Abstract
We assessed the combination of sirolimus and tacrolimus without methotrexate after myeloablative allogeneic stem cell transplantation from 53 matched related donors (MRDs) and 30 unrelated donors (URDs). All patients received cyclophosphamide and total body irradiation conditioning followed by transplantation of mobilized peripheral blood stem cells. The median time to neutrophil engraftment was 14 days. The median time to platelet engraftment was 12 days. No differences between MRD and URD cohorts was noted. The incidence of grade II-IV and III-IV acute graft-versus-host disease (GVHD) were 20.5% and 4.8%. The cumulative incidence of chronic GVHD was 59.1%. There were no differences in acute or chronic GVHD incidence between MRD and URD cohorts. The omission of methotrexate was associated with low transplant-related toxicity, with 30-day and 100-day treatment-related mortality rates of 0% and 4.8%. Relapse-free survival at 1 and 2 years was 72.3% and 68.5%, respectively. Overall survival at 1 and 2 years was 77.1% and 72.2%, respectively. There were no differences in relapse-free or overall survival between MRD and URD cohorts. The substitution of sirolimus for methotrexate as GVHD prophylaxis is associated with rapid engraftment, a low incidence of acute GVHD, minimal transplant-related toxicity, and excellent survival. Differences between MRD and URD cohorts are not evident when effective GVHD prophylaxis is used.
Introduction
Acute graft-versus-host disease (GVHD) and transplant-related toxicity are 2 of the most critical barriers to successful allogeneic stem cell transplantation. The combination of a calcineurin-inhibitor and methotrexate has been the standard GVHD prophylactic regimen for the past 20 years,1 but despite these 2 agents, acute GVHD occurs after 35% to 50% of matched, related donor (MRD) transplantation and occurs even more frequently after unrelated donor (URD) transplantation.2 One-year transplantation-related mortality after MRD transplantation ranges from 27% to 37%3 and is higher after URD transplantation. Although some of this mortality is due to acute GVHD, other important factors include infection and organ toxicity. Some of this mortality can be attributed to methotrexate, which delays hematopoietic engraftment,1,4,5 causes epithelial tissue injury, and thus contributes to infection, oral mucositis,6 and organ toxicity.7,8
Sirolimus is the first available inhibitor of the mammalian target of rapamycin (mTOR), a critical regulator of eukaryotic cellular homeostasis.9 Sirolimus binds uniquely to FK-binding protein 12 (FKBP12) and forms a complex with mTOR and the raptor/rictor proteins.10,11 Although there is theoretical competition for FKBP-binding sites between sirolimus and calcineurin inhibitors, these agents appear to work synergistically,12,13 because sirolimus does not interact with calcineurin or its downstream effectors. The sirolimus-FKBP12-mTOR complex inhibits several biochemical pathways, resulting in a reduction in DNA transcription, DNA translation, protein synthesis, and cell cycling, ultimately leading to T-cell immunosuppression. In contrast to the calcineurin inhibitors, sirolimus may also be immunosuppressive via inhibition of dendritic-cell activity through a reduction in antigen uptake,14,15 cellular maturation,16 intracellular signaling,17 and apoptosis induction.18,19 The differential inhibition of certain T-cell subsets (such as CD4+CD25+ regulatory T cells) may also be responsible for some of the immunosuppressive properties of sirolimus.20-22
Sirolimus has been used alone and in combination with calcineurin inhibitors for prevention of allograft rejection after solid organ transplantation23,24 and as therapy for acute25 and chronic GVHD.26,27 The predominant toxicities of sirolimus are mild reversible cytopenias, delayed pulmonary toxicity,28 cutaneous reactions,29,30 and hyperlipidemia with prolonged exposure. It is not associated with the neurotoxicity and nephrotoxicity of calcineurin inhibitors but is associated with a syndrome of thrombotic microangiopathy.31
We have previously demonstrated that the combination of sirolimus, tacrolimus, and low-dose methotrexate is effective GVHD prophylaxis in HLA-matched and HLA-mismatched URD transplantation as well as mismatched related transplantation.32 A preliminary analysis of sirolimus and tacrolimus without methotrexate was demonstrated to be feasible and safe in 30 HLA-matched, MRD transplant recipients.33 In this report, we provide extended follow-up of a large cohort of HLA-matched, related and unrelated patients treated with sirolimus and tacrolimus, without additional methotrexate, and demonstrate that effective GVHD prophylaxis may abrogate differences in matched, related and unrelated donor transplantation.
Patients and methods
Study design
Two trials of sirolimus and tacrolimus as GVHD prophylaxis after allogeneic peripheral blood stem cell transplantation (PBSCT) for hematologic malignancies were performed. HLA-matched, related donors were enrolled between May 2002 and July 2004, and HLA-matched, unrelated donors were enrolled between December 2003 and August 2005. The studies were approved by the Office for the Protection of Research Subjects at the Dana-Farber Cancer Institute and were registered at www.clinicaltrials.gov (NCT00144703, NCT00133367). All participating subjects signed informed consent in accordance with the Declaration of Helsinki. The primary end points of the trials were the incidence and severity of acute GVHD when sirolimus and tacrolimus are used in combination, without methotrexate. Secondary end points included the incidence of serious complications after transplantation (including veno-occlusive disease [VOD], thrombotic microangiopathy [TMA], and interstitial pneumonitis), the time to first hospital discharge, and survival at 100 days and 1 year after transplantation.
Eligible patients had HLA-A, -B, -C, and -DR matched, related and unrelated donors confirmed by polymerase chain reaction (PCR) of sequence-specific primers. Eligibility requirements included age older than 18 years (and younger than 55 years for individuals with unrelated donors), Eastern Cooperative Oncology Group (ECOG) performance status 2 or lower, and adequate measures of renal, hepatic, cardiac, and pulmonary function. For patients with related donors, any hematologic malignancy was eligible. In the URD trial, eligible diagnoses included the acute and chronic leukemias at any stage except untreated blast crisis chronic myelogenous leukemia (CML), the myelodysplastic and myeloproliferative disorders, and treated lymphomas and chronic lymphocytic leukemia (CLL). Burkitt lymphoma was excluded.
Study therapy
For both studies, conditioning prior to transplantation consisted of cyclophosphamide (1800 mg/m2) on 2 consecutive days followed by total body irradiation. A linear accelerator with an energy of 4 MeV was used to deliver a total midline radiation dose of 14.0 Gy in 7 fractions at a dose rate of 10 cGy/min. Lead blocks were used to compensate for lung absorption. Tacrolimus was administered at 0.02 mg/kg/d intravenously by continuous infusion beginning on day −3 with a target serum concentration of 5 to 10 ng/mL. Sirolimus was administered as a 12-mg oral loading dose on day −3, followed by a 4-mg/d single dose, with a target serum concentration of 3 to 12 ng/mL by high-performance liquid chromatography (HPLC). Levels were monitored 3 times weekly during hospitalization and then as clinically indicated. Intravenous tacrolimus was converted to an oral equivalent dose prior to discharge and both immunosuppressives were tapered beginning at day +100 after transplantation and eliminated by week 26 when clinically feasible. No methotrexate was given after transplantation.
Peripheral blood stem cells (PBSCs) were mobilized from related donors after administration of 5 consecutive days of filgrastim (Amgen, Thousand Oaks, CA) at 10 μg/kg/d. PBSCs were mobilized from URDs according to local donor center practices. PBSCs were harvested by large-volume leukapheresis in one to 2 sessions to obtain a target stem-cell dose of 5 × 106 CD34+ cells/kg. The first day of stem cell infusion corresponded to day 0.
All patients were treated in single-patient laminar air-flow rooms and received standard supportive care after transplantation as previously described.32 Filgrastim was administered at 5 μg/kg/d beginning on day +12 when necessary and was continued until neutrophil engraftment. Patients received prophylactic antiviral therapy against herpesvirus infections and prophylaxis against Pneumocystis carinii. No prophylactic antifungal therapy was administered. All patients were monitored for CMV reactivation, without prophylactic therapy. Acute GVHD was graded according to the consensus grading scale.34 Biopsy of involved organs was not required for the diagnosis of acute GVHD.
Statistical analysis
Data for this analysis were sealed on June 30, 2006 and analyzed thereafter. Neutrophil and platelet engraftments were defined as the first of 3 consecutive days of an absolute neutrophil count of 500 cells/μL or an unsupported platelet count of 20 000/μL, respectively. Relapse-free survival (RFS) was defined as the time from transplantation to relapse or death from any cause. Overall survival (OS) was defined as the time from transplantation to death from any cause. Patients alive without a relapse reported were censored at the date of last contact.
Descriptive statistics were used for patient demographics and disease characteristics. The Fisher exact test was used to compare 2 sample proportions, and the Wilcoxon rank sum test was used for 2-sample comparison of continuous variables. RFS and OS were calculated according to the method of Kaplan and Meier.35 The log-rank test was used for comparing OS or RFS between groups. Cumulative incidence curves for acute GVHD and chronic GVHD were constructed reflecting 100-day death or time to relapse (with or without death) as competing risks, respectively. The cumulative incidence for relapse was also computed using nonrelapse death as a competing risk. All analyses were done with the SAS software package (Cary, NC) and all P values are 2-sided.
Results
A total of 53 related donor recipients and 30 unrelated donor recipients are included in this analysis. Their demographic characteristics are shown in Table 1. Two additional patients were enrolled in the MRD trial; one donor failed to mobilize PBSCs and one recipient withdrew consent and did not undergo transplantation. These patients are not included in this analysis. Twenty-nine of 30 URDs were HLA-A, -B, -C, -DR, and -DQ allelic matches, whereas one donor was a single HLA-DQ allelic mismatch.
Baseline characteristics
| . | MRD . | URD . |
|---|---|---|
| Sample size | 53 | 30 |
| Median age, y (range) | 42 (18-59) | 44 (22-54) |
| Sex, no. (%) | ||
| Male | 27 (51) | 13 (43) |
| Female | 26 (49) | 17 (57) |
| Sex mismatch, donor/recipient, no. (%) | ||
| M/M | 11 (21) | 11 (37) |
| F/F | 15 (28) | 7 (23) |
| F/M | 12 (23) | 2 (7) |
| M/F | 15 (28) | 10 (33) |
| Disease | ||
| AML, no. (%) | 15 (28) | 13 (43) |
| CR1, no. | 7 | 6 |
| More than CR1, no. | 8 | 7 |
| CML, no. (%) | 13 (25) | 6 (20) |
| CP, no. | 10 | 5 |
| AP/BC, no. | 3 | 1 |
| NHL/CLL/HD, no. (%) | 14 (26) | 5 (17) |
| MDS, no. (%) | 6 (11) | 4 (13) |
| Myeloproliferative diseases, no. (%) | 3 (6) | 0 |
| ALL, no. (%) | 1 (2) | 2 (7) |
| CR1, no. | 0 | 1 |
| More than CR1, no. | 1 | 1 |
| Plasma-cell dyscrasia, no. (%) | 1 (2) | 0 |
| . | MRD . | URD . |
|---|---|---|
| Sample size | 53 | 30 |
| Median age, y (range) | 42 (18-59) | 44 (22-54) |
| Sex, no. (%) | ||
| Male | 27 (51) | 13 (43) |
| Female | 26 (49) | 17 (57) |
| Sex mismatch, donor/recipient, no. (%) | ||
| M/M | 11 (21) | 11 (37) |
| F/F | 15 (28) | 7 (23) |
| F/M | 12 (23) | 2 (7) |
| M/F | 15 (28) | 10 (33) |
| Disease | ||
| AML, no. (%) | 15 (28) | 13 (43) |
| CR1, no. | 7 | 6 |
| More than CR1, no. | 8 | 7 |
| CML, no. (%) | 13 (25) | 6 (20) |
| CP, no. | 10 | 5 |
| AP/BC, no. | 3 | 1 |
| NHL/CLL/HD, no. (%) | 14 (26) | 5 (17) |
| MDS, no. (%) | 6 (11) | 4 (13) |
| Myeloproliferative diseases, no. (%) | 3 (6) | 0 |
| ALL, no. (%) | 1 (2) | 2 (7) |
| CR1, no. | 0 | 1 |
| More than CR1, no. | 1 | 1 |
| Plasma-cell dyscrasia, no. (%) | 1 (2) | 0 |
M indicates male; F, female; CR1, first complete remission; more than CR1, beyond first complete remission; CP, chronic phase; AP/BC, acute phase/blast crisis; HD, Hodgkin disease; MDS, myelodysplastic syndrome; ALL, acute lymphoblastic leukemia.
Stem-cell product and engraftment
The median number of stem cells infused to matched, related recipients was 7.6 × 106 CD34+ cells/kg (range, 1.6-20.6 cells/kg). Recipients of URD cells received a median of 10.17 × 106 CD34+ cells/kg (range, 3.1-22.1 cells/kg), which was statistically higher than MRD recipients (P < .001).
Engraftment characteristics can be found in Table 2. All patients engrafted neutrophils at a median of 14 days from transplantation (range, 9-17 days). There were no significant differences in the time to engraftment of cells from MRDs and URDs, with MRD recipients engrafting at 14 days (range, 9-17 days) and URD recipients engrafting at 13.5 days (range, 11-14 days, Wilcoxon rank sum P = .2). With this early engraftment of neutrophils, the use of filgrastim after transplantation was minimal. Twelve patients (3 MRD, 9 URD, 14.5% overall) required no filgrastim, and the median number of days of filgrastim use was only 2 (range, 0-13 days).
Engraftment end points
| . | Combined . | MRD . | URD . | P . |
|---|---|---|---|---|
| Neutrophil engraftment, d (range) | 14 (9-17) | 14 (9-17) | 13.5 (11-14) | .2 |
| Platelet engraftment to 20 000/μL, d (range) | 12 (9-47) | 12 (10-47) | 12 (9-25) | .13 |
| Platelet engraftment to 100 000/μL, d (range) | 17.5 (11-189) | 17.5 (11-189) | 17 (12-101) | .32 |
| Time to hospital discharge, d (range) | 19 (14-55) | 19 (15-55) | 19 (14-55) | .95 |
| . | Combined . | MRD . | URD . | P . |
|---|---|---|---|---|
| Neutrophil engraftment, d (range) | 14 (9-17) | 14 (9-17) | 13.5 (11-14) | .2 |
| Platelet engraftment to 20 000/μL, d (range) | 12 (9-47) | 12 (10-47) | 12 (9-25) | .13 |
| Platelet engraftment to 100 000/μL, d (range) | 17.5 (11-189) | 17.5 (11-189) | 17 (12-101) | .32 |
| Time to hospital discharge, d (range) | 19 (14-55) | 19 (15-55) | 19 (14-55) | .95 |
P refers to comparison of MRD and URD groups.
The median time to platelet engraftment to 20 000/μL was 12 days (range, 9-47 days). Again, no statistical difference was noted when MRD patients were compared with URD patients (MRD 12 days, range, 10-47 days; URD 12 days, range, 9-25 days, Wilcoxon rank sum P = .13). The time to attain a platelet count of 100 000/μL was not statistically different either, with a median time in the combined cohort of 17.5 days (range, 11-189 days). In the MRD cohort, this corresponded to 17.5 days (range, 11- 189 days) and in the URD cohort this corresponded to 17 days (range, 12-101 days, Wilcoxon rank sum P = .32). In total, 6 subjects (5 MRD, 1 URD) did not attain a platelet count of 100 000/μL prior to relapse or death.
Eighty-one of 83 patients survived to first hospital discharge, with all 30 URD patients surviving to first hospital discharge. The median time to hospital discharge for MRD patients was 19 days after stem-cell infusion (range, 15-55 days) and the median time to first hospital discharge for URD patients was also 19 days (range, 14-55 days, Wilcoxon rank sum P = .95).
Acute GVHD
In a competing risk model, with death from any cause before 100 days as competing risk, the cumulative incidence of grade II-IV acute GVHD was 20.5%. In the MRD study, the cumulative incidence was 18.9% and the incidence in the URD trial was 23.3%. This difference was not statistically different (P = .68). There were only 3 cases of grade III-IV in the MRD trial and one case in the URD trial. The remaining 13 patients all had grade II disease overall. Two individuals had hepatic involvement, 7 had gastrointestinal involvement, and the remainder had cutaneous disease. The median time to develop grade II-IV acute GVHD was 21 days (range, 7-85 days). The median time for the MRD cohort was 20 days (range, 11-77 days) and that for the URD cohort was 25 days (range, 7-85 days; Figure 1A). There were no cases of primary steroid-resistant acute GVHD.
Cumulative incidences of acute and chronic GVHD. (A) Cumulative incidence of acute GVHD with death as a competing risk. The cumulative incidence of grade II-IV acute GVHD for the combined group was 20.5%: MRD incidence, 18.9%; URD incidence, 23.3% (P = .78). (B) Cumulative incidence of chronic GVHD with death or relapse as a competing risk. The cumulative incidence of chronic GVHD for the combined group was 59.1%: MRD incidence, 58.3%; URD incidence, 59.3% (P = .52). The median time to develop chronic GVHD was 231 days (range, 102-522 days).
Cumulative incidences of acute and chronic GVHD. (A) Cumulative incidence of acute GVHD with death as a competing risk. The cumulative incidence of grade II-IV acute GVHD for the combined group was 20.5%: MRD incidence, 18.9%; URD incidence, 23.3% (P = .78). (B) Cumulative incidence of chronic GVHD with death or relapse as a competing risk. The cumulative incidence of chronic GVHD for the combined group was 59.1%: MRD incidence, 58.3%; URD incidence, 59.3% (P = .52). The median time to develop chronic GVHD was 231 days (range, 102-522 days).
Transplant-related toxicity
Regimen-related toxicity was moderate and is shown in Table 3. Idiopathic pneumonia syndrome/diffuse alveolar hemorrhage occurred in only one individual and was not fatal. A total of 7 subjects developed VOD of the liver of varying severity (8.4%). This was the cause of death in 4 of 7 affected. Two individuals with VOD had been exposed to gemtuzumab ozogamicin prior to transplantation.36 TMA (diagnosed according to standard criteria) was noted in 5 MRD recipients and 1 URD recipient, for a combined incidence of 7.3%. TMA was managed conservatively with dose reduction or discontinuation of tacrolimus. Mycophenolate was substituted in 5 subjects (4 MRD, 1 URD) at the treating physician's discretion, but sirolimus was continued and dosed according to serum level. Renal function recovered in all individuals and TMA did not contribute to the cause of death in any subject. The incidence of TMA was slightly higher in the MRD cohort, but this group was studied first and more aggressive tacrolimus dose adjustments were made in the subsequent URD cohort to prevent this complication.
Transplant-related toxicity
| . | Combined, no. (%) . | MRD, no. (%) . | URD, no. (%) . |
|---|---|---|---|
| VOD of the liver | 7 (8.4) | 5 (9.4) | 2 (6.7) |
| TMA | 6 (7.3) | 5 (9.4) | 1 (3.3) |
| HHV-6 encephalitis | 2 (2.4) | 0 | 2 (6.7) |
| Diffuse alveolar hemorrhage/idiopathic pneumonia syndrome | 1 (1.2) | 1 (1.9) | 0 |
| Invasive fungal infection | 4 (4.8) | 3 (5.7) | 1 (3.3) |
| EBV-associated lymphoproliferative disease | 1 (1.2) | 1 (1.9) | 0 |
| . | Combined, no. (%) . | MRD, no. (%) . | URD, no. (%) . |
|---|---|---|---|
| VOD of the liver | 7 (8.4) | 5 (9.4) | 2 (6.7) |
| TMA | 6 (7.3) | 5 (9.4) | 1 (3.3) |
| HHV-6 encephalitis | 2 (2.4) | 0 | 2 (6.7) |
| Diffuse alveolar hemorrhage/idiopathic pneumonia syndrome | 1 (1.2) | 1 (1.9) | 0 |
| Invasive fungal infection | 4 (4.8) | 3 (5.7) | 1 (3.3) |
| EBV-associated lymphoproliferative disease | 1 (1.2) | 1 (1.9) | 0 |
In all comparisons P was not significant.
Chronic GVHD
In a competing risk model, with relapse with or without death from any cause after 100 days as a competing risk, the cumulative incidence of clinically extensive chronic GVHD or limited chronic GVHD requiring systemic immunosuppression was 59.1%. In the MRD study, the cumulative incidence was 58.3% and the incidence in the URD trial was 59.3%. This difference was not statistically different (P = .52). The median time to develop chronic GVHD was 231 days (range, 102-522 days). The median time for the MRD cohort was 239 days (range, 102-522 days) and that for the URD cohort was 222 days (range, 138-368 days; Figure 1B).
Survival and outcome
The median follow-up of all surviving patients is 33.5 months (range, 14.5-51.7 months) from the time of transplantation. Among the MRD cohort, the median follow-up for surviving patients is 41.9 months (range, 29.6-51.7 months), and among the URD cohort, the median follow-up is 22.2 months (range, 14.5-33 months).
The non–relapse- and relapse-related mortality rate at 30 days was 0% among the 83 patients. Non–relapse-related mortality and relapse-related mortality rates at 100 days were 4.8% and 1.2%, respectively, for a combined mortality rate at 100 days of 6%. Among MRD recipients, these figures were 5.7%, 0%, and 5.7%. Among URD recipients, these figures were 3.3%, 3.3%, and 6.7%.
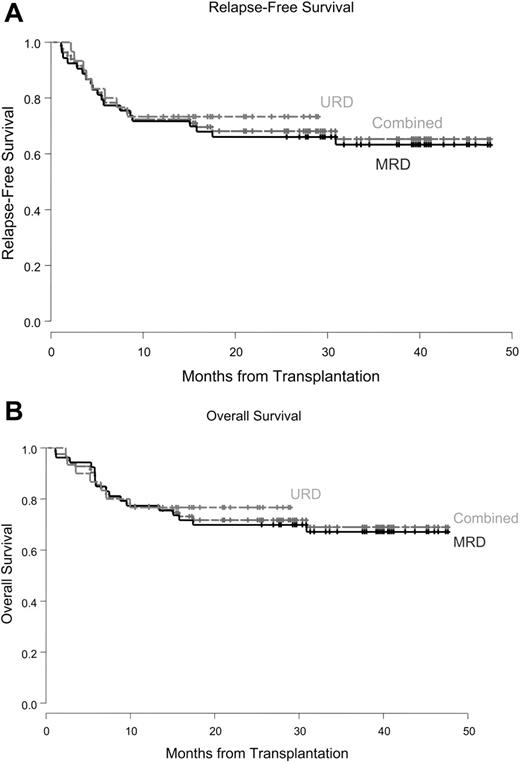
In a competing risk model, with non–relapse-related death as the sole competing risk, the cumulative incidence of relapse was 16.2% (MRD 17%, URD 13.3%, P = .8). RFS for the entire group was 72.3% at 1 year and 68.5% at 2 years. For the MRD group, the corresponding RFS figures were 71.7% and 66.0% at 1 and 2 years, respectively. In the URD group, RFS at 1 and 2 years was 73.3%. To date, there have been no relapses or deaths that have occurred more than 1 year after URD transplantation. The RFS for the MRD and URD cohorts is not statistically different (P = .60; Figure 2A).
RFS and OS. (A) RFS for the combined group was 72.3% at 1 year and 68.5% at 2 years: MRD group, 71.7% and 66.0%; URD group, 73.3% and 73.3% (P = .60). (B) OS for the combined group at 1 year and 2 years was 77.1% and 72.2%: MRD group, 77.4% and 69.8%; URD group, 76.7% and 76.7% (P = .67).
RFS and OS. (A) RFS for the combined group was 72.3% at 1 year and 68.5% at 2 years: MRD group, 71.7% and 66.0%; URD group, 73.3% and 73.3% (P = .60). (B) OS for the combined group at 1 year and 2 years was 77.1% and 72.2%: MRD group, 77.4% and 69.8%; URD group, 76.7% and 76.7% (P = .67).
OS at 1 and 2 years for the entire cohort is 77.1% and 72.2%, respectively. OS rates at 1 and 2 years in the MRD group are 77.4% and 69.8%. In the URD group, OS rates at 1 and 2 years are 76.7%. The MRD and URD cohorts are not statistically different (P = .67; Figure 2B).
Three patients remain alive after disease relapse. All 3 received donor lymphocyte infusions for relapse of HTLV-1–associated adult T-cell leukemia/lymphoma (ATLL), mantle-cell non-Hodgkin lymphoma (NHL), and acute myelogenous leukemia (AML) that occurred at 5.5, 5.9, and 17.5 months after transplantation, respectively. These individuals are currently alive at 36.6, 23.4. and 17.9 months from the time of relapse. Only the individual with mantle-cell NHL has persistent evidence of relapsed disease.
The causes of death among the 24 individuals who died after transplantation are shown in Table 4. Over half of all deaths (54%) are related to relapsed disease, demonstrating the reduced rate of transplantation-related mortality in this cohort.
Causes of death
| . | Combined, no. (%) . | MRD, no. (%) . | URD, no. (%) . |
|---|---|---|---|
| Relapse | 13 (15.7%) | 9 (17.0%) | 4 (13.3%) |
| VOD of the liver | 4 (4.8%) | 2 (3.8%) | 2 (6.7%) |
| Pulmonary complications | 3 (3.6%) | 2 (3.8%) | 1 (3.3%) |
| GVHD | 2 (2.4%) | 2 (3.8%) | 0 |
| Infection | 1 (1.2%) | 1 (1.9%) | 0 |
| Multisystem organ failure | 1 (1.2%) | 1 (1.9%) | 0 |
| . | Combined, no. (%) . | MRD, no. (%) . | URD, no. (%) . |
|---|---|---|---|
| Relapse | 13 (15.7%) | 9 (17.0%) | 4 (13.3%) |
| VOD of the liver | 4 (4.8%) | 2 (3.8%) | 2 (6.7%) |
| Pulmonary complications | 3 (3.6%) | 2 (3.8%) | 1 (3.3%) |
| GVHD | 2 (2.4%) | 2 (3.8%) | 0 |
| Infection | 1 (1.2%) | 1 (1.9%) | 0 |
| Multisystem organ failure | 1 (1.2%) | 1 (1.9%) | 0 |
Discussion
Prevention of transplantation-related morbidity and mortality (TRM) without compromising the rate of acute GVHD remains as one of several critical barriers to the broader acceptance of allogeneic stem cell transplantation for hematologic malignancies. We had hypothesized that the elimination of methotrexate and the use of a more potent immunosuppressive agent, sirolimus, would be able to accomplish both of these goals in the related and unrelated transplantation setting. In this report, we demonstrate low rates of TRM and excellent prevention of acute GVHD after ablative transplantation using the combination of sirolimus and tacrolimus, without methotrexate.
Several methods are currently used to reduce TRM. The most common method is the use of subablative transplantation conditioning. This method, though effective at reducing TRM, is often associated with an increase in the rate of malignant relapse, due to the reduced intensity of the conditioning therapy provided.37,38 Other methods to reduce the rate of TRM include the use of targeted dosing of conditioning agents39 and the use of T-cell depletion.40 The latter approach is also associated with an increased risk of relapse as well due to a loss of T-cell–mediated antitumor activity. In this report, we demonstrate that the use of a GVHD prophylaxis regimen associated with reduced TRM is not associated with an obvious increased rate of relapse; however, this must be evaluated prospectively.
Elimination of methotrexate was associated with rapid reconstitution of hematopoiesis with a short neutropenic period. As a result there were only 2 deaths related to infection and multisystem organ failure in the first 100 days. More importantly, the elimination of methotrexate essentially eliminated the risk of acute pulmonary syndromes such as diffuse alveolar hemorrhage and idiopathic pneumonia syndrome, as previously reported.7,8 The rate of VOD was lower than usually reported, suggesting that methotrexate contributes to tissue injury in this syndrome as well.41 As a result, the 30-day TRM of 0% and 100-day TRM of 4.8% are comparable or superior to many reduced-intensity conditioning trials, and the rate of relapse in this trial was not compromised as may be seen in the reduced-intensity setting.37
Prior attempts to replace methotrexate have had mixed results. In randomized studies where methotrexate was omitted or replaced with corticosteroids, acute1,42-44 and chronic GVHD45,46 rates were higher. When mycophenolate is given in combination with cyclosporine without methotrexate, the time to engraftment has generally been demonstrated to be shortened; however, rates of acute GVHD range between 38% and 62%, which is no different than historical controls.47-50 In our series, the rate of acute GVHD was 20.5% and was not different when MRD and URD cohorts were compared. The rate of chronic GVHD was no different in our series than other published series.
Sirolimus has multiple immunosuppressive properties that may have contributed to the improved GVHD control noted when compared with historical trials of calcineurin inhibitors combined with methotrexate. Sirolimus is known to affect dendritic cells via multiple mechanisms,14-19 and therefore may block the initiating and propagating events of GVHD. In addition, sirolimus specifically inhibits CD8+ T-cell proliferation51 and since CD8+ T cells are important mediators of GVHD,52,53 this may have contributed to the excellent GVHD control noted in both related and unrelated donor cohorts. Other lymphocyte fractions, including regulatory T cells, may be important mediators or modulators of acute GVHD. Regulatory T cells that express the CD4+CD25+ immunophenotype and express high levels of the transcription factor Foxp3 have been shown to generate transplant tolerance in experimental models of transplantation.54 Sirolimus is known to induce Foxp3 expression in a manner different from other immunosuppressive agents, and thus may preferentially maintain regulatory T-cell fractions in comparison with calcineurin inhibitors.20-22
Long-term outcomes reported in this study were comparable or better than other reported series of PBSCT. For example, in a large review of International Bone Marrow Transplant Registry, leukemia-free survival at 1 year after MRD PBSCT varied between 68% and 77%.3 In a randomized trial using MRDs from Seattle, 2-year survival was 66%.55 These results are comparable to our own data, where RFS at 1 year was 72.3% and OS at 2 years was 71.7%. Our results, however, include both related and unrelated donor transplant recipients.
Traditionally, outcomes after unrelated donor transplantation have been inferior when compared with MRD transplantation, with increased rates of both TRM and GVHD contributing to this difference.2 The increase in the rate of GVHD can be explained by the previously unrecognized importance of matching at the extended HLA loci and increased disparity among donor-recipient pairs for minor HLA antigens. The increase in TRM, reflected in increased rates of VOD, acute pulmonary syndromes, and early mortality, is harder to explain, but may be due to a combination of factors, including more advanced disease and stage migration at the time of transplantation, a greater delay to transplantation from the time of malignant diagnosis, and the use of more cytotoxic chemotherapy prior to transplantation. Despite the expected differences, we noted equivalent outcomes for our patients across all major end points studied in this moderate-sized study. There are several possible explanations for this finding. In addition to matching at HLA-A, -B, and -DR, our URD recipients were required to be matched at HLA-C for entry to this study, which may be responsible for some of the improved outcome noted.56 In addition, we excluded patients with refractory leukemia, although patients with untreated relapse underwent transplantation and more than half of the patients with acute leukemia had disease beyond first remission. In the absence of methotrexate, engraftment in this trial was prompt and was not different between MRD and URD cohorts. Historically, engraftment after URD transplantation is thought to be delayed when compared with MRD transplantation, and a reduction in the neutropenic period after transplantation could also account for some of the improvement and comparability between MRD and URD cohorts.
In summary, we have shown that the substitution of methotrexate with sirolimus is a safe and effective regimen for the prevention of acute GVHD in both the MRD and URD setting. This regimen is associated with prompt engraftment, minimal TRM, and excellent GVHD control. At the present, this regimen can be considered an equivalent or potentially superior GVHD prophylaxis regimen for both MRD and URD patients with less transplant-related morbidity than conventional prophylaxis. Moreover, the possibility that the sirolimus and tacrolimus GVHD prophylaxis regimen results in equivalent outcomes in MRD and URD transplantation is encouraging. If these data are confirmed they suggest that recommendations for transplantation can be made independently of donor type, rather than reserving transplantation for patients with MRDs. This regimen will be tested formally in a randomized phase 3 study in the MRD patient population in a trial conducted by the Bone Marrow Transplant Clinical Trials Network.
Authorship
Contribution: C.C. and J.H.A designed the study; C.C, V.T.H., J.K., E.A., R.J.S., and J.H.A. were responsible for patient accrual and care; C.C. and S.L. collected and analyzed the data; C.C. prepared the manuscript; and C.C., S.L., V.T.H., J.K., E.A., R.J.S., and J.H.A. reviewed the manuscript.
Conflict-of-interest disclosure: The authors have no competing financial interests.
Correspondence: Corey Cutler, Dana-Farber Cancer Institute, 44 Binney St, D1B22, Boston, MA 02115; e-mail: corey_cutler@dfci.harvard.edu.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Portions of this work were presented in part at meetings of the American Society of Hematology (December 2004, San Diego, CA; December 2005, Atlanta, GA) and the American Society of Blood and Marrow Transplantation (February 2005, Keystone, CO; February 2006, Honolulu, HI).
Acknowledgment
This work was supported in part by grant P01 HL070149 from the National Heart, Lung, and Blood Institute; an unrestricted educational grant from Astellas, Inc; the Ted and Eileen Pasquarello Research Fund; the Jock and Bunny Adams Education and Research Fund, the DFCI Rising Stars Program, and the Stem Cell Cyclists of the Pan-Mass Challenge.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal