The t(11;14)(p13;q11) is presumed to arise from an erroneous T-cell receptor delta TCRD V(D)J recombination and to result in LMO2 activation. However, the mechanisms underlying this translocation and the resulting LMO2 activation are poorly defined. We performed combined in vivo, ex vivo, and in silico analyses on 9 new t(11;14)(p13;q11)-positive T-cell acute lymphoblastic leukemia (T-ALL) as well as normal thymocytes. Our data support the involvement of 2 distinct t(11;14)(p13;q11) V(D)J-related translocation mechanisms. We provide compelling evidence that removal of a negative regulatory element from the LMO2 locus, rather than juxtaposition to the TCRD enhancer, is the main determinant for LMO2 activation in the majority of t(11;14)(p13;q11) translocations. Furthermore, the position of the LMO2 breakpoints in T-ALL in the light of the occurrence of TCRD-LMO2 translocations in normal thymocytes points to a critical role for the exact breakpoint location in determining LMO2 activation levels and the consequent pressure for T-ALL development.
Introduction
The t(11,14)(p13;q11) (LMO2-TCRD) occurs frequently (7%) and is considered a paradigm for T-cell receptor (TCR)-associated translocations in human T-cell acute lymphoblastic leukemia (T-ALL).1,2 Although the causative mechanism is still poorly understood, it is generally assumed to result from erroneous V(D)J recombination during T-cell development.3 So far only 5 t(11;14)(p13;q11) junctions have been sequenced.4,,,,–9 In 3 cases, cryptic sequences resembling TCR/Ig recombination signal sequences (RSSs) were located next to the LMO2 breakpoint. Two of these concerned the same cryptic RSS (cRSS). Consequently, RAG mistargeting of an LMO2 cRSS at the moment of TCRD recombination was proposed as the causal mechanism.4,,–7 Recently, we and others demonstrated that this shared LMO2 cRSS could indeed function as target for V(D)J recombination in ex vivo recombination assays.10,11 Although these data fit with illegitimate V(D)J recombination due to RAG mistargeting, they are clearly too limited to draw firm conclusions regarding recurrent involvement of this mechanism in t(11;14)(p13;q11)
Dogmatically, TCR-associated translocations are believed to result in protooncogene activation due to juxtaposition to a TCR enhancer or other regulatory elements.1,12 LMO2 consists of 6 exons and is transcribed from 2 promoters, a distal promoter upstream of exon 1 and a proximal promoter upstream of exon 3, with both transcripts encoding the same protein.13 Strikingly, our retrospective analysis of published t(11;14)(p13;q11) translocation junctions4,,,–8 revealed no juxtaposition of LMO2-coding exons to the TCRD enhancer, suggesting alternative LMO2 activation mechanisms. Distal promoter/negative regulatory element (NRE) removal has been suggested as an LMO2 activation mechanism in t(11;14)(p13;q11)13,14 but this has never been shown experimentally.
Clearly, many issues regarding how t(11;14)(p13;q11) leads to LMO2 activation and T-ALL are so far poorly understood. At least 4 factors must govern the occurrence of recurrent oncogenic translocations: (1) the presence of a specific site/region prone to double-strand DNA breakage through structural features and/or enzymatic deregulation; (2) the chromatin accessibility of this site to mechanisms and/or agents generating double-strand DNA breaks; (3) the posttranslocation configuration of the derivative chromosomes allowing overexpression or ectopic expression of the oncogene; and (4) growth or survival advantage of the translocation. We therefore performed a comprehensive study in both malignant and normal thymocytes using in vivo, ex vivo, and in silico approaches to integrate these factors for t(11;14)(p13;q11).
Patients, materials, and methods
T-ALL and normal human thymocyte subsets
Eight childhood T-ALLs (tumor load > 90%), with t(11;14)(p13;q11) or atypical TCRD rearrangements suggestive of chromosomal abnormalities,15 and the T-cell line TALL-104 were used. Thymocyte subsets were isolated (> 90% pure) as described.16 Samples were obtained according to informed-consent guidelines in accordance with the Declaration of Helsinki, with institutional research board approval of all involved research centers.
Translocation breakpoint analysis
To molecularly characterize translocation junctions, ligation-mediated polymerase chain reaction (LM-PCR) was performed.15
Functionality of LMO2 cRSSs
Ex vivo recombination substrate assay.
Patient-specific LMO2 breakpoint regions were cloned in recombination constructs (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article)11 and transfected (SuperFect; Qiagen, Hilden, Germany) into 3T3 fibroblasts together with RAG1/RAG2 expression vectors. Recombination status of the constructs was analyzed after 48 hours.11
The RIC algorithm.
The recombination information content (RIC) algorithm predicts the recombinogenic potential of RSSs from Ig/TCR loci and can be used to identify functional cRSSs.17 Using the RSS Project Data Base Search program,18 we determined RIC scores for LMO2 cRSSs we found functional ex vivo. Furthermore, we analyzed the LMO2 locus (−10 kb to +30 kb) for the occurrence of 12-bp and 23-bp cRSSs predicted to be functional according to the RIC score.
LMO2 expression
LMO2 transcripts were determined by real-time quantitative PCR (RQ-PCR) and quantified by normalization against ABL.16
The t(11,14)(p13;q11) in healthy thymi
Two representative LMO2 cRSSs (cRSSa and cRSSb) were selected and analyzed for involvement in t(11;14)(p13;q11) in healthy human thymocytes from 4 different thymi. Nested PCR was performed on thymocyte DNA with Dδ2/LMO2 translocus primers followed by Southern blot analysis using a γ-ATP-labeled upstream Dδ2 probe. Primers and probes are available upon request.
Results and discussion
All 9 T-ALLs revealed TCRD/LMO2 recombination (Figure S2). LMO2 breakpoints localized throughout the gene, but clustering around the distal promoter was apparent (Figure 1A). Based on heptamer-sequence resemblance, 6 cases contained a cRSS near the LMO2 breakpoint (Figure S2; Table 1), suggestive of illegitimate V(D)J recombination due to RAG mistargeting. T068 and 647 showed involvement of the same cRSS previously identified in 2 other t(11;14)(p13;q11) T-ALLs.6,7 Efficient rearrangement normally only occurs between gene segments flanked by a 12-bp RSS and a 23-bp RSS, a restriction known as the 12/23 rule.20 We inferred the 12/23 nature of the potential cRSS (Figure S2; Table 1) and selected the recombination substrates with the appropriate authentic Dδ3 12-bp or 23-bp RSS. In case of ambiguity, both 12-bp and 23-bp RSS partners were tested. All LMO2 cRSSs specifically recombined with the authentic RSS (pathway 1), albeit with clearly different frequencies (Table 1). The 647_T068/Dδ3 construct showed the highest recombination potential, confirming its high potential as a 12-bp cRSS,10,11 whereas the other LMO2 cRSSs functioned as intermediate or weak 12-bp RSSs. The T064 cRSS functioned as a weak predicted 23-bp RSS but exhibited a high efficiency as a 12-bp RSS. Its involvement as a 23-bp RSS in T064 follows from its genomic orientation relative to the TCRD 12- and 23-bp RSSs. Additional functional 12-bp cRSSs (pathway 2) were detected (Table 1), indicating a high density of functional cRSSs in the LMO2 region.
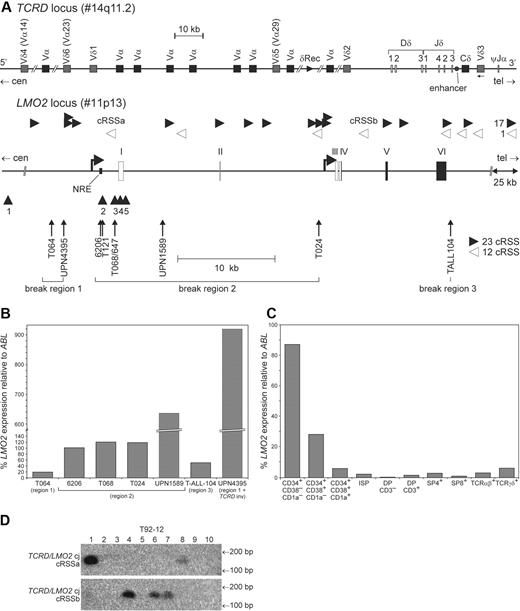
Effect of t(11;14)(p13;q11) derivative chromosome configuration on LMO2 expression in T-ALL. (A) Schematic diagram depicting the human TCRD locus that is located within the TCRA locus; V, D, and J gene segments and the TCRD enhancer are indicated. Schematic diagram of LMO2; the 6 exons are indicated (I-VI), of which the coding exons (exon IV partly, exons V and VI) are indicated in black and noncoding exons in white. The distal and proximal promoters are indicated by bent arrows, whereas NRE indicates the negative regulatory element located within the distal promoter. Exact breakpoint location of the t(11;14)(p13;q11) cases of the present study are indicated. The 3 major breakpoint regions with regard to LMO2-coding region and NRE are indicated. Arrowheads under the gene indicate molecular characterized LMO2 breakpoint regions involved in TCR-associated translocations as described in the literature: 1 = t(11,14)(p13;q11),9 ; 2 = t(7,11)(q34;p13)19 ; 3 = t(11,14)(p13;q11)6,7 and t(7;11)(q34;p13)8 ; 4 = t(11,14)(p13;q11)4,8 ; 5 = t(11,14)(p13;q11).4,5 White triangles orientated to the left and black triangles orientated to the right as depicted above the LMO2 locus indicate 12-bp cRSS and 23-bp cRSS, respectively, that were identified with the RIC algorithm and that pass the functionality threshold and are orientated in the appropriate direction for potential involvement in t(11;14)(p13;q11). The 25-kb area indicated 3′ of LMO2 contains another 17 23-bp cRSSs and 1 12-bp cRSS. (B) LMO2 RQ-PCR expression in T-ALL with t(11;14)(p13;q11) with different derivative chromosome configurations, as presented in Table 2. (C) LMO2 RQ-PCR expression in consecutive T-cell developmental stages isolated from 6 pooled human thymus samples (aged 6 wk to 3.5 y; median, 11 mo). LMO2 expression in panels B-C is normalized to the expression level of ABL and given as percentages of LMO2 expression relative to ABL expression. (D) One representative thymus demonstrating PCR/Southern blot analyses of total human thymocytes for t(11;14)(p13;q11) coding joints (CJ) due to either the involvement of cRSSa located just downstream of the LMO2 NRE and frequently involved in T-ALL or the involvement of cRSSb located in LMO2 intron 4. In total, 2 of 4 thymi tested contained t(11;14)(p13;q11), each having 2 of 10 positive PCR reactions for t(11;14)(p13;q11) involving cRSSa, whereas 1 had 2 of 10 and the other 3 of 10 positive PCR reactions for t(11;14)(p13;q11) involving cRSSb.
Effect of t(11;14)(p13;q11) derivative chromosome configuration on LMO2 expression in T-ALL. (A) Schematic diagram depicting the human TCRD locus that is located within the TCRA locus; V, D, and J gene segments and the TCRD enhancer are indicated. Schematic diagram of LMO2; the 6 exons are indicated (I-VI), of which the coding exons (exon IV partly, exons V and VI) are indicated in black and noncoding exons in white. The distal and proximal promoters are indicated by bent arrows, whereas NRE indicates the negative regulatory element located within the distal promoter. Exact breakpoint location of the t(11;14)(p13;q11) cases of the present study are indicated. The 3 major breakpoint regions with regard to LMO2-coding region and NRE are indicated. Arrowheads under the gene indicate molecular characterized LMO2 breakpoint regions involved in TCR-associated translocations as described in the literature: 1 = t(11,14)(p13;q11),9 ; 2 = t(7,11)(q34;p13)19 ; 3 = t(11,14)(p13;q11)6,7 and t(7;11)(q34;p13)8 ; 4 = t(11,14)(p13;q11)4,8 ; 5 = t(11,14)(p13;q11).4,5 White triangles orientated to the left and black triangles orientated to the right as depicted above the LMO2 locus indicate 12-bp cRSS and 23-bp cRSS, respectively, that were identified with the RIC algorithm and that pass the functionality threshold and are orientated in the appropriate direction for potential involvement in t(11;14)(p13;q11). The 25-kb area indicated 3′ of LMO2 contains another 17 23-bp cRSSs and 1 12-bp cRSS. (B) LMO2 RQ-PCR expression in T-ALL with t(11;14)(p13;q11) with different derivative chromosome configurations, as presented in Table 2. (C) LMO2 RQ-PCR expression in consecutive T-cell developmental stages isolated from 6 pooled human thymus samples (aged 6 wk to 3.5 y; median, 11 mo). LMO2 expression in panels B-C is normalized to the expression level of ABL and given as percentages of LMO2 expression relative to ABL expression. (D) One representative thymus demonstrating PCR/Southern blot analyses of total human thymocytes for t(11;14)(p13;q11) coding joints (CJ) due to either the involvement of cRSSa located just downstream of the LMO2 NRE and frequently involved in T-ALL or the involvement of cRSSb located in LMO2 intron 4. In total, 2 of 4 thymi tested contained t(11;14)(p13;q11), each having 2 of 10 positive PCR reactions for t(11;14)(p13;q11) involving cRSSa, whereas 1 had 2 of 10 and the other 3 of 10 positive PCR reactions for t(11;14)(p13;q11) involving cRSSb.
Patient-specific LMO2 cRSSs and sequencing results of recombination vectors in ex vivo recombination substrate assay
| Vector . | Patient-specific cRSSs* . | No. T† . | No. colonies‡ . | No. A§ . | V(D)J recombination pathway, % . | Break repair pathway, 4, %** . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Heptamer sequence . | Spacer length, bp . | Nonamer sequence . | 1‖ . | 2¶ . | 3# . | |||||
| 647_T068/Dδ3 | CACAGTA | 12 | GCAATAATT | 3 | 193 (∼ 64) | 28 | 78.5 | 0 | 3.5 | 18 |
| T121/Dδ3 | CACAGCA | 12 | ACCAGGGAA | 3 | 60 (∼ 20) | 26 | 31 | 4 | 4 | 61.5 |
| T024/Dδ3 | CACACTA | 12 | ACAGAAATG | 12 | 113 (∼ 9) | 110 | 4.5 | 0 | 11 | 84.5 |
| 6206/Dδ3 | CACATCA | 12 | TCTCCTACT | 14 | 78 (∼ 6) | 76 | 1 | 0 | 22 | 76 |
| 6206/Dδ3inv | CACATCA | 23 | AATTCACCA | 12 | 39 (∼ 3) | 38 | 0 | 0 | 24 | 76 |
| T064/Dδ3inv | CACAGTG | 23 | ACGCTCAAC | 5 | 103 (∼ 21) | 40 | 5 | 10 | 12.5 | 72.5 |
| T064/Dδ3 | CACAGTG | 12 | AAGACAGCC | 3 | 84 (∼ 28) | 27 | 67 | 0 | 11 | 22 |
| TALL104/Dδ3 | No cRSS | 11 | 101 (∼ 9) | 75 | 0 | 5 | 8 | 87 | ||
| TALL104/Dδ3inv | No cRSS | 8 | 42 (∼ 8) | 41 | 0 | 0 | 5 | 95 | ||
| UPN4395/Dδ3 | No cRSS | 3 | 36 (∼ 12) | 36 | 0 | 0 | 6 | 94 | ||
| UPN4395/Dδ3inv | No cRSS | 3 | 45 (∼ 15) | 41 | 0 | 0 | 2.5 | 97.5 | ||
| UPN1589/Dδ3 | No cRSS | 4 | 24 (∼ 6) | 22 | 0 | 0 | 23 | 77 | ||
| UPN1589/Dδ3inv | No cRSS | 4 | 19 (∼ 5) | 19 | 0 | 0 | 16 | 84 | ||
| Vector . | Patient-specific cRSSs* . | No. T† . | No. colonies‡ . | No. A§ . | V(D)J recombination pathway, % . | Break repair pathway, 4, %** . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Heptamer sequence . | Spacer length, bp . | Nonamer sequence . | 1‖ . | 2¶ . | 3# . | |||||
| 647_T068/Dδ3 | CACAGTA | 12 | GCAATAATT | 3 | 193 (∼ 64) | 28 | 78.5 | 0 | 3.5 | 18 |
| T121/Dδ3 | CACAGCA | 12 | ACCAGGGAA | 3 | 60 (∼ 20) | 26 | 31 | 4 | 4 | 61.5 |
| T024/Dδ3 | CACACTA | 12 | ACAGAAATG | 12 | 113 (∼ 9) | 110 | 4.5 | 0 | 11 | 84.5 |
| 6206/Dδ3 | CACATCA | 12 | TCTCCTACT | 14 | 78 (∼ 6) | 76 | 1 | 0 | 22 | 76 |
| 6206/Dδ3inv | CACATCA | 23 | AATTCACCA | 12 | 39 (∼ 3) | 38 | 0 | 0 | 24 | 76 |
| T064/Dδ3inv | CACAGTG | 23 | ACGCTCAAC | 5 | 103 (∼ 21) | 40 | 5 | 10 | 12.5 | 72.5 |
| T064/Dδ3 | CACAGTG | 12 | AAGACAGCC | 3 | 84 (∼ 28) | 27 | 67 | 0 | 11 | 22 |
| TALL104/Dδ3 | No cRSS | 11 | 101 (∼ 9) | 75 | 0 | 5 | 8 | 87 | ||
| TALL104/Dδ3inv | No cRSS | 8 | 42 (∼ 8) | 41 | 0 | 0 | 5 | 95 | ||
| UPN4395/Dδ3 | No cRSS | 3 | 36 (∼ 12) | 36 | 0 | 0 | 6 | 94 | ||
| UPN4395/Dδ3inv | No cRSS | 3 | 45 (∼ 15) | 41 | 0 | 0 | 2.5 | 97.5 | ||
| UPN1589/Dδ3 | No cRSS | 4 | 24 (∼ 6) | 22 | 0 | 0 | 23 | 77 | ||
| UPN1589/Dδ3inv | No cRSS | 4 | 19 (∼ 5) | 19 | 0 | 0 | 16 | 84 | ||
Identified patient-specific cRSSs and the length of their anticipated spacers are indicated; mismatches from the consensus immune RSS (CACAGTG 12/23 ACAAAAACC) are underlined.
Total number of independent transfections.
Total number of clones obtained (average number of colonies per transfection).
Total number of clones analyzed (PCR screen and sequencing).
V(D)J-mediated recombination between authentic Dδ3 RSSs and the cRSSs identified near the patient-specific LMO2 breakpoint.
V(D)J-mediated recombination between authentic Dδ3 RSSs and other cRSSs in the cloned LMO2 area.
V(D)J-mediated recombination between authentic Dδ3 RSSs and other cRSSs in the core vector.
Break repair-mediated recombination (defined as not mediated by V(D)J).
Two types of translocations due to illegitimate V(D)J recombination are recognized: type-1 translocations, in which trans-V(D)J recombination occurs between a TCR/Ig locus and a cRSS-bearing oncogene locus as the result of a RAG-targeting mistake; and type-2 translocations, in which TCR/Ig breakage is RAG induced while the break at the oncogene locus is initiated by other, yet unknown, mechanisms.11,21 Type-1 translocations are so far generally considered to cause t(11;14)(p13;q11).10,11 Although we identified several different functional LMO2 cRSSs that are involved in in vivo type-1 t(11;14)(p13;q11), type-1 translocations thus account for only approximately 65% (9/14) of the current (n = 9) and published (n = 5) t(11;14)(p13;q11) cases.4,,,,–9
To understand whether LMO2 breakpoints at particular cRSSs are directly related to their recombinogenic potential or to a more complex process such as oncogenic selection, we obtained a global view of potent cRSSs within LMO2 using the RIC algorithm.17 We first determined RIC scores of 12-bp cRSS, identified in t(11;14)(p13;q11), and those cRSSs found functional in our ex vivo recombination assay. This revealed a fair correlation (near significant, P = .05, r = 0.698) between ex vivo recombination percentages and RIC scores (Table S1), validating comparison of the 2 approaches, even in the case of low-recombinogenic cRSSs. When using the RIC threshold of authentic Ig/TCR RSS, only the cRSS with the highest ex vivo recombination potential (647/T068) reached a “pass” value. Using this RIC threshold, we identified 8 12-bp and 33 23-bp potent cRSSs, which were randomly scattered throughout LMO2 and appropriately oriented for potential involvement in t(11;14)(p13;q11) (Figure 1A; Table S2). Of these, only 1 was found in t(11;14)(p13;q11) (T068, 6476,7 ) so far. This preferred cRSS exhibited the highest ex vivo recombination potential and has also been found in one t(7;11)(q34;p13) case, involving TCRB and LMO2.8 Interestingly, the second most potent LMO2 cRSS (T121) ex vivo and in silico was also found in a t(7;11)(q34;p13) case,19 whereas all other LMO2 cRSSs, doing poorly in ex vivo/in silico evaluation, were only observed in single t(11;14)(p13;q11) cases so far (this study). Importantly, the preferred cRSS is located directly 3′ of the LMO2 NRE and clusters with other breakpoints 3′ of the NRE (Figure 1A) that contain weak cRSSs. Apparently, as a function of location, these cRSSs with low recombinogenic potential were repetitively more efficient to lead to oncogenic t(11;14)(p13;q11) than cRSSs with higher recombination potential located elsewhere in LMO2. Thus, the involvement of an LMO2 cRSS in t(11;14)(p13;q11) is not solely determined by its recombination potential, but the location within the gene is also a critical determinant for the recurrence/selection of RAG-mediated translocations at specific recombination sites.
The breakpoints in our cases (n = 9) and published cases (n = 5) are scattered throughout LMO2, with TALL-104 showing a novel break in the downstream region. However, clustering of 8 (57%) of 14 breakpoints in a 2565-bp region directly 3′ of the NRE (Figure 1A) suggests a critical role for this region in leukemic selection. Depending on the position of the LMO2 breakpoint and the type of TCRD rearrangement involved, we identified 4 different t(11;14)(p13;q11) derivative chromosomal configurations (Table 2). We observed wide differences in LMO2 expression levels between 7 evaluable cases, correlating with the derivative chromosome configuration (Figure 1B). Breakage 5′ of LMO2 (T064; break region 1), leaving the complete gene plus NRE intact, but excluding the TCRD enhancer, was associated with modest LMO2 expression (∼ 20%). NRE decoupling from LMO2-coding elements (T068, 6206, T024, unique patient number [UPN] 1589; break region 2) was unambiguously associated with high LMO2 expression (∼ 100%-636%), even without juxtaposition of the TCRD enhancer to the LMO2-coding elements. Breakage 3′ of LMO2 (TALL-104), leaving the whole gene intact, while the TCRD enhancer was placed approximately 48-kb downstream of LMO2 was associated with intermediate expression (∼ 50%; Figure 1B). Interestingly however, when the TCRD enhancer was placed approximately 13-kb 5′ of LMO2 (break region 1), there was massive LMO2 expression (UPN4395: ∼ 920%; Figure 1B). Juxtaposition of the TCRD enhancer to LMO2 is thus not necessarily associated with the highest expression, but it can play a very potent role, although this requires the rare and complex Vδ3-Dδ2 inversional recombination, which explains its relative rarity among t(11;14)(p13;q11) translocations (UPN4395).9 More importantly, but contrary to the current dogma, we provide for the first time experimental evidence demonstrating that LMO2 activation in most t(11;14)(p13;q11) translocations is associated with NRE decoupling from LMO2-coding exons rather than juxtaposition of LMO2 to the TCRD enhancer.
t(11;14)(p13;q11) derivative chromosome configuration
| LMO2 break . | LMO2 coding region . | LMO2 NRE . | TCRD enhancer . |
|---|---|---|---|
| Region 1 | der(14) | der(14) | der(11) |
| Region 2 | der(14) | der(11) | der(11) |
| Region 3 | der(11) | der(11) | der(11) |
| Region 1 + TCRD inversion | der(14) | der(14) | der(14) |
| LMO2 break . | LMO2 coding region . | LMO2 NRE . | TCRD enhancer . |
|---|---|---|---|
| Region 1 | der(14) | der(14) | der(11) |
| Region 2 | der(14) | der(11) | der(11) |
| Region 3 | der(11) | der(11) | der(11) |
| Region 1 + TCRD inversion | der(14) | der(14) | der(14) |
LMO2 was expressed in the earliest thymic subsets (CD34+CD38−CD1a− and CD34+CD38+CD1a−), after which it declined to low/undetectable levels (Figure 1C), indicating accessibility for V(D)J recombination at the moment that TCRD recombination occurs during T-cell development.16 Immunophenotypically/genotypically our T-ALL cases represent malignant proliferations of more mature T-cell precursors16,22,23 and consequently overexpress LMO2, suggestive of a role in leukemogenesis.
Interestingly, T-ALL development in LMO2 transgenic mice positively correlates with LMO2 expression levels.24 Most t(11;14)(p13;q11) LMO2 breakpoints mapped so far localize to break region 2 (Figure 1A and Royer-Pokora et al13 ), suggesting a selective advantage for this area. We hypothesize that this is probably due to the uniformly high LMO2 transcript levels associated with breakage in this region. This notion implies that the resultant LMO2 activation level is a critical selective determinant and that not every t(11;14)(p13;q11) confers a selective advantage leading to T-ALL. To examine this, we analyzed healthy thymocytes for the presence of t(11;14)(p13;q11) involving the most frequently found LMO2 cRSS (cRSSa) in T-ALL (T068, 6476,7 ; Figure 1A). As “control” we evaluated the presence of t(11;14)(p13;q11) involving the very potent cRSSb (RIC score = −33.89; Table S2) localized in LMO2 intron 4 (Figure 1A). cRSSb usage would inactivate LMO2 due to disruption of the coding part and as such would not govern any selective advantage. The t(11;14)(p13;q11) translocations involving cRSSa and cRSSb were detected in healthy thymocytes (Figure 1D). Thus different types of t(11;14)(p13;q11) occur in healthy thymocytes, albeit at low frequencies (∼ 10−6). Hence, t(11;14)(p13;q11) as such does not systematically reflect potent LMO2 deregulation, suggesting that not each t(11;14)(p13;q11) will lead to T-ALL.
In summary, we show that illegitimate V(D)J recombination due to RAG mistargeting of several different LMO2 cRSSs accounts for approximately 65% of t(11;14)(p13;q11) translocations in T-ALL, whereas other cases typically occur through type-2 translocations. NRE decoupling from LMO2-coding exons is the main determinant associated with LMO2 activation in the majority of t(11;14)(p13;q11) cases. In addition, our data show that the exact position of the LMO2 breakpoints and the derivative chromosome configuration impact LMO2 activation levels and the consequent pressure for T-ALL development. This study provides important new insights into mechanistic aspects of TCR-associated translocations and subsequent oncogenic activation.
The online version of this manuscript contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank E. F. E. de Haas for help with cell sorting; W. M. Comans-Bitter for preparing figures; and members of the Molecular Immunology Unit, Erasmus MC, for helpful discussions. The pEBB-RAG1 and pEBB-RAG2 expression vectors were kindly provided by C. Roman and S. Cherry.
This work was supported by The Dutch Cancer Society, “Koningin Wilhelmina Fonds” (EMCR 2002-2707; W.A.D., A.W. L., J.J.M.v.D.); the Haak Bastiaanse Kuneman Foundation (A.W.L.); Committee for Scientific Research, Poland (KBN 2 P05A 057 26; G.K.P.); the Alfried Krupp von Bohlen und Halbach Stiftung (G.K.P., C.A.S.); the German José Carreras Leukemia Foundation (G.K.P., P.G., C.A.S.); INSERM (AVENIR2003; B.N., J.M.N.); la Fondation pour la Recherche Médicale (FRM; INE2003114116; B.N., J.M.N.); Association pour la Recherche sur le Cancer (ARC; 7877; B.N., J.M.N.); and Le Conseil Général des Bouches du Rhône (B.N., J.M.N.).
B.N. is a recipient of a Contrat d'Interface INSERM/Assistance Publique-Hôpitaux de Marseille.
Authorship
Contribution: W.A.D., B.N, G.K.P., V.A., P.G., C.A.S., E.A.M., J.J.M.v.D., and A.W.L. contributed to the conception and design of the project, analysis and interpretation of the data, and the drafting of the article. W.A.D., P.G., J.M.N., and B.V. contributed the technical procedures.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Anton W. Langerak, Department of Immunology, Erasmus MC, Dr. Molewaterplein 50, 3015 GE, Rotterdam, The Netherlands; e-mail: a.langerak@erasmusmc.nl.