Comment on Eltzschig et al, page 1602
Injurious stimuli such as hypoxia and proinflammatory cytokines protect tissues from excessive inflammation by stimulating the induction of adenosine receptors and several of the enzymes that are involved in adenosine production, transport, or degradation.
Eltzschig and colleagues report that hypoxia also results in the induction of adenosine deaminase (ADA) and CD26, a membrane protein that can tether ADA to the surface of human cells, resulting in a diminution of adenosine signaling.
In response to hypoxia, the production of ADA inside endothelial cells (ECs) is increased, and some of the newly formed ADA is exported to the extracellular space by an unknown mechanism where it can bind to newly formed CD26 on the EC surface and convert adenosine to inosine. This discovery adds to our understanding of mechanisms responsible for tightly regulating the local concentration of adenosine and consequently its autocrine and paracrine adenosine receptor-mediated effects that include regulation of vascular tone, platelet function, leukocyte adhesion, endothelial permeability, angiogenesis, and fibrosis.
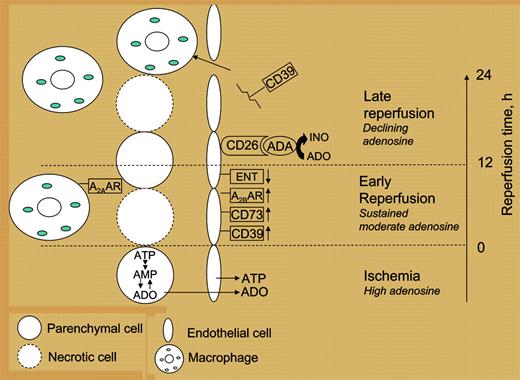
Phases of adenosine signaling that occur during ischemia and reperfusion. Tissue ischemia and hypoxia acutely stimulate the production of adenosine from intracellular sources. ATP that is released from endothelial cells (ECs) in response to shear stress and by other stimuli is converted to ADP/AMP by the ectoenzyme CD39 (NTPDase1). AMP is converted to adenosine (ADO) by CD73, also on the EC surface. ADO limits the extent of acute inflammation by activating anti-inflammatory A2A and A2B receptors on macrophages, neutrophils, lymphocytes, and ECs.1-5Beginning 2 to 4 hours after hypoxia, hypoxia-inducible factor-induced transcription of adenosine A2B receptors, CD39, and CD73 on ECs stimulates enhanced adenosine production and signaling.6Adenosine levels also are increased following hypoxia by transcriptional repression of equilibrative nucleoside transporters (ENTs).7Subsequently, adenosine levels decline in association with accelerated extravasation of activated macrophages that remove necrotic debris. Eltzschig and colleagues show that a late decline in adenosine may occur in part from induction of ADA and CD26. Declining adenosine may also result from the cleavage of CD39 from the EC surface following ischemia-reperfusion injury.8
Phases of adenosine signaling that occur during ischemia and reperfusion. Tissue ischemia and hypoxia acutely stimulate the production of adenosine from intracellular sources. ATP that is released from endothelial cells (ECs) in response to shear stress and by other stimuli is converted to ADP/AMP by the ectoenzyme CD39 (NTPDase1). AMP is converted to adenosine (ADO) by CD73, also on the EC surface. ADO limits the extent of acute inflammation by activating anti-inflammatory A2A and A2B receptors on macrophages, neutrophils, lymphocytes, and ECs.1-5Beginning 2 to 4 hours after hypoxia, hypoxia-inducible factor-induced transcription of adenosine A2B receptors, CD39, and CD73 on ECs stimulates enhanced adenosine production and signaling.6Adenosine levels also are increased following hypoxia by transcriptional repression of equilibrative nucleoside transporters (ENTs).7Subsequently, adenosine levels decline in association with accelerated extravasation of activated macrophages that remove necrotic debris. Eltzschig and colleagues show that a late decline in adenosine may occur in part from induction of ADA and CD26. Declining adenosine may also result from the cleavage of CD39 from the EC surface following ischemia-reperfusion injury.8
Acute tissue hypoxia in response to ischemia-reperfusion injury causes a rapid increase in tissue adenosine production that results in adenosine receptor-mediated signals that increase tissue blood flow and limit acute inflammatory responses (Figure 1). Within several hours after hypoxia there is a transcriptionally induced increase in A2A and A2B receptors and adenosine production that serves to limit the extent of activation of inflammatory cells. The long-term response of tissues to ischemia and reperfusion over 12 to 48 hours includes a late proinflammatory response during which neutrophils and macrophages accumulate to remove necrotic debris, defend injured tissue from invading pathogens, and begin the process of tissue remodeling. Endogenously produced adenosine appears to play a role in orchestrating an appropriate inflammatory response, dictated by the duration of hypoxia and the extent of tissue necrosis, that results in a balance between signals that increase adenosine and inhibit inflammation and signals such as ADA and CD26 that play a role in reducing adenosine and initiating repair. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal