Abstract
Introduction: HSE is a rare but very severe central nervous system (CNS) infection caused by Herpes simplex virus type 1 (HSV-1) in almost all cases, and characterized by a high morbidity and mortality rate (97 and 70% without therapy, respectively). Immunosuppression, is a known risk factor and both early diagnosis and treatment are critical points for a good outcome in this setting. Hereby we reported two cases of HSE after alloHSCT.
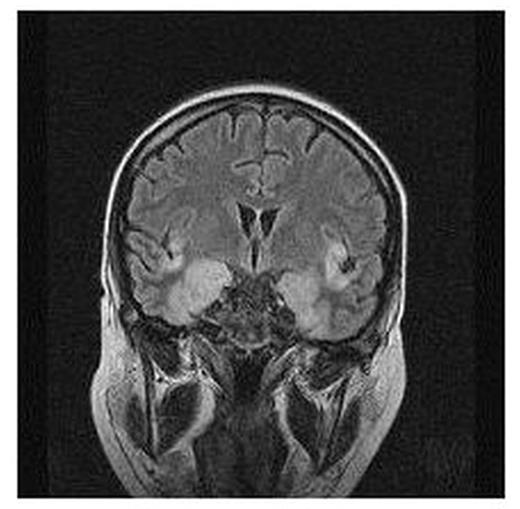
Patients: A 35-year-old female with relapsed multiple myeloma, underwent alloHSCT from a matched unrelated donor (MUD). On day +120, she developed an acute onset of fever, drowsiness, and generalized seizures. After 48 hours, a rapid deterioration of neurological symtoms was observed and the brain MRI showed acute encephalitis with high signal intensity in the temporal lobe and insula cortex (fig. 1). The HSV-PCR from cerebrospinal fluid (CSF) was positive for HSV-1, and a treatment with acyclovir 30 mg/Kg/d was initiated, 72 hours after the hospital admission. A 66 year-old male with high risk AML underwent MUD alloHSCT. Thirteen months after transplant, an acute sialoadenitis and HSV-1 gengivostomatitis occurred, followed by fever and focal seizures. Since typical lesions of HSE were demonstrated by brain MRI, antiviral therapy with aciclovir was promptly administrated, within 24 hours from the symptoms onset. HSV-PCR on CSF was performed two days later, and proved negative, probably due to ongoing antiviral therapy and delay to CSF analysis. After 21 days of antiviral treatment, both patients recovered from the acute phase, but in the first case we observed serious neurological sequelae that required prolonged unsuccessful cognitive rehabilitation. The second patient didn’t experienced significant residual neurological impairment, and didn’t require any other supportive measure. Both pts have had chronic GVHD and received prolonged courses of immunosuppressive therapy; they experienced recurrent CMV infections thereafter, and were under high dose foscarnet therapy at the diagnosis of HSE, but without HSV prophylaxis.
Conclusion: the time from diagnosis-to-antiviral therapy, and the level of consciousness at the onset of symptoms are two major risk factors impairing morbidity and mortality of HSE. In heavily immunosuppressed alloHSCT pts with initial focal neurological signs, an early and aggressive diagnostic approach should be performed as emergency, even if they are under anti-CMV therapy; prompt acyclovir administration is therefore warranted in these settings, in order to prevent severe disability or mortality.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal