and wrote the paper; Y.-Y.L., Q.-L.Z., L.W., C.L., and Y.-W.Z. performed research and statistical analysis; J.M. and J.-F.G. contributed vital new reagents; J.-M.L., Y.-P.S., and Z.-X.S. collected, analyzed, and interpreted data.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Sai-Juan Chen, State Key Laboratory of Medical Genomics, Shanghai Institute of Hematology, Rui Jin Hospital, Shanghai Jiao Tong University School of Medicine, 197 Rui Jin Er Road, Shanghai 200025, China; e-mail: sjchen@stn.sh.cn; or Anne Janin, Inserm U728, Laboratoire de Pathology, Hôpital Saint Louis, 1 Avenue Claude Vellefaux, Paris 75010, France; e-mail: anne_janin@yahoo.com.
References
Author notes
W.-L.Z., Y.-Y.L., Q.-L.Z., and L.W. contributed equally to this work.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal