Comment on Rovó et al, page 1100
Irreversible gonadal failure has previously been considered an inevitable consequence of allogeneic stem cell transplantation and an unfortunate but acceptable price to pay for cure of the underlying disease.
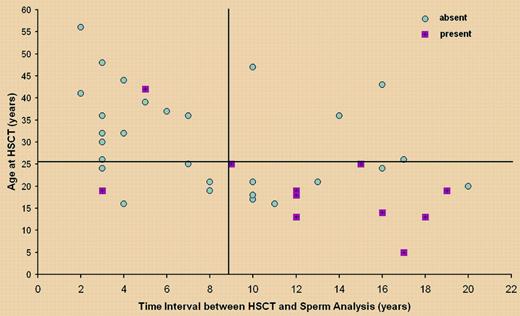
In this issue of Blood, Rovó and colleagues present convincing evidence that our earlier gloomy predictions may have been exaggerated. Thirty-nine male survivors of allografting participated in a snapshot survey of spermatogenesis and 11 (28%) had some degree of recovery. Restoration of spermatogenesis was associated with younger age at transplantation, longer intervals since transplantation, and the absence of chronic graft-versus-host disease (GvHD). Gonadal recovery in men has been reported previously,1-3 but this study is sufficiently large to identify prognostic factors. Younger age at transplantation, a well-recognized prognostic feature for women, has not been considered so important for males. In fact, in this study only one male older than 25 years recovered sperm production, and more than half of those younger than 25 years at transplantation and more than 9 years from grafting recovered. Perhaps the most interesting result is the association of return of spermatogenesis with an absence of chronic GvHD, introducing the possibility of alloimmune-mediated damage of gonadal tissue.FIG1
Presence or absence of spermatozoa after HSCT as a function of age at HSCT and time interval from HSCT. See the complete figure in the article beginning on page 1100.
Presence or absence of spermatozoa after HSCT as a function of age at HSCT and time interval from HSCT. See the complete figure in the article beginning on page 1100.
The study, although most encouraging, still leaves us with some unanswered questions. First, is gonadal recovery impossible in older men? From the figure, it would appear that older men do not generally survive more than 2 years from transplantation. In fact, older patients were less likely to participate in the study, and this is academically regrettable. Older men were more likely to have a family prior to transplantation and perhaps less interested in their personal results. One can speculate about other reasons, including perhaps that their partners were beyond the normal biologic age of conception. Second, how likely is recovery in the prepubertal or peripubertal boy? From this study, it seems that this group has a high chance of recovery with time, but further information regarding their optimal management is required. Third, is the chance of recovery affected by the preparative regimen, particularly pertinent in this time of reduced-intensity conditioning (RICT)? All 3 patients who received transplants using cyclophosphamide as the single agent for severe aplastic anemia (SAA) recovered. However, the 3 recipients of RICT were less than 3 years from transplantation and none showed evidence of recovery. Time will tell. Fourth, what was the effect of prior chemotherapy? Unfortunately, there were no data regarding spermatogenesis immediately prior to transplantation, and so any available information was uninterpretable. Finally, does recovery of spermatogenesis always indicate return of fertility? None of the participants had completely normal spermatogenesis as defined by WHO guidelines and only 3—those who underwent transplantation for SAA, had fathered children since their transplantation.
The demonstration that return of spermatogenesis is possible will give hope to prospective male recipients of a transplant, particularly for their future quality of life. In practice, however, this study also shows 70% of individuals had not recovered and confirms the need for knowledgeable counseling and semencryo preservation prior to treatment. Paradoxically, it also alerts us that counseling regarding birth control will become a mor eregular feature of post-transplantation follow-up! ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal