Various clinical prognostic scoring systems (PSSs) have been suggested as means of selecting high-risk chronic idiopathic myelofibrosis (CIMF) patients at diagnosis. The WHO has recently proposed strict diagnostic criteria for CIMF, and the European consensus for bone marrow fibrosis (BMF) grading recommends 4 classes. It has been suggested that BMF grading may play a prognostic role in CIMF, but it has never been compared with the other PSSs in the same patients. We tested a prognostic model for overall survival (OS) based on the WHO criteria and BMF grading in 113 consecutive patients with chronic myeloproliferative disorders (98 with CIMF and 15 with postpolycythemic myelofibrosis), and compared the findings with those of PSSs. The results showed that our model is significantly associated with different OSs and, unlike the other PSSs, clearly discriminates the OS of intermediate- and high-risk patients.
Introduction
The pathogenesis of chronic idiopathic myelofibrosis (CIMF), a chronic myeloproliferative disorder (CMPD), involves a pluripotent hematopoietic progenitor cell that induces the deposition of fibrin and collagen in bone marrow via the release of angiogenic factors.1,–3 Its main clinicopathological characteristics are progressive anemia, leukocytosis or leukopenia, increased levels of circulating CD34+ hematopoietic progenitor cells, constitutional symptoms, bone marrow fibrosis with neovascularization, and marked splenomegaly with extramedullary hematopoiesis.1,2,4,–6 The patients' median age at diagnosis is 60 years,7 and transformation to acute leukemia occurs in 15% of cases with an extremely poor prognosis.3,8–9
A number of prognostic scoring systems (PSSs) based on clinical variables (platelet count, leukocyte count, monocyte count, circulating blasts, hemoglobin level, systemic symptoms, and hepato/splenomegaly) have been proposed as means of selecting high-risk patients at diagnosis who may be eligible for intensive treatments.1,4,7,10,–12 Three of these (the Mayo,12 Cervantes,10 and Dupriez11 PSSs) have been compared in the same series of patients, and were all found to have significant prognostic value, although the results of the Mayo PSS12 were the most solid.
The WHO has recently proposed strict diagnostic criteria for CIMF,13 and a European consensus has recommended the 4-class grading of bone marrow fibrosis (BMF) as assessed by trephine bone marrow biopsies (BMBs).14 The prognostic role of BMF grading has been suggested in CIMF subsets, but it has never been compared with the other PSSs in the same patients.
We therefore generated a prognostic model for overall survival (OS) based on the WHO classification and the European consensus for BMF grading, assuming that BMF is a sound marker of disease progression and that the clinical variables used in other PSSs are consequences of this event. This hypothesis was tested in a representative series of 113 consecutive CMPD patients, and the results were compared with those obtained using all of the known validated PSSs: Mayo,12 Dingli,12 Cervantes,10 and Dupriez.11
Methods
This study was approved by the Fondazione IRCCS Ospedale Maggiore, Mangiagalli e Regina Elena Institutional Review Board. Informed consent was obtained in accordance with the Declaration of Helsinki.
Patients
The study involved 113 consecutive CMPD patients (61 males and 52 females; M/F ratio: 1.2; median age: 67 years [range: 27–86 years]), who were diagnosed between 1996 and 2006 (median follow-up: 19 months; range: 1–126 months), and classified on the basis of the WHO criteria.13 Ninety-eight had CIMF and 15 had postpolycythemic myelofibrosis and myeloid metaplasia (PPMM); the latter group was analyzed separately. On the basis of the European consensus on BMF grading,14 33 of the CIMF cases were classified as CIMF-0; 27, as CIMF-1; 26, as CIMF-2; and 12, as CIMF-3. Clinical data were available for all of the patients (Table 1), all of whom were Philadelphia chromosome negative (Ph−).
Clinical data at diagnosis
| . | CIMF-0 . | CIMF-1 . | CIMF-2 . | CIMF-3 . | PPMM . |
|---|---|---|---|---|---|
| No. of patients | 33 | 27 | 26 | 12 | 15 |
| Median age, y (range) | 66 (27–80) | 67 (29–84) | 71 (45–86) | 71 (60–85) | 64 (45–85) |
| M/F, ratio | 16/17 (0.94) | 14/13 (1.08) | 16/10 (1.6) | 7/5 (1.4) | 8/7 (1.14) |
| Hb level, g/L, median (range) | 139 (68–170) | 118 (76–167) | 116 (62–163) | 105 (76–141) | 116 (88–153) |
| Hb level less than 100 g/L, no. of pts (%) | 1 (3) | 7 (26) | 11 (42) | 5 (42) | 4 (27) |
| Plt count, ×109/L, median (range) | 746 (289–1546) | 521 (4–1289) | 430 (88–1470) | 187 (17–489) | 282 (31–903) |
| Plt count less than 100×109/L, no. of pts (%) | 0 (0) | 3 (11) | 2 (8) | 3 (25) | 2 (13) |
| WBC count, ×109/L, median (range) | 9.5 (5.9–41.6) | 7.6 (1.9–20.6) | 10.8 (1.9–25.2) | 9.8 (1.9–39.4) | 8.9 (2.8–34) |
| WBC count less than 4 or higher than 30×109/L, no. of pts (%) | 1 (3) | 2 (7) | 3 (11) | 2 (17) | 2 (13) |
| AMC 1×109/L or higher, no. of pts (%) | 5 (15) | 1 (4) | 3 (11) | 2 (17) | 1 (7) |
| Circulating blasts 1% or more, no. of pts (%) | 4 (12) | 7 (26) | 14 (54) | 7 (58) | 9 (60) |
| Constitutional symptoms, no. of pts (%) | 0 (0) | 3 (11) | 3 (11) | 1 (8) | 1 (7) |
| No. of deaths (%) | 0 (0) | 3 (11) | 4 (15) | 6 (50) | 2 (13) |
| Mayo PSS,12 no. of pts (%) | |||||
| LR | 28 (85) | 20 (74) | 12 (46) | 4 (33) | 10 (67) |
| IR | 4 (12) | 2 (7) | 11 (42) | 4 (33) | 2 (13) |
| HR | 1 (3) | 5 (19) | 3 (12) | 4 (33) | 3 (20) |
| Dingli PSS,12 no. of pts (%) | |||||
| LR | 33 (100) | 20 (74) | 15 (58) | 5 (42) | 10 (67) |
| IR | 0 (0) | 3 (11) | 8 (31) | 4 (33) | 3 (20) |
| HR | 0 (0) | 4 (15) | 3 (11) | 3 (25) | 2 (13) |
| Cervantes PSS,10 no. of pts (%) | |||||
| LR | 33 (100) | 24 (89) | 18 (69) | 8 (67) | 11 (73) |
| HR | 0 (0) | 3 (11) | 8 (31) | 4 (33) | 4 (27) |
| Dupriez PSS,11 no. of pts (%) | |||||
| LR | 32 (97) | 20 (74) | 15 (58) | 6 (50) | 10 (67) |
| IR | 0 (0) | 5 (19) | 8 (31) | 5 (42) | 4 (27) |
| HR | 1 (3) | 2 (7) | 3 (11) | 1 (8) | 1 (6) |
| . | CIMF-0 . | CIMF-1 . | CIMF-2 . | CIMF-3 . | PPMM . |
|---|---|---|---|---|---|
| No. of patients | 33 | 27 | 26 | 12 | 15 |
| Median age, y (range) | 66 (27–80) | 67 (29–84) | 71 (45–86) | 71 (60–85) | 64 (45–85) |
| M/F, ratio | 16/17 (0.94) | 14/13 (1.08) | 16/10 (1.6) | 7/5 (1.4) | 8/7 (1.14) |
| Hb level, g/L, median (range) | 139 (68–170) | 118 (76–167) | 116 (62–163) | 105 (76–141) | 116 (88–153) |
| Hb level less than 100 g/L, no. of pts (%) | 1 (3) | 7 (26) | 11 (42) | 5 (42) | 4 (27) |
| Plt count, ×109/L, median (range) | 746 (289–1546) | 521 (4–1289) | 430 (88–1470) | 187 (17–489) | 282 (31–903) |
| Plt count less than 100×109/L, no. of pts (%) | 0 (0) | 3 (11) | 2 (8) | 3 (25) | 2 (13) |
| WBC count, ×109/L, median (range) | 9.5 (5.9–41.6) | 7.6 (1.9–20.6) | 10.8 (1.9–25.2) | 9.8 (1.9–39.4) | 8.9 (2.8–34) |
| WBC count less than 4 or higher than 30×109/L, no. of pts (%) | 1 (3) | 2 (7) | 3 (11) | 2 (17) | 2 (13) |
| AMC 1×109/L or higher, no. of pts (%) | 5 (15) | 1 (4) | 3 (11) | 2 (17) | 1 (7) |
| Circulating blasts 1% or more, no. of pts (%) | 4 (12) | 7 (26) | 14 (54) | 7 (58) | 9 (60) |
| Constitutional symptoms, no. of pts (%) | 0 (0) | 3 (11) | 3 (11) | 1 (8) | 1 (7) |
| No. of deaths (%) | 0 (0) | 3 (11) | 4 (15) | 6 (50) | 2 (13) |
| Mayo PSS,12 no. of pts (%) | |||||
| LR | 28 (85) | 20 (74) | 12 (46) | 4 (33) | 10 (67) |
| IR | 4 (12) | 2 (7) | 11 (42) | 4 (33) | 2 (13) |
| HR | 1 (3) | 5 (19) | 3 (12) | 4 (33) | 3 (20) |
| Dingli PSS,12 no. of pts (%) | |||||
| LR | 33 (100) | 20 (74) | 15 (58) | 5 (42) | 10 (67) |
| IR | 0 (0) | 3 (11) | 8 (31) | 4 (33) | 3 (20) |
| HR | 0 (0) | 4 (15) | 3 (11) | 3 (25) | 2 (13) |
| Cervantes PSS,10 no. of pts (%) | |||||
| LR | 33 (100) | 24 (89) | 18 (69) | 8 (67) | 11 (73) |
| HR | 0 (0) | 3 (11) | 8 (31) | 4 (33) | 4 (27) |
| Dupriez PSS,11 no. of pts (%) | |||||
| LR | 32 (97) | 20 (74) | 15 (58) | 6 (50) | 10 (67) |
| IR | 0 (0) | 5 (19) | 8 (31) | 5 (42) | 4 (27) |
| HR | 1 (3) | 2 (7) | 3 (11) | 1 (8) | 1 (6) |
CIMF indicates chronic idiopathic myelofibrosis; PPMM, postpolycythemic myelofibrosis and myeloid metaplasia; Hb, hemoglobin; Plt, platelet; WBC, white blood cell; AMC, absolute monocyte count; PSS, prognostic scoring system; LR, low risk; IR, intermediate risk; and HR, high risk.
The patients were divided into prognostic groups using the 4 PSSs. The Mayo PSS12 is structurally organized into low-risk (LR), intermediate-risk (IR), and high-risk (HR) categories, and considers the clinical variables of hemoglobin (Hb) level (< 100 g/L [10 g/dL]), white blood cell (WBC) count (< 4 or > 30 × 109/L), platelet (Plt) count (< 100 × 109/L), and absolute monocyte count (AMC; ≥ 1 × 109/L). The Dingli PSS12 is organized into LR, IR, and HR groups, and considers Hb level (< 100 g/L [10 g/dL]), WBC count (< 4 or > 30 × 109/L), and Plt count (< 100 × 109/L). The Cervantes PSS10 is structurally organized into LR and HR categories, and considers Hb level (< 100 g/L [10 g/dL]), constitutional symptoms, and circulating blasts (≥ 1%). The Dupriez PSS11 is structurally organized into LR, IR, and HR categories, and considers Hb level (< 100 g/L [10 g/dL]) and WBC count (< 4 or > 30 × 109/L).
Bone marrow histology
Formalin-fixed, paraffin-embedded trephine BMB specimens of the posterior superior iliac spine taken at diagnosis were available for all of the patients. The sections were stained with hematoxylin-eosin, Giemsa, Gomori silver impregnation, and Masson trichrome to evaluate their morphology and BMF grading.14
Our 98 CIMF and 15 PPMM cases were selected on the basis of the WHO criteria13 by 2 experienced hemopathologists (U.G., L.B.). In relation to the problem of differentiating essential thrombocythemia (ET) from the cellular phase of CIMF (CIMF-0), the latter is characterized by hypercellular marrow for the patient's age, with an increase in the number of neutrophils and atypical megakaryocytes (ie, megakaryocytes ranging in size from small to large and giant, and with striking maturation abnormalities, “cloud-like” lobulation of nuclei, and naked nuclei), frequently aggregated in clusters.
Our series of prefibrotic CIMF included cases with these features but simultaneously presenting dense clusters of megakaryocytes (ie, 3 or more megakaryocytes touching each other) with maturation defects and “cloudlike” nuclei. We have recently reported that these megakaryocytic morphologic features are more frequently associated with the cellular phase of CIMF than with ET.15 In our laboratory, interobserver agreement when considering these specific megakaryocytic features is approximately 80% (U.G., unpublished data, May 2006).
Reticulin staining was scored using a scale from 0 to 3 according to the European consensus on BMF grading.14 To increase interobserver agreement in relation to fibrosis grading, a consensus discussion was first held during which some cases were reviewed together using a double-headed microscope to ensure uniform assessment criteria. Subsequently, the fibrosis of each case was microscopically graded independently by the 2 observers who had no knowledge of the clinical data except for the previous CMPD diagnosis. Agreement was 82.3% (93/113 cases) and then the discordant cases were re-examined at the double-headed microscope and a consensus was obtained.
The control group consisted of 20 trephine BMBs obtained for staging purposes or for nonneoplastic miscellaneous conditions, and found to be free of neoplasias and abnormalities at histologic examination.
Statistical analysis
The clinicopathological relationships were examined univariately by cross-tabulation using the χ2 test for discontinuous variables, and the Kruskal-Wallis and Mann-Whitney tests for continuous variables. The OS curves were calculated according to Kaplan-Meier and compared by the log-rank test. A P value less than .05 was considered significant.
Results and discussion
Considering the 4 BMF classes, the patients in lower CIMF stages more frequently presented an absence of circulating blasts (χ2 test: P = .002), more favorable Hb level (Kruskal-Wallis test: P < .001), platelet count (Kruskal-Wallis test: P < .001), and lactate dehydrogenase (LDH) level (Kruskal-Wallis test: P < .001), and less spleen (Kruskal-Wallis test: P < .001) and liver (Kruskal-Wallis test: P < .001) enlargement, whereas higher BMF grades were more frequent in the higher risk groups of the PSSs (χ2 test: Mayo: P = .04; Dingli: P = .004; Cervantes: P = .005; Dupriez: P = .006).
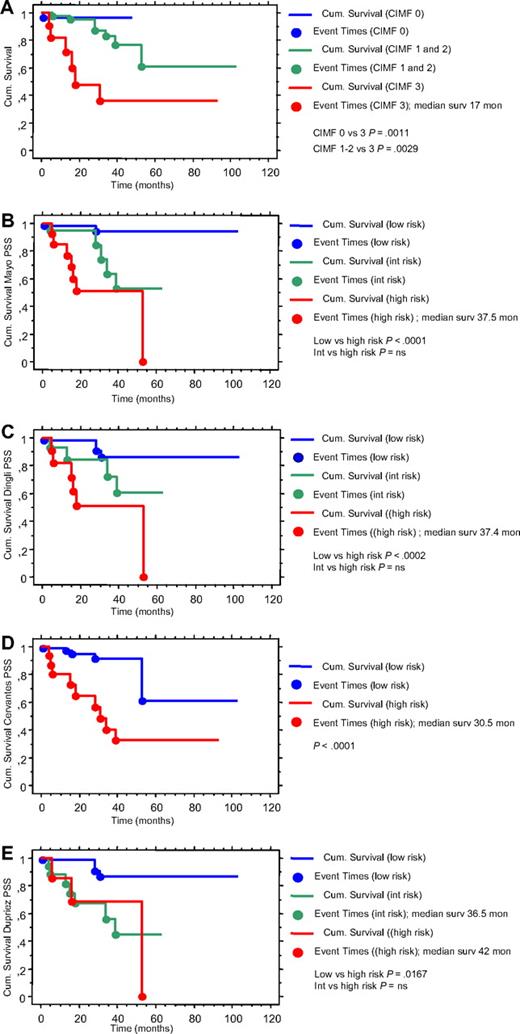
OS was significantly less in the patients with CIMF-3 than in those with CIMF-0 or CIMF-1 + 2 (Kaplan-Meier analysis, log-rank test: P = .001 and P = .003, respectively), and similar in the CIMF-3 and PPMM patients (Figure 1). The results of our prognostic model were therefore similar to those reported by Tefferi et al,12 who showed that survival was less in the HR than in the LR and IR patients defined by the Mayo,12 Cervantes,10 and Dupriez11 PSSs.
Comparative survival using the different prognostic scoring systems (PSSs). Kaplan-Meyer survival curves in primary myelofibrosis based on the different PSSs: (A) WHO classification and European consensus for BMF grading13,14 ; (B) Mayo PSS12 ; (C) Dingli PSS12 ; (D) Cervantes PSS10 ; and (E) Dupriez PSS.11 Using the WHO classification and European consensus for BMF grading, CIMF-0 showed significantly better survival than CIMF-3, and CIMF-1/2 (grouped) showed significantly better survival than CIMF-3; using the Mayo,12 Dingli,12 and Dupriez11 PSSs, there were no differences between the intermediate- and high-risk classes (the Cervantes PSS10 identifies only 2 risk classes).
Comparative survival using the different prognostic scoring systems (PSSs). Kaplan-Meyer survival curves in primary myelofibrosis based on the different PSSs: (A) WHO classification and European consensus for BMF grading13,14 ; (B) Mayo PSS12 ; (C) Dingli PSS12 ; (D) Cervantes PSS10 ; and (E) Dupriez PSS.11 Using the WHO classification and European consensus for BMF grading, CIMF-0 showed significantly better survival than CIMF-3, and CIMF-1/2 (grouped) showed significantly better survival than CIMF-3; using the Mayo,12 Dingli,12 and Dupriez11 PSSs, there were no differences between the intermediate- and high-risk classes (the Cervantes PSS10 identifies only 2 risk classes).
In our patients, all 4 PSSs identified differences in survival between the HR and the LR and IR classes (Kaplan-Meier cumulative survival; log-rank test: Cervantes10 : P = .001, Mayo12 : P = .001, Dingli12 : P = .001, Dupriez11 : P = .001) but, unlike our model, the PSSs that select 3 risk classes (Mayo,12 Dingli,12 Dupriez11 ) failed to identify differences in survival between the IR and HR patients (Figure 1).
Two important studies have investigated the prognostic relevance of BMF in CIMF in large series of CMPD patients,2,7 but their end points were significantly different from ours (ie, the impact of the WHO classification and BMF grading on OS). In assessing the prognostic role of BMF on event-free survival, Kreft et al16 did not apply any grading score and considered only patients older than 59 years, and Thiele and Kvasnicka17 correlated BMF grading with clinical hematologic data. The latter found a significant difference in the levels of hemoglobin, leukocytes, thrombocytes, peripheral blasts (erythroblasts and myeloblasts), and LDH, as well as in the extent of splenomegaly and hepatomegaly, between the cases with lower (CIMF-0) and higher (CIMF-2 and CIMF-3) degrees of BMF, and also suggested that BMF grading plays a role in prognosis. The statistical significance of their findings was not declared.
More importantly, neither of these studies directly compared BMF grading as a prognostic model with all of the other proposed and validated PSSs.
Finally, as previously reported in the paper by Wilkins et al,18 the grading of bone marrow fibrosis showed good interobserver agreement, although it could be further increased by training in the application of strict diagnostic criteria.
In conclusion, we found that the WHO classification and the European consensus for BMF grading, used as a prognostic parameter in CIMF, were significantly associated with different survival in our series of patients and, unlike the other PSSs, our model clearly distinguished OS in IR and HR patients. If validated in a larger series of patients, the results of this analysis may have a significant impact on current CIMF prognostication.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: C.V. designed and performed the study, analyzed the data, and wrote the paper; N.S.F. designed the study, analyzed the data, and wrote the paper; U.G. designed and performed the study, analyzed the data, and wrote the paper; R.C., F.R., A.I., S.C., and G.G. performed the study; L.B. and G.L.D. performed the study and analyzed the data.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Claudia Vener, U.O. Ematologia I–Centro Trapianti di Midollo, Fondazione IRCCS Ospedale Maggiore, Mangiagalli e Regina Elena, Via Francesco Sforza 35, 20122 Milano, Italy; e-mail: claudiavener@tiscali.it.
References
Author notes
C.V. and N.S.F. contributed equally to this work.