Abstract
Thirty elderly (> 60 years) Philadelphia chromosome–positive (Ph+) patients with acute lymphoblastic leukemia (ALL) received imatinib, 800 mg daily, associated to steroids without further chemotherapy as frontline treatment. Median age was 69 years (range, 61-83 years). Twenty-nine patients were evaluable for response and all of them obtained a hematologic complete remission, with a median BCR-ABL reduction of 2.9 and 2.0 logs in p190+ and p210+ cases, respectively. Most of the induction treatment did not require admission of the patients. No major toxicities occurred and the treatment was well tolerated. Median survival from diagnosis was 20 months. This study shows that elderly Ph+ patients with ALL—often considered eligible only for palliative treatment strategies—may benefit from an imatinib-steroids protocol, which does not require chemotherapy nor a long hospitalization, is feasible, highly active, and associated with a good quality of life.
Introduction
Philadelphia chromosome–positive (Ph+) acute lymphoblastic leukemia (ALL) occurs in 25% to 30% of adults and in approximately 4% of children with ALL,1–6 and is associated with a very poor prognosis. The reported incidence in the elderly (> 60 years) seems even higher,7 with more unfavorable results and a median survival of less than one year.8,9
In the last few years, studies aimed at testing the activity of different associations of imatinib and chemotherapy as frontline treatment for Ph+ patients with ALL have been carried out, both for younger adults10–13 and for elderly patients.14–16
The question of whether a chemotherapy-free treatment, based only on imatinib plus steroids, could effectively control the disease by inducing durable hematologic and/or molecular responses, is still open. This report summarizes our results on a total of 30 elderly Ph+ patients with ALL who received imatinib plus steroids in induction and imatinib in consolidation until relapse or death.
Patients, materials, and methods
Patients
Patients were treated according to the Gruppo Italiano Malattie Ematologiche dell'Adulto (GIMEMA) LAL0201-B protocol, which had been approved by the internal review board and by the ethics committee of the trial coordinating center, as well as by the local ethics committee of each participating institution. Patients with a diagnosis of ALL who were older than 60 years of age were eligible for this study if they carried either the Ph chromosome or the BCR-ABL molecular translocation. Written informed consent was obtained from each patient in accordance with the Declaration of Helsinki.
BCR-ABL diagnosis and monitoring
All molecular examinations at diagnosis and during the follow-up were performed in the same reference GIMEMA laboratory.17 Total RNA was extracted from bone marrow (BM) cells. cDNA synthesis and reverse transcriptase–polymerase chain reaction (RT-PCR) specific for the BCR-ABL transcripts encoding either the p190Bcr-Abl or the p210Bcr-Abl proteins were performed using the standardized BIOMED-1 protocol.18 Quantitative real-time PCR (Q-RT-PCR) analysis of minimal residual disease was carried out using the methods standardized within a Europe Union concerted action program.19 ABL was used as the control gene and the BCR-ABL values were expressed as a percentage of the ABL transcript levels of ABL.
Study design and therapy
Patients were assigned to receive a 7-day steroid pretreatment (prednisone, at increasing doses from 10 to 40 mg/m2 per day) followed by induction treatment with imatinib at the fixed dose of 800 mg/d, associated to steroids (prednisone by mouth at the dose of 40 mg/m2 per day) from day 1 to day 45. Response evaluation was carried out at day 45. Assessments of BM aspirates, including molecular biology evaluation, were planned after the response evaluation, at the second, fourth, and sixth month from complete remission (CR), and/or at the time of possible relapse.
Dose reduction or discontinuation of imatinib were planned only in case of nonhematologic toxicity. Definitive discontinuation was planned only in case of grade 3 or 4 toxicity occurring more than once. Imatinib was continued in all responding patients until occurrence of disease relapse or excessive toxicity.
Assessment of toxicity and response criteria
Adverse events were graded according to the Common Toxicity Criteria Grading System of the National Cancer Institute (NCI-CTC), version 2.0, April 1999.20 Assessments were carried out and recorded during visits scheduled according to the protocol and/or when unforeseen events occurred.
Complete hematologic remission (CHR) was defined as the disappearance of blast cells from the peripheral blood (PB) and the reduction of BM blasts to fewer than 5%, and a normalization of the PB count. Complete molecular remission (CMR) was defined as the absence of the specific BCR-ABL amplification band detected at diagnosis by qualitative nested RT-PCR and by quantitative RT-PCR negativity (BCR-ABL/ABL copies ratio equal to zero).
Hematologic relapse was defined as the reappearance of the disease with more than 5% blasts in the BM or the reappearance of blasts in the PB or in any other extrahematologic district.
Statistical methods
Time to event analysis was performed using the Kaplan-Meier method. Overall survival (OS) was measured from the date of diagnosis until death from any cause; patients alive were censored at the last follow-up. Disease-free survival (DFS) was measured from the date of CR achievement to the date of hematologic relapse or death in remission, censoring patients alive in CR. Probability of relapse was measured from the date of CR achievement to the date of hematologic relapse, censoring patients dead in remission or alive in CR. All analyses were performed using the SAS v.8.02 software.
Results and discussion
A total of 30 patients with a median age of 69 years (range, 61-83 years) and a diagnosis of BCR-ABL+ ALL confirmed by molecular assessment were enrolled in this study between February 2000 and January 2006. Twenty-nine were considered assessable for response. All 29 (100%) achieved a CHR, whereas a CMR was detected in 1 of the 27 cases evaluable for molecular response. Three additional cases converted to negative nested qualitative PCR status.
At the end of the induction, the patient formally not assessable for response (BM evaluation not performed) showed the disappearance of blasts in the PB and a normalization of the white blood cell and platelet counts, as well as a normal differential count.
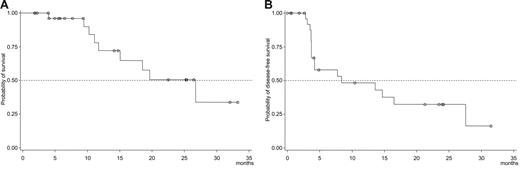
The median survival and the median duration of hematologic response for the 29 patients were 20 months (95% confidence interval [CI]: 12-not reached) and 8 months (95% CI: 4-27), respectively. Fourteen patients relapsed after a median time of 4 months (range, 3-28 months), 2 patients died in CR at 5 and 15 months, whereas 13 patients are alive in continuous remission after a median time of 10 months (range, 1-32 months) from response. The probability of OS and DFS at 12 months is 74% (95% CI: 54-94) and 48% (95% CI: 28-69), respectively (Figure 1A-B).
Median probability of survival. Overall survival (A) and disease-free survival (B) probability in elderly (> 60 years) patients with Ph+ ALL, treated with imatinib plus steroids.
Median probability of survival. Overall survival (A) and disease-free survival (B) probability in elderly (> 60 years) patients with Ph+ ALL, treated with imatinib plus steroids.
During the 45-day induction period, only 7 patients (23%) experienced either a dose reduction or a temporary discontinuation of imatinib due to extrahematologic toxicities. All the grade 3 or higher World Health Organization (WHO) extrahematologic toxicities that occurred during treatment with imatinib are reported in Table 1.
Extrahematologic toxicities (WHO grade > 2)
| Patient no. . | Induction treatment . | Postremission treatment . | ||||||
|---|---|---|---|---|---|---|---|---|
| Toxicity . | WHO grade . | Action taken . | Outcome . | Toxicity . | WHO grade . | Action taken . | Outcome . | |
| 1 | Peripheral nervous system | 3 | TD | Resolved | Peripheral nervous system | 3 | DD | Resolved |
| 2 | Peripheral nervous system | 3 | TD | Resolved | Peripheral nervous system | 3 | DD | Off protocol |
| 3 | None | NA | NA | NA | Nausea/Vomiting | 3 | TD | Resolved |
| 4 | None | NA | NA | NA | Nausea/Vomiting | 3 | TD | Resolved |
| 5 | None | NA | NA | NA | Cutaneous | 3 | DD | Off protocol |
| 6 | Nausea/Vomiting | 3 | TD | Resolved | Gastrointestinal | 3 | DD | Off protocol |
| 7 | None | NA | NA | NA | Cardiac | 3 | DD | Off protocol |
| 8 | Gastrointestinal | 4 | TD | Resolved | None | NA | NA | NA |
| 9 | None | NA | NA | NA | Nausea/Vomiting | 3 | TD | Resolved |
| 10 | Liver toxicity | 3 | TD | Resolved | None | NA | NA | NA |
| 11 | Edema | 3 | TD | Resolved | Cutaneous | 3 | DD | Off protocol |
| 12 | None | NA | NA | NA | Edema | 3 | TD | Resolved |
| 13 | Liver toxicity | 3 | TD | Resolved | None | NA | NA | NA |
| Patient no. . | Induction treatment . | Postremission treatment . | ||||||
|---|---|---|---|---|---|---|---|---|
| Toxicity . | WHO grade . | Action taken . | Outcome . | Toxicity . | WHO grade . | Action taken . | Outcome . | |
| 1 | Peripheral nervous system | 3 | TD | Resolved | Peripheral nervous system | 3 | DD | Resolved |
| 2 | Peripheral nervous system | 3 | TD | Resolved | Peripheral nervous system | 3 | DD | Off protocol |
| 3 | None | NA | NA | NA | Nausea/Vomiting | 3 | TD | Resolved |
| 4 | None | NA | NA | NA | Nausea/Vomiting | 3 | TD | Resolved |
| 5 | None | NA | NA | NA | Cutaneous | 3 | DD | Off protocol |
| 6 | Nausea/Vomiting | 3 | TD | Resolved | Gastrointestinal | 3 | DD | Off protocol |
| 7 | None | NA | NA | NA | Cardiac | 3 | DD | Off protocol |
| 8 | Gastrointestinal | 4 | TD | Resolved | None | NA | NA | NA |
| 9 | None | NA | NA | NA | Nausea/Vomiting | 3 | TD | Resolved |
| 10 | Liver toxicity | 3 | TD | Resolved | None | NA | NA | NA |
| 11 | Edema | 3 | TD | Resolved | Cutaneous | 3 | DD | Off protocol |
| 12 | None | NA | NA | NA | Edema | 3 | TD | Resolved |
| 13 | Liver toxicity | 3 | TD | Resolved | None | NA | NA | NA |
TD indicates temporary discontinuation; DD, definitive discontinuation; NA, not applicable.
In 22 cases, the BCR-ABL levels were re-evaluated at the time of response evaluation. The median reduction of the BCR-ABL/ABL ratio was 2.9 logs (range, 0.93-4.26 logs) for p190+ cases and 2.0 logs (range, 0.28-3.43 logs) for p210+ cases, respectively. In the p190+ cases, the relapse risk at 12 months proved to be more than double when the BCR-ABL reduction was less than 3 logs: 57% (range, 49.1%-66.5%) compared with 20% (range, 13.5%-29.6%) for patients with a reduction greater than or equal to 3 logs. However, this difference did not reach statistical significance.
Two authors have already reported the activity of imatinib in elderly Ph+ ALL.14,21 However, our data suggest that imatinib alone—without chemotherapy—is capable of inducing very positive responses, not only in terms of high HCR rate, but also in terms of prolonged survival probability. Interestingly, in our study OS results were not inferior to what was obtained when postremission chemotherapy was added to imatinib treatment.14
In conclusion, the results of this study support the recommendation that in the presence of a diagnosis of ALL a complete work-up must be rapidly performed, even in elderly patients, in order to swiftly determine if the disease carries the Ph chromosome. Moreover, the impressive CR rate results—close to 100%—obtained without chemotherapy should be taken into account in the planning of future treatment strategies with tyrosin kinase inhibitors for younger adult patients.
Authorship
Contribution: M.V., P.F., L.A., M.B., and F.M. designed and wrote the clinical protocol; G.C. and L.E. performed the centralized molecular analysis for the molecular diagnosis and monitoring of the disease; G. Martinelli, F.D.R., F.F., G. Meloni, A.A., G.Q., L.P., and G.R.-C. performed the research, selecting, enrolling and treating the patients described in the manuscript; R.B. contributed in the organization and managing of the support needed to ensure the availability of the data on the experimental drug and the experimental drug itself; M.V. and P.F. managed the data and analysis, and wrote the manuscript; and G.C. and R.F. analyzed the data and wrote and reviewed the manuscript.
Conflict-of-interest disclosure: R.B. is employed by Novartis Pharma S.p.A., whose product was studied in the present work. The remaining authors declare no competing financial interests.
A complete list of the participating members of GIMEMA appears as Document S1 (available on the Blood website; see the Supplemental Materials link at the top of the online article).
Correspondence: Marco Vignetti, Via Benevento, 6, 00161 Rome, Italy; e-mail: vignetti@bce.uniroma1.it
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
This work was supported by grants from the Gruppo Italiano Malattie EMatologiche dell'Adulto (GIMEMA) Foundation, Rome, Italy, and from the Italian Association against Leukemias, Lymphomas and Myeloma (AIL), Rome, Italy.
Stefania Gubbiotti from the GIMEMA Data Center contributed to the statistical analysis and to the preparation of tables and figures. Sandra De Simone from the GIMEMA Data Center collected and managed all the data from the centers, performing all consistency checks on the database.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal