Using primary human vascular endothelial cells grown on a surface coated with a basement membrane extract, Caselli and coworkers found that infection with human herpesvirus 8 (HHV-8, or Kaposi sarcoma–associated herpesvirus) induces the formation of capillary-like tubules that are a hallmark of angiogenesis.
The tubule induction was dependent on monocyte chemoattractant protein 1 (MCP-1), an inflammatory cytokine with angiogenic properties.1,2 MCP-1 induction appeared to be the end point of a tightly channeled, virus-induced NF-κB response (Figure 1). Interest in this observation is heightened because HHV-8 is the etiologic agent of Kaposi sarcoma (KS), a neoplasm that occurs in immune-compromised individuals, elderly men from the Mediterranean region, and in children and adults in some parts of equatorial Africa. KS lesions are defined by a profusion of capillary-like slits that are lined with HHV-8–infected endothelial cells. HHV-8 encodes at least 2 proteins with demonstrated angiogenic properties when studied outside the context of viral infection: a G protein–coupled receptor (vGPCR) that is related to CXCR2,3,4 and a homolog of interleukin 6. Among other things, vGPCR induces NF-κB and MCP-1.5 The paper by Caselli et al is important, in part, because the angiogenic effect occurred in the context of productive viral infection. It will be interesting to see whether the dots can be connected between these experimental biologic systems, and ultimately to pathogenesis in humans.
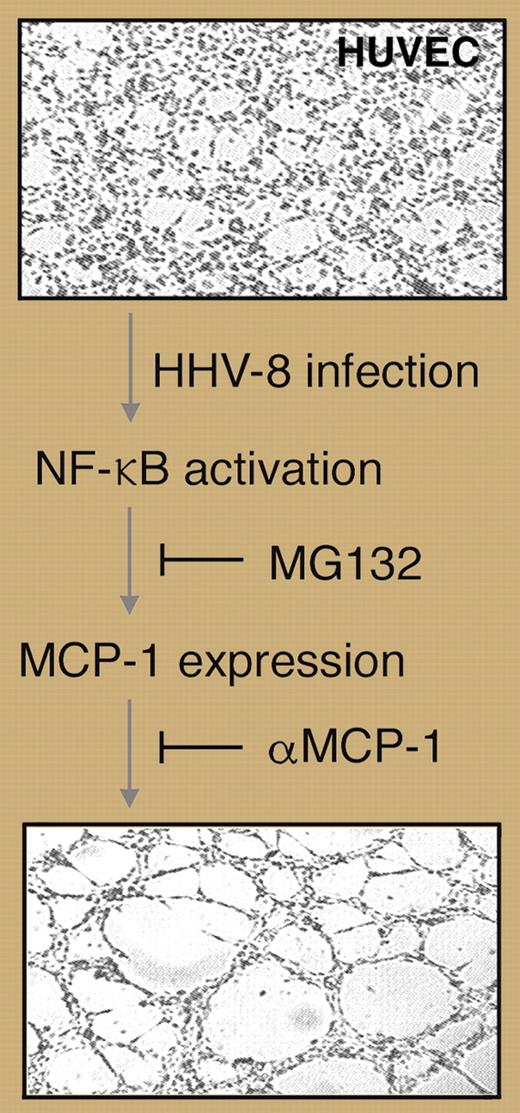
Human umbilical vein endothelial cells (HUVECs) are induced to form capillary-like tubules in response to HHV-8 infection, a process that is dependent on NF-κB–induced MCP-1. Professional illustration by Marie Dauenheimer.
Human umbilical vein endothelial cells (HUVECs) are induced to form capillary-like tubules in response to HHV-8 infection, a process that is dependent on NF-κB–induced MCP-1. Professional illustration by Marie Dauenheimer.
Primary vascular endothelial cells are able to spontaneously form capillary-like tubules, and indeed such tubules formed in the system used by Caselli and coworkers. Not only did HHV-8 infection accelerate this process, but an antibody against MCP-1 inhibited virus-induced tubule formation; the same antibody had no inhibitory effect against the spontaneous process. Thus, angiogenesis is a complex process that has multiple triggers. Because the MCP-1 antibody blocks HHV-8–induced tubule formation but has no substantial effect on spontaneous tube formation, this novel pathway is a potential target for novel KS therapeutics.
NF-κB is a central regulator of a variety of cellular genes that control inflammatory and immune responses, as well as cell proliferation and survival. Although many genes are potentially responsive to NF-κB, only a subset of its target genes is induced under a given set of activating conditions. The requirement of NF-κB for MCP-1 induction in HHV-8–infected cells, in the absence of a broad anti-inflammatory response, emphasizes the specificity with which NF-κB responses can be channeled.
Several items remain for future study. The role of NF-κB needs to be fleshed out, and the other pathways that regulate MCP-1 expression need to be identified. The MCP-1–dependent and –independent pathways for endothelial cell tubule formation need to be defined and their point of convergence identified. Coupling this system with virus genetics will strengthen understanding of the angiogenic mechanism and help dissect the complex process of KS tumor formation: what are the viral factors and how do they work?
The author declares no competing financial interests. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal