Abstract
IL-17 and its receptor are founding members of a novel family of inflammatory cytokines. IL-17 plays a pathogenic role in rheumatoid arthritis (RA)–associated bone destruction. However, IL-17 is also an important regulator of host defense through granulopoiesis and neutrophil trafficking. Therefore, the role of IL-17 in pathogen-initiated bone loss was not obvious. The most common form of infection-induced bone destruction occurs in periodontal disease (PD). In addition to causing significant morbidity, PD is a risk factor for atherosclerotic heart disease and chronic obstructive pulmonary disease (COPD). Similar to RA, bone destruction in PD is caused by the immune response. However, neutrophils provide critical antimicrobial defense against periodontal organisms. Since IL-17 is bone destructive in RA but a key regulator of neutrophils, we examined its role in inflammatory bone loss induced by the oral pathogen Porphyromonas gingivalis in IL-17RA–deficient mice. These mice showed enhanced periodontal bone destruction, suggesting a bone-protective role for IL-17, reminiscent of a neutrophil deficiency. Although IL-17RA–deficient neutrophils functioned normally ex vivo, IL-17RA knock-out (IL-17RAKO) mice exhibited reduced serum chemokine levels and concomitantly reduced neutrophil migration to bone. Consistently, CXCR2KO mice were highly susceptible to alveolar bone loss; interestingly, these mice also suggested a role for chemokines in maintaining normal bone homeostasis. These results indicate a nonredundant role for IL-17 in mediating host defense via neutrophil mobilization.
Introduction
The IL-17 cytokine family consists of 6 cytokines (IL-17A to IL-17F) and at least 5 receptors (IL-17RA to IL-17RE; reviewed in Moseley et al1 ). The IL-17 superfamily bears little sequence homology to other cytokine families, and its in vivo functions and molecular biology are poorly understood. Like many inflammatory cytokines, IL-17 plays both protective and pathogenic roles in the immune system. On one hand, IL-17 is important for host defense against infectious organisms, including Klebsiella pneumoniae, Candida albicans, and Toxoplasma gondii.2–4 Conversely, elevated levels of IL-17 are found in autoimmune diseases, including rheumatoid arthritis (RA)/collagen-induced arthritis (CIA), colitis, and multiple sclerosis/experimental autoimmune encephalomyelitis (EAE).5,6 IL-17 was recently shown to be the hallmark cytokine produced by a newly-identified subset of T helper cells, called “Th17,” which are generated following signals from TGFβ, IL-6, and IL-23.7 Although produced primarily by T cells, IL-17 activates many of the same signaling events as innate cytokines such as TNFα and IL-1β, and is thus considered an important bridging molecule between the adaptive and innate immune systems.8,9
IL-17 plays a particularly significant role in regulating neutrophil recruitment and granulopoiesis.10–12 IL-17 up-regulates granulocyte colony-stimulating factor (G-CSF), and overexpression of IL-17 causes neutrophilia in mice.13 In addition, the most strongly induced IL-17 target genes are neutrophil-recruiting chemokines, such as Groα (KC, CXCL1), LIX (CXCL5) and MIP2 (CXCL2).14–17 In K pneumoniae and C albicans infections, where neutrophils are crucial for host defense, an IL-17 receptor deficiency results in reduced chemokine levels and reduced neutrophil numbers in infected tissues.3,4,18 Moreover, IL-17 appears to be part of a feedback loop regulating neutrophil homeostasis.19
Considerable evidence shows that IL-17 impacts bone turnover, particularly in inflammatory arthritis.20 IL-17 is elevated in RA synovial fluid and exerts direct effects on bone cells.6,21 Blocking IL-17 in rodent models of arthritis reduces inflammation and bone damage, whereas excess IL-17 exacerbates disease.22–25 Furthermore, IL-17 knock-out (KO) mice are resistant to CIA, and other mouse models also resistant to CIA show defects in IL-17 production.26,27 Therefore, IL-17 and its receptor are considered attractive therapeutic targets for inflammatory diseases.28
The paradoxical functions of IL-17 raised the question of its role pathogen-induced inflammatory bone loss. Periodontal disease (PD) accounts for most bone disease in humans, and causes tooth loss in 15% of adults.29 Over 75% of the population experiences some form of PD, with significant economic and medical consequences. Not only does PD cause substantial morbidity in its own right, but it is a risk factor for life-threatening conditions such as cardiovascular disease, diabetes, and chronic obstructive pulmonary disease (COPD).30,31 The process of tooth loss is initiated by a subgingival infection that destroys underlying alveolar bone as well as the connective tissue attachment between the gingiva and tooth root. Several Gram-negative bacterial species are associated with periodontal bone loss.32–34 These bacteria initiate but do not directly cause bone destruction in PD. Although periodontal pathogens express a variety of tissue-eroding virulence factors, most damage is actually a result of host response mechanisms.35,36 Neutrophils, however, play a key role in defense against periodontal infection. Indeed, humans with defects in neutrophil adhesion or trafficking are highly susceptible to PD, and frequently lose all their teeth before adulthood.34,35
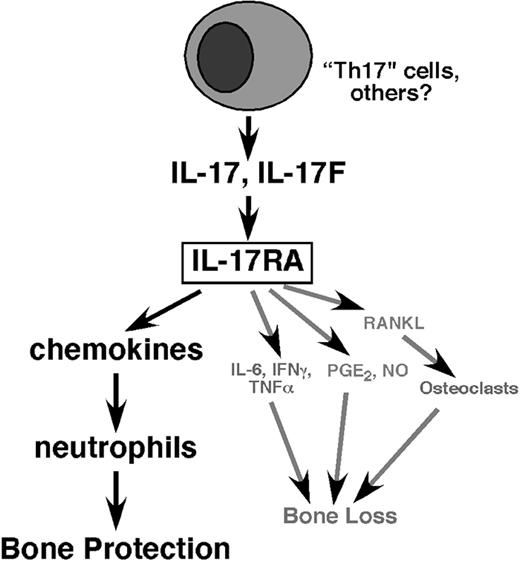
Thus, the role of IL-17 in periodontal disease was not obvious. While IL-17 has been implicated in a few of studies of severe PD,37,38 its role in this disease remains largely undefined. Whereas IL-17 is clearly bone destructive in the context of arthritis, its potent effects on neutrophils suggested that IL-17 could play a defensive role in PD, ultimately exerting a net bone-protective effect (Figure 6). Accordingly, we used IL-17RA–deficient mice to determine the role of IL-17 signaling in a murine model of Porphyromonas gingivalis–induced alveolar (jaw) bone loss. Our results indicate that the overall influence of IL-17 is bone protective in this setting, largely through control of chemokine expression and neutrophil recruitment. Thus, the positive influence of IL-17 on neutrophil regulation outweighs its potential bone-destructive signals, underscoring the importance of IL-17–mediated control of neutrophil mobilization in vivo.
Materials and methods
Mice
IL-17RAKO mice were generously provided by Dr J. Kolls (University of Pittsburgh, PA) with permission from Amgen (Seattle, WA), and CXCR2KO and wild-type (WT) mice (C57BL/6 and BALB/C) were from The Jackson Laboratory (Bar Harbor, ME). Genotypes were confirmed by polymerase chain reaction (PCR). Mice were maintained in HEPA-filtered cages with autoclaved food, water, and bedding. Animals within an experiment were age- and strain-matched females (4-8 mice per group), 6 to 7 weeks old. All procedures were performed in accordance with protocols approved by the University at Buffalo Institutional Animal Care and Use Committee (IACUC).
Bacterial culture
P gingivalis (A7A1-28) was stored in defibrinated sheep blood (Crane Laboratories, Syracuse, NY) at −70°C. Bacteria were maintained by weekly transfer on supplemented blood agar (Brain Heart Infusion Agar [BD Biosciences, San Jose, CA] with 5.0 μg/mL hemin, 5.0 μg/mL menadione [Sigma, St Louis, MO], and 5% defibrinated sheep blood), and grown anaerobically under 5% CO2, 5% H2, and 90% N2 at 37°C.
Oral infections and bone loss assessment
Mice were infected as described.39 Briefly, to reduce oral flora, animals were given sulfamethoxazole trimethoprim in 10 mL/L drinking water (2 mg/mL wt/vol and 0.4 mg/mL wt/vol, respectively) for 10 days, followed by a 5-day wash-out. Infected groups were given 109 CFU Pg suspended in 500 μL PBS with 2% carboxymethylcellulose (CMC; Sigma) via feeding needle 3 times at 2-day intervals. The dosage used was 250 μL placed in the throat and 250μL placed directly in the oral cavity. Control groups were given CMC alone on the same schedule. Forty-two days after the third inoculation, serum was collected by cardiac puncture. Jaws were autoclaved and defleshed, immersed overnight in 3% hydrogen peroxide, and stained with 1% methylene blue in PBS. Horizontal bone loss was assessed morphometrically by measuring the distance between the cementoenamel junction (CEJ) and the alveolar bone crest (ABC). Measurements at 14 buccal sites per mouse (7 sites on the left and right maxillary molars) were made under a dissecting microscope (Brook-Anco, Rochester, NY) fitted with an Aquinto imaging measurement system (a4i America). Random and blinded bone measurements were taken by 2 independent evaluators. All data were analyzed on GraphPad Prism 4 software (GraphPad, San Diego, CA).
For in situ neutrophil recruitment assays, gauze strips soaked in a chemoattractant mixture (100 μg/mL Groα, 100 μg/mL LIX; Peprotech, Rocky Hill, NJ) or saline were adsorbed to the maxillary gingival tissue adjacent to the first molars. To maintain the chemokine gradient, 1 μg of chemoattractant was applied to the gauze every 5 minutes. After 1 hour, gingival tissue was harvested for histology.
ELISA
Pg-specific enzyme-linked immunosorbent assays (ELISAs) were performed as described.39 Briefly, polystyrene plates were coated with formalin-killed Pg. Serial dilutions (2-fold) of test or positive control sera (22 to 212) were incubated for 1 hour at 37°C and washed. Alkaline phosphatase–conjugated goat anti-mouse IgM, IgA, or IgG Abs (Zymed Laboratories, South San Francisco, CA) were used to detect bound Ab, which was quantified by P-nitrophenyl phosphate substrate and absorbance at OD405. Titer was defined as the reciprocal of the highest dilution that produced OD readings more than 0.1 OD unit above background. Total IgG was determined using a mouse IgG quantitation kit (Bethyl Laboratories, Montgomery, TX). Groα and LIX ELISA kits were from R&D Systems (Minneapolis, MN).
Cell culture and neutrophil migration assays
MC3T3-E1 cells were cultured in αMEM (Sigma) supplemented with 10% FBS and 1% penicillin, streptomycin, and L-glutamine (Invitrogen, Carlsbad, CA). To obtain conditioned media (CM), MC3T3-E1 cells were seeded at 1 × 106 cells/mL. Following attachment, cells were washed twice in PBS, incubated in αMEM/0.3% FBS overnight, stimulated with IL-17 (200 ng/mL) for 24 hours; the supernatants were then collected. Bone marrow neutrophils were isolated by magnetic beads using anti–Gr-1 Abs (clone RB6-8C5; BD Pharmingen, San Diego, CA) and a magnetic-activated cell-sorting (MACS) column (Miltenyi Biotec, Auburn, CA). Conditioned supernatants or 100 μM fMLP (Sigma) were added to the lower well of a transwell chamber and approximately 1 × 105 neutrophils were added to the upper chambers. After 15 minutes at 37°C, cells in the lower chamber were counted under 400× magnification in 10 random fields.
Flow cytometry
Bone marrow cells (106) from 8- to 12-week-old female WT or IL-17RAKO mice were stained with 1 μg anti-mouse CXCR2 (clone 242216; R&D Systems) and FITC-conjugated anti-rat IgG2a (clone RG7/1.30; BD Pharmingen) and 0.1 μg anti–Gr-1–PE (clone RB6-8C5; BD Pharmingen). Cells were analyzed using a FACScalibur and CellQuest software (BD Biosciences).
Histology and immunohistochemistry
Maxillary tissue was harvested 24 hours after the first or third infections in 2 mice per group. Tissue was fixed overnight in 10% neutral buffered formalin, decalcified in CalEx II (Fisher Scientific, Pittsburgh, PA) for 72 hours, and dehydrated in 20% ethanol for 1 hour, 50% ethanol for 1 hour, and 70% ethanol for 1 hour. Samples were embedded in paraffin and serially sliced into 0.2-μm sagittal sections, and stained in hematoxylin and eosin by the University at Buffalo Histology Services Core Facility. Sections were analyzed under oil emersion at × 1000 magnification. Positive identification of tissue neutrophils was determined by matching nuclear morphology and cytoplasmic color to previously identified neutrophils in a neighboring capillary, and observations were verified by an oral pathologist. Total neutrophils present in capillaries, gingival epithelium and connective tissue proximal to molars was determined in 40 sequential sections per mouse, excluding sections without teeth. Neutrophils were normalized to the number of teeth in the section.
For immunohistochemistry, Abs were generated against mouse LIX in rabbits by Cocalico Biological (Reamstown, PA) using a synthetic 92-residue peptide corresponding to the full-length LIX.40 The peptide was synthesized at the Microchemical Core Facility of the Norris Comprehensive Cancer Center (University of Southern California, Los Angeles, CA), and purified by high-performance liquid chromatography (HPLC). Peptide composition was verified by mass spectrometry and amino acid analysis. Cross-reactivity to Groα and MIP2 was demonstrated in Western blots (not shown). Archived tissue sections were stained for chemokine-secreting cells using these antisera. Sections were deparaffinized and rehydrated in 3 washes each of xylene, 100% ethanol, 95% ethanol, and ddH2O. They were boiled for 10 minutes in Antigen Unmasking Solution (Vector Labs, Burlingame, CA) and processed with the DAKO LSAB+ kit (DAKO Cytomation, Carpinteria, CA). Slides were counterstained with Mayer hematoxylin, dehydrated in 95% ethanol, 100% ethanol, and xylene, and coverslipped with Vectamount (Vector Labs).
Results
IL-17RAKO mice show enhanced susceptibility to alveolar bone loss following Pg infection
To date, no studies have examined a role for IL-17 or its receptor in bone loss triggered by infection. Since IL-17 is produced by activated T cells and promotes the production of IL-6 and other inflammatory mediators, there were many reasons to think that this cytokine may contribute to bone destruction.37,38,41 However, IL-17 also regulates chemokine expression and neutrophil recruitment (reviewed in Linden and Adachi10 ), which correlates strongly with alveolar (jaw) bone protection in PD.42,43 Therefore, we addressed the role of IL-17 signaling in a widely-accepted PD bone loss model using IL-17R–deficient (IL-17RAKO) mice3 infected with the human periodontal pathogen P gingivalis (Pg). Importantly, IL-17RAKO mice do not exhibit obvious bone defects such as runting or incomplete tooth eruption (data not shown). To determine whether IL-17RAKO mice showed altered resistance to bone loss following Pg infection, IL-17RAKO and age-matched C57BL/6 WT mice were infected orally with Pg suspended in carboxymethylcellulose (CMC). Parallel groups of WT and IL-17RAKO mice were sham-infected with CMC alone. Importantly, infection did not cause significant weight changes or other unexpected side effects (data not shown).
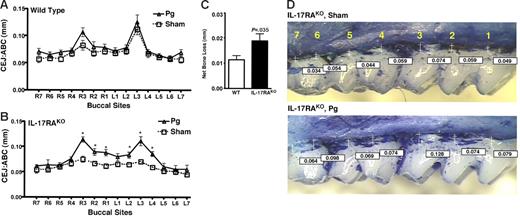
In this model, statistically significant bone destruction levels off at approximately 6 weeks after infection.44 Therefore, alveolar bone loss was assessed after 6 weeks at 14 buccal sites per mouse. Horizontal alveolar bone loss was quantified by measuring the distance between the cementoenamel junction (CEJ) and the alveolar bone crest (ABC) (Figure 1). C57Bl/6 mice are known to be resistant to bone destruction induced by Pg,45,46 so it was not surprising that no significant differences in ABC/CEJ distances were observed between sham-infected and Pg-infected WT animals (Figure 1A). In contrast, IL-17RAKO mice showed significant bone loss at multiple sites (ranging from 29%-57%), particularly in the vicinity of the first molar (Figure 1B-D; sites 1-3). Although the magnitude of alveolar bone loss in this model varies by strain and sex, it is typical to observe a 20% to 50% increase in ABC/CEJ distances,41 and therefore these results indicate considerable bone destruction. Thus, the absence of signaling through IL-17RA predisposes mice to bone loss following periodontal infection.
IL-17RAKO mice exhibit enhanced alveolar bone loss in response to P gingivalis infection. (A-B) WT and IL-17RAKO mice (n = 6-8) were infected with Pg or sham-infected. Alveolar bone destruction was assessed after 6 weeks by measuring the distance from the ABC to the CEJ at 14 maxillary buccal sites per mouse (R1-R7 = right jaw; L1-L7 = left jaw). Standard deviations are shown. Data were analyzed by a Mann-Whitney unpaired t test, and statistically significant differences of Pg-infected compared with sham-infected for each buccal site are indicated with an asterisk (P < .05). (C) Net bone loss averaged over all buccal sites for WT and IL-17RAKO mice, with standard deviations. (D) Representative bone loss measurements from IL-17RAKO sham-infected (C) and Pg-infected (D) maxillary jaws that were stained with methylene blue. Images were acquired with a Nikon SMZ 1000 microscope, magnification ×3. Buccal sites (1-7) are indicated in yellow, and specific ABC/CEJ distance measurements are indicated in boxes.
IL-17RAKO mice exhibit enhanced alveolar bone loss in response to P gingivalis infection. (A-B) WT and IL-17RAKO mice (n = 6-8) were infected with Pg or sham-infected. Alveolar bone destruction was assessed after 6 weeks by measuring the distance from the ABC to the CEJ at 14 maxillary buccal sites per mouse (R1-R7 = right jaw; L1-L7 = left jaw). Standard deviations are shown. Data were analyzed by a Mann-Whitney unpaired t test, and statistically significant differences of Pg-infected compared with sham-infected for each buccal site are indicated with an asterisk (P < .05). (C) Net bone loss averaged over all buccal sites for WT and IL-17RAKO mice, with standard deviations. (D) Representative bone loss measurements from IL-17RAKO sham-infected (C) and Pg-infected (D) maxillary jaws that were stained with methylene blue. Images were acquired with a Nikon SMZ 1000 microscope, magnification ×3. Buccal sites (1-7) are indicated in yellow, and specific ABC/CEJ distance measurements are indicated in boxes.
Infection was confirmed by demonstrating that Pg could be recovered by paper point assay and PCR of Pg 16S ribosomal DNA in both WT and IL-17RAKO mice (data not shown). We examined Pg-specific antibody titers to assess immune responses to the bacteria. Consistent with other studies, Pg-specific IgA was too low to be detected, and no changes in Pg-specific IgM were observed (data not shown).39 However, levels of anti-Pg IgG were strongly enhanced following Pg infection in both WT and IL-17RAKO mice (Figure 2A). While all IgG isotypes were enhanced following Pg infection, only IgG2b was elevated disproportionately in IL-17RAKO mice (data not shown). Interestingly, the baseline levels of IgG were considerably higher in sham-infected IL-17RAKO mice compared with sham-infected WT mice. Since these mice were never exposed to Pg (nor was Pg recovered from sham-infected mice; data not shown), we hypothesized that this result might be due to an elevation in overall levels of IgG in IL-17RAKO mice, causing a higher nonspecific background signal. Indeed, total IgG levels were enhanced 1.6-fold in IL-17RAKO mice compared with WT (Figure 2B). Thus, although baseline IgG levels differed between WT and IL-17RAKO mice, both strains mounted vigorous anti-Pg responses after infection.
IgG titers are elevated in IL-17RAKO mice. (A) Sera from mice described in Figure 1 were analyzed for Pg-specific IgG in WT (□) and IL-17RAKO (▪) mice by ELISA.41 Standard deviations are shown. *Statistically significant differences in Pg-infected samples compared with sham-infected samples of the same strain, as determined by unpaired t test (P < .05). There was no significant difference between WT Pg-infected IgG and IL-17RAKO sham-infected IgG levels. (B) Total IgG levels in uninfected WT (□) and IL-17RAKO (▪) mice were determined in triplicate by ELISA. Standard deviations are shown. *Statistically significant difference compared with WT determined by unpaired t test (P < .05).
IgG titers are elevated in IL-17RAKO mice. (A) Sera from mice described in Figure 1 were analyzed for Pg-specific IgG in WT (□) and IL-17RAKO (▪) mice by ELISA.41 Standard deviations are shown. *Statistically significant differences in Pg-infected samples compared with sham-infected samples of the same strain, as determined by unpaired t test (P < .05). There was no significant difference between WT Pg-infected IgG and IL-17RAKO sham-infected IgG levels. (B) Total IgG levels in uninfected WT (□) and IL-17RAKO (▪) mice were determined in triplicate by ELISA. Standard deviations are shown. *Statistically significant difference compared with WT determined by unpaired t test (P < .05).
IL-17RAKO neutrophils
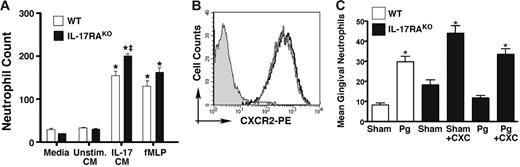
The enhanced susceptibility to bone loss observed in IL-17RAKO mice was reminiscent of findings in other strains with defects in neutrophil recruitment (eg, ICAM-1KO and P/E-selectinKO mice).35,42,43 Since IL-17 has been strongly implicated in neutrophil activity,3,19 we hypothesized that neutrophils in IL-17RAKO mice were functioning abnormally. To determine whether this defect was an intrinsic property of IL-17RAKO neutrophils, we assessed their migratory capacity compared with that of WT. As a source of chemoattractants, we used the bacterial peptide fMLP or conditioned media from a preosteoblast cell line (MC3T3-E1) known to produce high amounts of CXC chemokines (LIX and Groα) in response to IL-17.16 As shown, bone marrow–derived Gr1+ cells (primarily neutrophils) from IL-17RAKO mice showed normal migration to chemotactic stimuli. In addition, surface expression of CXCR2, the major receptor for LIX and Groα, was identical in WT and IL-17RAKO Gr1+ cells (Figure 3B). Similarly, the microbial killing capacity of IL-17RAKO neutrophils in vitro also appeared normal (data not shown). To determine whether the ability of IL-17RAKO neutrophils to migrate in vivo was impaired, we applied LIX and Groα directly to the maxillary molar and monitored neutrophil infiltration by histology. Similar numbers of neutrophils were recruited to the gingiva in WT and IL-17RAKO mice regardless of infection status (Figure 3C), indicating that exogenously provided chemokines are sufficient to rescue the IL-17RA deficiency. Thus, IL-17RAKO neutrophils appear to have no intrinsic functional defects.
Characterization of IL-17RAKO neutrophils. (A) IL-17RAKO neutrophils show no migration defects ex vivo. As a source of chemokines, conditioned media (CM) was obtained from MC3T3-E1 cells stimulated with nothing (Unstim. CM) or 200 ng/mL IL-17 (IL-17 CM; contains > 39 ng/mL LIX; data not shown) for 24 hours (as described16 ). Bone marrow–derived Gr1+ cells from WT (□) or IL-17RAKO mice (▪) were incubated with media alone, with MC3T3-E1 CM, or with the chemotactic peptide fMLP (100 μM). Cells in the lower chambers were quantified in 10 random microscope fields, and standard deviations are shown. *Significant differences compared with unstimulated samples (P < .001); ‡significant difference between WT and IL-17RAKO mice for the same treatment condition (P < .01). (B) Normal CXCR2 levels in IL-17RAKO mice. Bone marrow from WT (black) or IL-17RAKO (gray) mice was stained with Abs to Gr1 and CXCR2. Cells were gated on the Gr1+ population, and the profile of CXCR2 staining is shown compared with the isotype control. (C) Ectopically applied chemokines rescue neutrophil migration to gingiva in IL-17RAKO mice. WT and IL-17RAKO mice were anesthetized, and a mixture of LIX and Groα was applied adjacent to the maxillary first molars for 1 hour. Sagittal sections of maxillary tissue were stained with H&E, and neutrophils were assessed by counting in a randomized, blinded fashion. Standard deviations are shown. *Significant differences compared with sham-infected sample by unpaired t test (P < .05).
Characterization of IL-17RAKO neutrophils. (A) IL-17RAKO neutrophils show no migration defects ex vivo. As a source of chemokines, conditioned media (CM) was obtained from MC3T3-E1 cells stimulated with nothing (Unstim. CM) or 200 ng/mL IL-17 (IL-17 CM; contains > 39 ng/mL LIX; data not shown) for 24 hours (as described16 ). Bone marrow–derived Gr1+ cells from WT (□) or IL-17RAKO mice (▪) were incubated with media alone, with MC3T3-E1 CM, or with the chemotactic peptide fMLP (100 μM). Cells in the lower chambers were quantified in 10 random microscope fields, and standard deviations are shown. *Significant differences compared with unstimulated samples (P < .001); ‡significant difference between WT and IL-17RAKO mice for the same treatment condition (P < .01). (B) Normal CXCR2 levels in IL-17RAKO mice. Bone marrow from WT (black) or IL-17RAKO (gray) mice was stained with Abs to Gr1 and CXCR2. Cells were gated on the Gr1+ population, and the profile of CXCR2 staining is shown compared with the isotype control. (C) Ectopically applied chemokines rescue neutrophil migration to gingiva in IL-17RAKO mice. WT and IL-17RAKO mice were anesthetized, and a mixture of LIX and Groα was applied adjacent to the maxillary first molars for 1 hour. Sagittal sections of maxillary tissue were stained with H&E, and neutrophils were assessed by counting in a randomized, blinded fashion. Standard deviations are shown. *Significant differences compared with sham-infected sample by unpaired t test (P < .05).
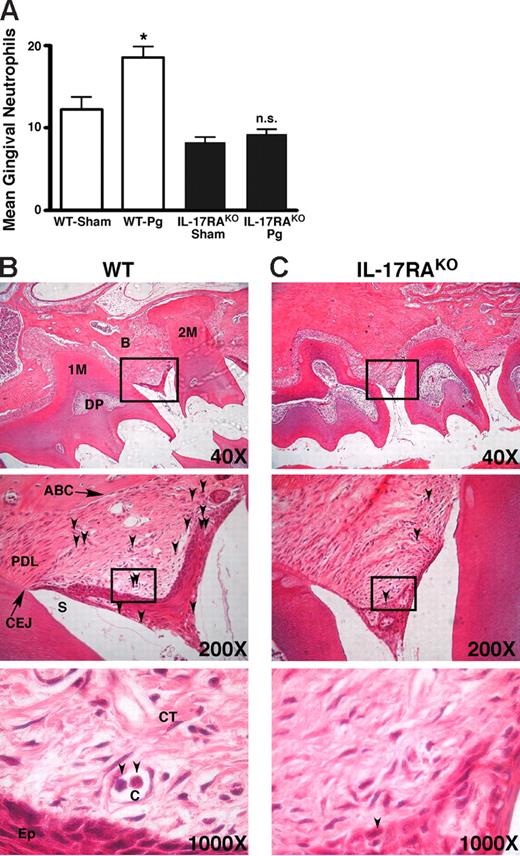
Since neutrophils in IL-17RAKO mice exhibited a normal ability to migrate to exogenous chemokines both ex vivo and in vivo, we next determined whether neutrophils migrated efficiently to the site of Pg infection in IL-17RAKO mice. Despite widespread use of this model, no one to our knowledge has ever directly quantified neutrophil recruitment to mouse gingiva following periodontal infection. To assess kinetics of neutrophil recruitment, IL-17RAKO and age-matched WT mice were sham- or Pg-infected 3 times over 5 days. Mice were killed 24 hours after either the first or third inoculations, and maxillary jaw tissue was harvested and decalcified for histologic analysis. No abnormalities in the morphology of teeth or alveolar bone were observed in IL-17RAKO mice, either in baseline (sham) or Pg-infected conditions (Figure 4B-C; data not shown). To quantify neutrophils in tissue adjacent to the gingival sulcus, we counted hematoxylin and eosin (H&E)–stained polymorphonuclear cells in 60 to 80 serial histologic sections per mouse (2 mice per group). Very little neutrophil recruitment to gingival tissue was observed in WT or IL-17RAKO mice 24 hours after the first infection (data not shown). However, as expected, the number of neutrophils found in situ in Pg-infected WT mice increased significantly relative to sham-treated WT mice 24 hours after the third inoculation (Figure 4A). In these mice, neutrophils could readily be observed in capillaries as well as adjacent connective tissue and epithelium, as would be expected in an inflamed environment. Strikingly, however, the number of neutrophils infiltrating the gingiva in Pg-infected IL-17RAKO mice was not significantly different from sham-treated mice, and few neutrophils were found in connective or epithelial tissue (Figure 4C). Therefore, IL-17RAKO mice mount a markedly reduced neutrophil response at the site of gingival infection.
Defective neutrophil migration to the gingiva in IL-17RAKO mice. IL-17RAKO or WT mice were infected with Pg 3 times over 5 days and killed 24 hours after the final inoculation. Sections were stained with H&E. Images were acquired with a Zeiss Axioimager 2I microscope system. (A) At least 80 slides per condition were examined for neutrophils by oil immersion microscopy at ×1000 magnification, and the number of neutrophils normalized to number of teeth present per slide was determined. Standard deviations are shown. Statistical significance of differences between Pg-infected and sham-infected was assessed by unpaired t test (P < .05). (B-C) Sample slides showing neutrophils in representative Pg-infected WT (panel B) or IL-17RAKO (panel C) gingival slices imaged with 40×/0.10, 200×/0.45, and 1000×/1.30 oil-immersion objective lenses. Arrows indicate polymorphonuclear neutrophils. 1M indicates first molar; 2M, second molar; PDL, periodontal ligament; B, bone; ABC, alveolar bone crest; CEJ, cementoenamel junction; DP, dental pulp; CT, connective tissue; Ep, epithelium; C, capillary; and S, sulcus.
Defective neutrophil migration to the gingiva in IL-17RAKO mice. IL-17RAKO or WT mice were infected with Pg 3 times over 5 days and killed 24 hours after the final inoculation. Sections were stained with H&E. Images were acquired with a Zeiss Axioimager 2I microscope system. (A) At least 80 slides per condition were examined for neutrophils by oil immersion microscopy at ×1000 magnification, and the number of neutrophils normalized to number of teeth present per slide was determined. Standard deviations are shown. Statistical significance of differences between Pg-infected and sham-infected was assessed by unpaired t test (P < .05). (B-C) Sample slides showing neutrophils in representative Pg-infected WT (panel B) or IL-17RAKO (panel C) gingival slices imaged with 40×/0.10, 200×/0.45, and 1000×/1.30 oil-immersion objective lenses. Arrows indicate polymorphonuclear neutrophils. 1M indicates first molar; 2M, second molar; PDL, periodontal ligament; B, bone; ABC, alveolar bone crest; CEJ, cementoenamel junction; DP, dental pulp; CT, connective tissue; Ep, epithelium; C, capillary; and S, sulcus.
Decreased chemokine expression in IL-17RAKO mice
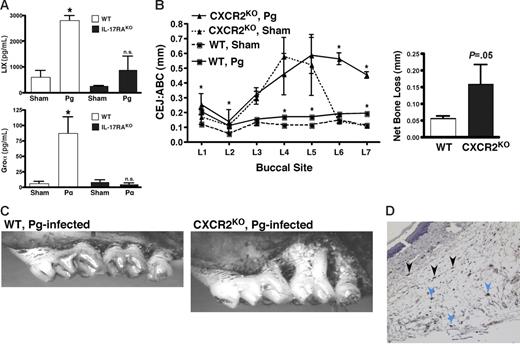
Collectively, these data support a model whereby the enhanced bone loss observed in IL-17RAKO mice is a result of defective neutrophil migration to the site of infection in alveolar bone. Chemokines, particularly those involved in neutrophil recruitment such as LIX and Groα, are strongly induced by IL-17.3,14–17 In samples taken from Pg-infected WT mice at the time of killing, both LIX and Groα concentrations were elevated significantly over that of sham-infected mice. In contrast, these chemokines remained unchanged in Pg-infected IL-17RAKO mice compared with sham-infected controls (Figure 5A). The baseline levels of LIX and Groα in sham-infected WT and sham-infected IL-17RAKO mice were not significantly different. This observation supports the hypothesis that defects in chemokine production in IL-17RAKO mice contribute to the failure of neutrophil recruitment to alveolar bone in IL-17RAKO mice.
CXC chemokine expression in situ. (A) IL-17RAKO mice fail to up-regulate CXC chemokines in response to Pg infection. Serum samples from WT and IL-17RAKO mice in Figure 1 were analyzed for Groα and LIX by ELISA. Standard deviations are shown. *Statistically significant differences between Pg-infected compared with Sham-infected mouse strains as assessed by unpaired t test (LIX, P < .001; Groα, P < .05). n.s. indicate not significant. (B) CXCR2KO mice are susceptible to Pg-induced bone loss. CXCR2KO or WT mice (BALB/c background) were infected with Pg or sham (n = 4-6), and ABC/CEJ distances on the left maxillary jaw were evaluated as in Figure 1. Net bone loss with standard deviations is shown. (C) Representative images of maxillary jaws in Pg-infected WT or CXCR2KO mice, taken as in Figure 1D. (D) Source of CXC chemokines in Pg infection. Sections from Pg-infected WT mice (adjacent sections as in Figure 4B) were stained with antisera that recognizes Groα, LIX, and MIP2. Blue arrows indicate representative monocyte/macrophages; black arrows indicate representative fibroblasts. Image obtained with a 200×/0.45 objective lens. n.s. indicates not significant.
CXC chemokine expression in situ. (A) IL-17RAKO mice fail to up-regulate CXC chemokines in response to Pg infection. Serum samples from WT and IL-17RAKO mice in Figure 1 were analyzed for Groα and LIX by ELISA. Standard deviations are shown. *Statistically significant differences between Pg-infected compared with Sham-infected mouse strains as assessed by unpaired t test (LIX, P < .001; Groα, P < .05). n.s. indicate not significant. (B) CXCR2KO mice are susceptible to Pg-induced bone loss. CXCR2KO or WT mice (BALB/c background) were infected with Pg or sham (n = 4-6), and ABC/CEJ distances on the left maxillary jaw were evaluated as in Figure 1. Net bone loss with standard deviations is shown. (C) Representative images of maxillary jaws in Pg-infected WT or CXCR2KO mice, taken as in Figure 1D. (D) Source of CXC chemokines in Pg infection. Sections from Pg-infected WT mice (adjacent sections as in Figure 4B) were stained with antisera that recognizes Groα, LIX, and MIP2. Blue arrows indicate representative monocyte/macrophages; black arrows indicate representative fibroblasts. Image obtained with a 200×/0.45 objective lens. n.s. indicates not significant.
To further confirm the central role of CXC chemokines in protecting against PD bone destruction, we examined the consequence of a chemokine deficiency using CXCR2KO mice.47 CXCR2 binds the IL-17–induced chemokines Groα, LIX, and MIP2. Neutrophils from these mice exhibit normal killing activity but dramatically impaired migration.47 Interestingly, the alveolar bone in the CXCR2KO mice was very fragile even in an unchallenged state, with extremely large ABC/CEJ distances at most sites and a rough alveolar bone crest (Figure 5B-C). Since the mice were housed in specific pathogen–free (SPF) conditions, this observation may indicate a role for CXCR2 in maintaining normal bone homeostasis, which is consistent with their runted phenotype (data not shown). However, ABC/CEJ distances increased even further following Pg infection, and in some mice resulted in a loss of dentition (data not shown; Figure 5B). Because the CXCR2KO mice are on the BALB/C background, the WT control mice experienced detectable bone loss (Figure 5B), and the susceptible buccal sites of bone loss were somewhat different from the IL-17RAKO mice, which are on the C57BL/6 background (Figure 1 vs Figure 5). However, IL-17RAKO mice backcrossed to BALB/C show a similar increase in Pg-induced alveolar bone destruction (data not shown), indicating that IL-17 contributes to bone loss regardless of genetic background. These data show that a CXC chemokine deficiency shows an even more severe phenotype with respect to oral bone loss than the IL-17RA deficiency, and supports a model whereby chemokines and neutrophils are essential to protect alveolar bone.
The cellular source(s) of chemokines in the setting of PD infection is not known. To determine which cells were expressing neutrophil-attractive chemokines, we performed immunohistochemistry on oral tissue from Pg-infected WT mice, staining with antisera that recognizes the 3 major neutrophil-recruiting CXC chemokines, LIX, Groα, and MIP2. The 2 cell types found to express these chemokines were the fibroblast and monocyte/macrophage populations (Figure 5D). In contrast, no expression was detected in epithelial or endothelial cells, lymphocytes, neutrophils, or other connective tissues. Thus, the major sources of neutrophil-attracting chemokines appear to be monocytes and fibroblasts.
Discussion
The immune system is regulated by myriad multifaceted interactions, and perhaps the most challenging to decipher has been the extraordinarily complex network of functions mediated by cytokines. While studies of cytokines in cultured cells have been enlightening, only studies in vivo reveal their activities in complex immunologic environments. Indeed, studies of cytokines in animal models have frequently yielded unexpected results that have generated important insights into cytokine biology.48
The IL-17 family is particularly fascinating because of its many novel properties.1 Structurally, IL-17 and its receptor bear little resemblance to other well-described cytokine families.49 In culture systems, IL-17 behaves much like classic inflammatory cytokines such as TNFα and IL-1β, triggering up-regulation of the same genes and using similar signaling pathways.14,50 Unlike TNFα and IL-1β, however, IL-17 is produced primarily by T cells, including a subset of effector memory CD4+ cells,51,52 now called “Th17.”7 Therefore, IL-17 appears to be a signal from the adaptive immune system alerting the innate immune system to amplify inflammation and mobilize neutrophils.
Studies in humans and animal models have confirmed that IL-17 plays a pathogenic, bone-destructive role in RA (reviewed in Gaffen25 and Lubberts and Koenders28 ). Many IL-17 target genes impact bone destruction, either through triggering osteoclastogenesis directly or driving up-regulation of genes in osteoblasts that in turn drive osteoclastogenesis (Figure 6; Kotake et al6 and Sato et al20 ). IL-17 also synergizes potently with TNFα and IL-1β, which play bone-destructive roles in RA.53–55 Furthermore, IL-17 is elevated in many autoimmune and inflammatory conditions, including psoriasis, multiple sclerosis, cystic fibrosis, Crohn disease, and Heliobacter pylori infections (reviewed in Cua and Kastelein56 and Gaffen et al57 ). Thus, IL-17 is considered an appealing target for anti-cytokine therapies.28
Opposing roles of IL-17 in inflammatory bone loss. While the dominant influence of IL-17 in RA leads to bone destruction (see Moseley et al,1 Gaffen,25 and Lubberts et al28 ), we find the net effect of IL-17RA–mediated signaling in PD leads to alveolar bone protection. IL-17 is produced primarily by T cells, and triggers a variety of target cells to secrete inflammatory mediators, including chemokines, cytokines, cell-surface receptors, prostaglandin E2, and nitric oxide (NO). While many of these effectors exert bone resorptive effects by mediating enhanced osteoclastogenesis, chemokines and the neutrophils they recruit exert antimicrobial activities that ultimately lead to a bone-protective effect in the context of periodontal infection.
Opposing roles of IL-17 in inflammatory bone loss. While the dominant influence of IL-17 in RA leads to bone destruction (see Moseley et al,1 Gaffen,25 and Lubberts et al28 ), we find the net effect of IL-17RA–mediated signaling in PD leads to alveolar bone protection. IL-17 is produced primarily by T cells, and triggers a variety of target cells to secrete inflammatory mediators, including chemokines, cytokines, cell-surface receptors, prostaglandin E2, and nitric oxide (NO). While many of these effectors exert bone resorptive effects by mediating enhanced osteoclastogenesis, chemokines and the neutrophils they recruit exert antimicrobial activities that ultimately lead to a bone-protective effect in the context of periodontal infection.
By far the most common form of human bone loss occurs in PD.35 PD is a risk factor for atherosclerotic heart disease, COPD, diabetes, increased preterm labor, and low birth weight.30,31 The immune system contributes to bone loss in many disease conditions, and T cells play a particularly key role in periodontal bone erosion.58,59 This is largely due to the ability of T and B cells to up-regulate RANKL, a key maturation factor for bone-erosive osteoclasts.36,60 Consistently, severe combined immunodeficient (SCID) mice and mice deficient in CD4+ T cells are resistant to Pg-induced bone destruction.39,41 Likewise, cytokines derived from T cells and innate cells play important roles in the etiology of PD. IL-1β, in particular, has a strong association with susceptibility to PD,61 probably in part due to its ability to enhance osteoclastogenesis by regulating RANKL expression on osteoblasts. Therefore, T cells and inflammatory cytokines drive alveolar bone destruction and the tooth loss that results.
IL-17 is derived from T cells and clearly has bone-destructive effects in RA. However, we observed that IL-17 signaling through IL-17RA exerts a profound bone-protective effect on PD bone loss. This was not entirely unexpected, since recent work has elucidated a key role for IL-17 in regulating neutrophils in vivo,11 and neutrophils play a well-characterized and essential function in controlling periodontal infection. Humans with inherited disorders in neutrophil chemotaxis have a high frequency of early-onset periodontitis (eg, localized aggressive periodontitis), and genetic polymorphisms affecting chemokine expression have been linked to susceptibility to PD.34 Since neutrophils serve as a first line of defense against infection, the consequence of reduced neutrophil activation is increased bacterial load. Thus, in a sterile inflammatory state such as RA or other autoimmune diseases, IL-17 signaling contributes to tissue damage,62 whereas in bacterial infections such as PD, IL-17 may be critical for recruiting neutrophils and/or other immune cells required to limit the spread of infection. Similar dual roles for other so-called “inflammatory” cytokines have been found in numerous diseases.48
Accordingly, it would be predicted that bacterial load is elevated in IL-17RAKO mice. However, in the PD model used here, it is extremely difficult to quantify accurately the amount of Pg present in gingiva. Although Pg can be recovered from subgingival areas by paper point, recovery is not quantitative or reproducible.63–65 Comparisons to other cultivable flora are sometimes used to normalize Pg levels,66 but this is not an appropriate control in immunocompromised IL-17RAKO mice, which likely have an overall increase in oral microbial burden. Similarly, it is not feasible to normalize Pg to gingival crevicular fluid, as volumes in mice are too small to be measured. Indeed, even in humans, precise quantitation of Pg is considered very challenging, although PCR-based methods have been attempted.67,68 Using PCR to assess levels of Pg 16S ribosomal DNA, we did not find detectable differences in Pg load in WT versus IL-17RAKO mice (data not shown). Thus, we found no evidence to support the hypothesis that bacterial load is increased in IL-17RAKO mice, although the limitations of the available assays still do not rule this out. Therefore, it is quite possible that increases in Pg in IL-17RAKO mice are subtle or nonexistent, and that enhancement of inflammation due to elevated bacterial burden is not the primary explanation for the enhanced bone loss observed here.
Why then, would an imbalance in chemokines and neutrophil migration caused by an IL-17 deficiency lead to enhanced bone loss? Much recent literature has demonstrated a complex relationship between chemokines, neutrophils, and lymphocyte homeostasis,19,69 and that a reciprocal relationship between neutrophils and lymphocytes appears to exist during inflammatory processes.70,71 Therefore, it is plausible that the reduction in chemokines and neutrophils observed in IL-17RAKO mice following infection disrupts the overall balance of immune responses in these mice, leading to enhanced lymphopoiesis, which in turn causes exacerbated bone turnover. Also consistent with this idea is that B-cell homeostasis is dysregulated in CXCR2KO mice.47 It is well established that periodontal bone loss is driven by the immune system,35 which occurs by overexpression of RANKL on activated T and B lymphocytes.36 RANKL is critical for driving development of osteoclasts, a monocyte-derived cell lineage that promotes bone destruction.60 It has been demonstrated in both RA and PD that lymphocyte expression of RANKL is responsible for immune-mediated bone turnover.36,72 Once the inflammation process is initiated by Pg, the immune-dependent bone loss can proceed independently of antigen. Therefore, enhanced bone loss in IL-17RAKO mice may occur not directly because of increased bacterial load, but rather because of dysregulated lymphopoiesis that follows the initial infection.
A few clinical reports suggest a pathogenic role for IL-17 in severe PD.37,38 Human PD is a complex disease state characterized by multiple microbial agents and influenced by a variety of host-dependent factors. The monoinfection system used here is considered to be a model of acute rather than chronic PD, so it is possible that in chronic phases of long-term inflammation, IL-17 may “switch sides” to play a pathogenic rather than protective role.48 Consistent with this, neutrophils are thought to be bone destructive in long-term chronic inflammation, both in RA and PD.62,73,74 Thus, while blockade of IL-17 may be beneficial in autoimmunity, targeting IL-17 may have undesired consequences such as causing increased susceptibility to otherwise mild diseases such as PD.
Our results indicate that the defect in IL-17RAKO mice lies in the ability of neutrophils to reach the gingiva (Figures 3,Figure 4–5). Since neutrophil chemotactic functions and CXCR2 receptor levels are normal in IL-17RAKO mice (Figure 3), the problem lies at least in part in a reduced expression of key neutrophil-attractive chemokines, such as LIX and Groα (Figure 5). Although there may be additional chemokines involved in neutrophil recruitment, LIX is by far the most strongly IL-17-induced chemokine in cultured murine osteoblasts (Figure 5; Ruddy et al16 ). Similarly, LIX is also the predominant chemokine in lungs of Klebsiella-infected mice.75 The cellular source(s) of chemokines within the gingival milieu has never been determined. Cell lines of mesenchymal origin such as fibroblasts and osteoblasts are particularly sensitive to IL-17 and induce high levels of LIX and Groα upon cytokine stimulation,14 but the ubiquitous pattern of IL-17RA expression suggests most cells are potential IL-17 targets.76 Our data show that fibroblastlike cells in the gingival tissue express CXC chemokines following Pg infection, but monocytes/macrophages also appear to be significant producers of chemokines (Figure 3C). Although it is possible that factors in addition to chemokines could contribute to defective neutrophil mobilization in these mice (eg, ICAM-1 and G-CSF, which are regulated by IL-1750 ), ectopic application of CXC chemokines to the gingival area was sufficient to rescue the neutrophil migration defect in IL-17RAKO mice (Figure 3C). Finally, CXCR2KO mice exhibited profound alveolar bone destruction in Pg (Figure 5B-C). Interestingly, the alveolar bone was fragile even in unchallenged CXCR2KO animals, and these mice are quite runted (J.J.Y., unpublished observations, November 2006), indicating that these chemokines or the neutrophils they recruit may play an unexpected role in maintaining healthy bone.
It is striking that a lack of IL-17RA exerts such a profound effect on neutrophil recruitment, since other cytokines still present in these mice also regulate expression of chemokines and other genes involved in neutrophil activation (eg, TNFα and IL-1β). The dominant role of IL-17RA signaling may lie in the fact that IL-17 synergizes potently with other inflammatory cytokines, particularly TNFα and IL-1β.14,55,77,78 Thus, while IL-17RA–mediated signals may appear to be redundant with those of TNFα and IL-1β in vitro, the amplifying effects of IL-17 are essential for an effective immune response in vivo.79
While chemokine expression and neutrophil migration is impaired in IL-17RAKO mice, there may be defects in other arms of the immune system as well. In examining humoral responses, we made the unexpected finding that total levels of IgG are considerably elevated in IL-17RAKO mice (Figure 2). While the mechanistic basis for this difference remains unknown, a similar phenomenon has been observed in other KO mouse strains, and could be due to changes in IgG processing or FcRγ expression.80 This finding differs from observations in IL-17KO mice, where antigen-specific IgG responses are reduced.81 Since IL-17RA also binds IL-17F, another IL-17 family member with more than 50% identity to IL-17,8,82 this might reflect an additional function of IL-17F in humoral responses. Nonetheless, IL-17RAKO mice developed potent anti-Pg antibody responses (Figure 2), suggesting that recall responses are not entirely impaired.
As with many rodent disease models, alveolar bone loss is influenced by genetic background. The IL-17RAKO mice were created on the C57BL/6 strain, which shows a natural resistance to Pg-induced bone destruction.45,66 Studies comparing gene expression in gingiva and spleens of susceptible (Balb/cByJ) versus Pg-resistant (A/J) mice showed that IL-1β, TNFα, and STAT6 were associated with enhanced susceptibility to alveolar bone loss, whereas IL-15, osteoprotogerin, and P-selectin were associated with resistance.46 However, IL-17 expression was too low to be compared in this study, and neither IL-17F nor IL-17RA were examined.
In summary, IL-17 is an intriguing new cytokine with important host defense functions in vivo. Although considerable literature has implicated IL-17 in bone erosion in RA, this cytokine plays a dominantly protective role in bone loss following periodontal infection. These findings have important implications for the use of pharmacologic blockers of IL-17, as well as defining the in vivo biology of this cytokine.
Authorship
Author contributions: J.J.R., M.J.R., G.C.W., and C.S. performed experiments; J.J.R., M.J.R., and S.L.G. designed experiments; P.J.B., R.T.E., and C.S. trained personnel in infection procedures and advised on model; J.B.S. provided key reagents and advice; and S.L.G. wrote the paper with input from M.J.R. and J.J.Y.
Conflict-of-interest statement: The authors declare no competing financial interests.
Correspondence: Sarah L. Gaffen, 36 Foster Hall, 3435 Main St, Buffalo, NY 14214; e-mail: sgaffen@buffalo.edu.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Drs J. Tocker, J. Peschon, S. Levin, K. Kirkwood, A. Teng, R. Genco, E. Hausman, A. Sharma, X. Lin, S. Gollnick, M. Taubman, P. Stashenko, and L. Garrett-Sinha for helpful suggestions and critical comments. IL-17RAKO mice were generously provided by Dr J. Kolls with permission from Amgen. We are especially grateful to Dr M. Neiders for help with histologic analyses and Dr M. Cho for assistance with in situ neutrophil recruitment studies. We thank S. Printup Jacobs and K. Pufpaff for technical assistance.
S.L.G. was supported by National Institutes of Health (NIH) grants AI49329 and AR050458. P.J.B. was supported by NIH grant DE10728. J.J.Y. was supported by a University at Buffalo (UB) Oral Biology training grant DE007034 and the Medical Scientist Training Program at UB. M.J.R. was supported by a training grant to the UB Witebsky Center for Microbial Pathogenesis and Immunology (AI07614). J.B.S. was supported by NIH grant HL57008. R.T.E. was supported by an Oral Immunity grant administered by the Department of Oral Biology at SUNY Buffalo and Therex, LLC (Buffalo, NY).


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal