Haptoglobin (Hp) is a plasma protein synthesized primarily by hepatocytes. It exerts a broad range of anti-inflammatory activities and acts indirectly as a bacteriostatic agent and an antioxidant by virtue of its ability to bind free hemoglobin (Hb) and to facilitate its immediate clearance by macrophages. We identified Hp as a novel specific granule protein of neutrophils by means of immunoelectron microscopy, subcellular fractionation, and exocytosis studies. Consistent with these findings, blood cells from a patient with specific granule deficiency (SGD) lacked neutrophil-derived Hp. Neutrophils contained a large amount of highly glycosylated Hp (β-chain 45-65 kDa) synthesized in neutrophil precursors and stored in specific granules and a small amount of Hp (β-chain 39 kDa) endocytosed from plasma and stored in secretory vesicles. Subsequent binding studies revealed that Hp from specific granules binds to Hb. Finally, the CCAAT enhancer binding protein-epsilon (C/EBPϵ) induced Hp transcription in a myeloid cell line, suggesting that Hp expression in myeloid cells, as in hepatocytes, is at least partially regulated by members of the C/EBP transcription factor family. Collectively, these findings demonstrate that Hp is stored in specific granules and is released by neutrophils in response to activation. Hence, neutrophil-derived Hp might reduce tissue damage and bacterial growth at sites of infection or injury by propagating anti-inflammatory activities and Hb clearance. (Blood. 2006;108:353-361)
Introduction
Infection and tissue injury initiate a local inflammatory response and the subsequent release of proinflammatory cytokines, which in turn mediate a systemic reaction. This so-called acute-phase reaction (APR) is characterized by a marked increase in a common set of plasma proteins known as acute-phase proteins (APPs). APPs are predominantly synthesized in the liver and are essential for reestablishing systemic homeostasis in response to infection. APPs can be subcategorized according to their key functions, such as protease inhibition, support of coagulation and fibrinolysis, modulation of the immune response, and clearance of toxic substances.1-3
Haptoglobin (Hp) is an APP protein whose plasma concentration increases several-fold in response to infection or injury. Hp is synthesized as a single polypeptide chain and is proteolytically cleaved to a short α-chain and a long β-chain that remain connected through a disulfide bond.4 Humans differ from other species by having 2 variants of the HP gene (denoted Hp 1 and Hp 2) caused by partial gene duplication of the α-chain (α1, approximately 10 kDa; α2, approximately 18 kDa). Given that both Hp variants contain a common β-chain (approximately 39 kDa), humans have 3 major phenotypes of Hp, namely Hp 1-1 containing α1-β molecules, Hp 2-2 containing α2-β molecules, and Hp 2-1 containing α1-β and α2-β molecules.5 The Hp 1-1 phenotype represents the basic structure of Hp, which is a dimer of 2 α1-β molecules joined by a single disulfide-bond between the α1-chains. In contrast, the Hp 2-1 and Hp 2-2 phenotypes generate various multimers of α1-β and α2-β molecules because the α2-chains contain 2 cysteine residues (a result of gene duplication) that form disulfide bonds with 2 other α-chains.5
The best understood function of Hp is to bind free hemoglobin (Hb) through the formation of high-affinity complexes.6,7 These Hp-Hb complexes (but not Hp or Hb alone) in turn bind with high specificity to the CD163 scavenger receptor on macrophages, resulting in endocytosis and subsequent intracellular degradation.8,9 Thus, Hp-Hb complex formation is thought to reduce the loss of free Hb through glomerular filtration and to support the recycling of iron.9,10 In addition, the immediate clearance of Hb released from erythrocytes is crucial because free Hb serves as a source of iron, which may otherwise enhance bacterial growth and virulence.11,12 Finally, heme and iron released from free Hb may participate in the generation of reactive oxygen species (Fenton reaction) and may thus promote tissue injury.13,14 The latter has been substantiated in vivo by demonstrating that Hp knockout mice experience severe Hb-mediated tissue injury, particularly in the kidney, compared with wild-type mice.15,16 Hence, Hp functions indirectly as a bacteriostatic agent and an antioxidant by facilitating the immediate clearance of free Hb by macrophages.
A variety of other immunomodulatory effects have been ascribed to Hp. It has been demonstrated that Hp binding to activated neutrophils inhibits calcium influx and subsequent generation of reactive oxygen species.17 In addition, it has been reported that Hp suppresses macrophage functions such as LPS-induced production of tumor necrosis factor alpha (TNF-α), proliferation and cytokine production by T cells, and proliferation of B cells.18-20 Hp has further been shown to bind to cells through CD11b/CD18, CD22, and other yet undefined surface antigens, suggesting that Hp exerts its immunomodulatory effects through receptor-mediated signaling.20-23 Finally, it has been reported that Hp suppresses heat- and oxidative stress-induced misfolding and subsequent precipitation of a variety of proteins. Hence, Hp has a genuine chaperone activity and might thus reduce toxic effects associated with inappropriate aggregation of damaged (misfolded) extracellular proteins.24 Collectively, these findings indicate that Hp contributes to the reestablishment of homeostasis after local or systemic infection by propagating various anti-inflammatory activities.
Polymorphonuclear neutrophilic granulocytes (neutrophils [PMNs]) are key effector cells of innate immunity and of the inflammatory response. Within minutes of injury, neutrophils accumulate at sites of infection and initiate a first line of defense.25-27 Neutrophils exert a broad range of defense mechanisms, including phagocytosis of microorganisms, release of reactive oxygen species to phagosomes, and de novo synthesis of chemokines and cytokines that recruit and modulate the immune response of additional effector cells (neutrophils, monocytes, T cells).25,27,28 Another defense mechanism, unique to neutrophils, is the finely tuned release of prestored antimicrobial and proteolytic proteins to phagosomes and the extracellular environment. Antimicrobial and proteolytic proteins of neutrophils are stored in distinct subsets of cytoplasmic granules, designated azurophil, specific, and gelatinase granules.25,27 A characteristic of granule formation is the sequential emergence of azurophil, specific, and gelatinase granules and their constituent granule proteins during granulocyte differentiation, namely in promyelocytes (PMs), myelocytes/metamyelocytes (MYs), and bone marrow neutrophils (bm-PMNs), respectively. These findings have fostered the targeting-by-timing theory, stating that targeting of granule proteins to a distinct subset of granules is determined by the time of their synthesis. Hence, granule proteins stored in azurophil, specific, and gelatinase granules are readily identified by their unique gene-expression profiles during granulocyte differentiation.29-31 More recently, Wagner et al32 reported that Hp is present, albeit not synthesized, in fully differentiated neutrophils, leading to the hypothesis that neutrophil-derived Hp is endocytosed from plasma.
Here, we provide evidence that neutrophil-derived Hp is primarily synthesized in MYs during granulocyte differentiation, stored in specific granules of fully differentiated neutrophils, and exocytosed immediately in response to activation. These findings implicate that neutrophils release Hp at sites of infection or injury to protect tissue from damage and to reduce bacterial growth during the initial phase of the immune response.
Materials and methods
Isolation of peripheral-blood neutrophils and bone marrow populations
Blood samples, buffy coats, and bone marrow aspirates were obtained from healthy donors and a child with confirmed specific granule deficiency (SGD) after informed consent had been given, in accordance with the local ethics committees of the cities of Copenhagen, Frederiksberg, and Manchester.33 Peripheral-blood neutrophils (pb-PMNs) were isolated from blood samples or buffy coats by density centrifugation and subsequent hypotonic lysis of erythrocytes, as described previously.34 Populations highly enriched in promyelocytes (PMs), myelocytes/metamyelocytes (MYs), and bone marrow neutrophils (bm-PMNs) were isolated from BM aspirates by 2-layer density centrifugation and subsequent immunomagnetic depletion of nongranulocytic cells, as described previously.31,35 All steps of immunomagnetic sorting were performed immediately after cell collection at 4°C or less with the use of nonpyrogenic reagents and plasticware to minimize cellular activation.
Cytospins were prepared by centrifugation of 1 to 2 × 105 isolated cells onto glass slides (300 rpm, 10 minutes, room temperature [RT]; centrifuge used was a Shandon Cytocentrifuge [Thermo Electron, Waltham, MA]). The purity of isolated BM and neutrophil populations was assessed by microscopy of Wright-Giemsa-stained cytospins. Cell numbers were assessed with an improved Neubauer hemocytometer.
Immunocytochemistry
Cytospins of purified BM and neutrophil populations were fixed in TBS (50 mM Tris, 150 mM NaCl, pH 7.6)/4% formaldehyde (37% stock; Sigma, St Louis, MO) at RT for 20 minutes, washed in TBS, and permeabilized in TBS/1% Triton X-100 (Sigma) at RT for 30 minutes. Cytospins were then washed in TBS/1% BSA, and nonspecific binding was blocked by incubation in TBS/1% BSA (Sigma) at RT for 30 minutes. Then cytospins were probed at RT for 30 minutes with the following primary antibodies diluted in TBS/0.25% BSA: rabbit anti-human haptoglobin (1:1000; A 0030; DakoCytomation, Glostrup, Denmark), rabbit anti-human lactoferrin (1:1000; gift from DakoCytomation), and control rabbit IgG (1:500; X 0936; DakoCytomation). Cytospins were washed twice in TBS, incubated at RT for 30 minutes with alkaline phosphatase-conjugated anti-rabbit/mouse polymer, washed twice in TBS, and stained with Fast-Red as recommended by the manufacturer (Dual Envision System-AP; DakoCytomation). Finally, cytospins were washed in running tap water for 10 minutes, counterstained for 1 minute in Mayer hematoxylin, washed again in running tap water for 3 minutes, and mounted. Cytospins were examined under a BX51 microscope equipped with a DP70 photosystem with analy SIS 5.0 software (Olympus, Hamburg, Germany) and a 40×/0.85 numeric aperture oil objective. PowerPoint software (Microsoft, Redmond, WA) was used to prepare the images.
Exocytosis studies
Neutrophils were isolated from freshly collected blood samples or buffy coats and resuspended at a density of 3 × 107 cells/mL in Krebs-Ringer phosphate buffer with glucose (KRG; 130 mM NaCl, 5 mM KCl, 1.27 mM MgSO4, 0.95 mM CaCl2,10mMNaH2PO4/Na2HPO4, 5 mM glucose, pH 7.4). To stimulate exocytosis of granule proteins by neutrophils, 1 mL cell suspension was preincubated for 5 minutes at 37°C and subsequently stimulated for 15 or 30 minutes at 37°C by the addition of the following agents: ionomycin (1 μM; Calbiochem, La Jolla, CA), phorbol-12-myristate 13-acetate (PMA; 2.5 μg/mL; Sigma), formyl-Met-Leu-Phe (fMLP; 100 nM; Sigma), TNF-α (50 ng/mL; Sigma), and 10% autologous serum-opsonized Escherichia coli (multiplicity of infection, 10 bacteria/cell). Opsonized E coli bacteria (XL-1 Blue; Stratagene, La Jolla, CA) were prepared using fresh autologous serum essentially as described previously.36 Control cells were incubated on ice for 20 or 35 minutes. Stimulation was stopped with the addition of 1 mL ice-cold KRG to cell suspensions. Cells were immediately pelleted, and the cell pellets and supernatants containing exocytosed granule were subjected to enzyme-linked immunosorbent assay (ELISA), as described previously, or were resuspended in 2 × Laemmli buffer for subsequent Western blot analysis.37
Immunoelectron microscopy
Isolated blood neutrophils were fixed for 24 hours in 0.1 M PHEM buffer (240 mM PIPES, 100 mM HEPES, 8 mM MgCl2, 40 mM EGTA, pH 6.9) containing 4% paraformaldehyde, as described previously.38 Ultrathin cryosections of neutrophils were prepared and incubated at RT with the primary antibodies rabbit anti-human haptoglobin (DakoCytomation) and rabbit anti-human lactoferrin (Cappel Laboratories, Cochranville, PA) and 10 nm or 15 nm protein A gold, as described previously.38 Controls were labeled with irrelevant rabbit antiserum. After immunolabeling, the cryosections were embedded in a mixture of methylcellulose and uranyl acetate and were examined through an electron microscope (CM 10; Philips, Eindhoven, The Netherlands).
Subcellular fractionation
Neutrophils isolated from buffy coats were incubated in saline/5 mM diisopropylfluorophosphate (DFP; Aldrich Chemical, Milwaukee, WI) for 5 minutes, pelleted (200g, 6 minutes, 4°C), and resuspended at 3 × 107 cells/mL in disruption buffer (100 mM KCl, 3 mM NaCl, 1 mM Na2 ATP, 3.5 mM MgCl2, 10 mM PIPES, pH 7.2) containing 0.5 mM phenylmethylsulfonyl fluoride (PMSF; Sigma). Cells were disrupted by nitrogen cavitation at 600 psi.39 Nuclei and intact cells were pelleted (400g, 15 minutes). Postnuclear supernatant (S1;10 μL) was carefully applied on top of a Percoll gradient including 3 layers of 9 mL Percoll with densities of 1.05, 1.09, and 1.12 g/mL. Gradients were generated by adding precalculated amounts of Percoll (range, 1.129-1.131 g/mL; Amersham Bioscience AB, Uppsala, Sweden) to disruption buffer/0.5 mM PMSF (Sigma) to obtain densities of 1.05, 1.09, and 1.12 g/mL.39 The 3-layer gradient topped by the postnuclear supernatant (S1) was centrifuged at 37 000g for 30 minutes for subcellular fractionation. This resulted in 4 major bands—the α-band enriched in azurophil granules, the β1-band enriched in specific granules, the β2-band enriched in gelatinase granules, and the γ-band enriched in cell membranes and secretory vesicles containing plasma proteins. Fractions of 1 mL were aspirated from the bottom of the 3-layer gradient, and 450 μL from each fraction was centrifuged for 20 minutes at 28 psi in an airfuge (Beckman, Palo Alto, CA) to sediment the Percoll. The supernatant containing the cellular material was resuspended in phosphatebuffered saline (PBS) and subjected to ELISA, as described previously, or was mixed with an equal volume of 2 × Laemmli buffer for subsequent Western blot analysis.37
N-glycosidase F treatment
Pooled subcellular β-fractions containing Hp from specific granules (20 μL) and purified plasma Hp (10 μL; Sigma) were deglycosylated by peptide N-glycosidase F (PNGase-F) treatment for 3 hours at 37°C in accordance with the manufacturer's instructions (New England Biolabs, Beverly, MA). After deglycosylation, samples were mixed with equal volumes of 2 × Laemmli buffer for Western blot analysis.
Hp-Hb affinity precipitation
Human HbA0 (Sigma) was coupled to CNBr-activated Sepharose 4B beads according to the manufacturer's instructions (Amersham Biosciences). HbA0 Sepharose beads and control Sepharose beads were washed twice in PBS (pH 7.8) and incubated with pooled subcellular β-fractions resuspended in PBS overnight at 4°C. After incubation, samples were washed 6 × in PBS (2800g, 2 minutes, RT), and Hp was eluted in SDS containing sample buffer (0.02 M Tris, pH 6.8, 5% SDS, 17.4% glycerol) for subsequent Western blot analysis.
Surface plasmon resonance analysis
Binding studies of neutrophil-derived Hp to Hb were performed by surface plasmon resonance (SPR) analysis. To obtain neutrophil-derived Hp contained in specific granules, subcellular β-fractions were prepared from pooled buffy coats (including Hp phenotypes 1-1, 2-1, 2-2), and Hp was highly enriched by affinity chromatography with a column containing 5 mg rabbit anti-human haptoglobin (DakoCytomation) immobilized on 4 mL CNBr-activated Sepharose beads (Amersham Bioscience).
SPR analysis was performed essentially as described previously with a BIAcore 3000 instrument (BIAcore AB, Uppsala, Sweden) and BIAcore CM5 sensor chips containing immobilized human HbA0 (Sigma) corresponding to 67 to 83 fmol/mm2 protein.8,40 Sensograms were generated using samples of purified neutrophil-derived Hp and plasma Hp (Sigma). Binding data were analyzed using the BIAmolecular analysis evaluation program (version 3.1; BIAcore AB).40
Western blot analysis
Samples were diluted with an equal volume of 2 × Laemmli buffer and were denatured at 100°C for 10 minutes.41 Samples were then electrophoresed on 10% and 12% SDS polyacrylamide gels (BDH Laboratory Supplies, Poole, United Kingdom) or 4% to 16% gradient SDS polyacrylamide gels and were transferred to nitrocellulose membranes (Amersham Bioscience) by electroblotting. Membranes were then incubated as indicated with primary rabbit anti-human haptoglobin (1:1000; DakoCytomation), myeloperoxidase (MPO; 1:1000, A0398; DakoCytomation), and lactoferrin (1:10 000; gift from DakoCytomation) followed by a secondary horseradish peroxidase-conjugated swine antirabbit antibody (1:1000, P0217; DakoCytomation) or an alkaline phosphatase-conjugated goat antirabbit antibody (1:1000, D0487; DakoCytomation). Binding of antibodies was visualized by enhanced chemiluminescence (ECL; Amersham Bioscience) or a mixture of nitroblue tetrazolium (NBT) and 5-bromo-4-chloro-3-indolyl-1-phosphate (BCIP; Promega, Madison, WI).
32Dcl3 cells
The murine 32Dcl3 cell line, generated from diploid myeloid progenitors, proliferates in the presence of IL-3 and can differentiate into mature neutrophils within 10 to 12 days in response to granulocyte-colony-stimulating factor (G-CSF) stimulation.42 32Dcl3 cells were transduced with a retroviral vector constitutively expressing the C/EBPϵ-ER fusion protein, which is maintained in the cytoplasm and only translocates to the nucleus to exert C/EBPϵ activity in the presence of the estrogen derivative 4-hydroxy-tamoxifen (4-HT).
32Dcl3 cells were maintained in Iscove modified Dulbecco medium (IMDM; Invitrogen, San Diego, CA) containing 10% heat-inactivated calf serum, 1 ng/mL murine IL-3 (StemCell Technologies, Vancouver, BC, Canada), and 100 U/mL penicillin combined with 100 μg/mL streptomycin (Invitrogen).
The C/EBPϵ-ER cDNA construct was prepared by linking the full-length human C/EBPϵ cDNA in-frame to a modified tamoxifen-responsive estrogen receptor hormone-binding domain (murine ER; amino acids 281-599).43 The C/EBPϵ-ER and ER cDNA were inserted into the polylinker of the pBabePuro retroviral vector (Nolan Laboratory home page: http://www.stanford.edu/group/nolan/index.html). The pBabePuro-C/EBPϵ-ER vector and the pBabePuro-ER control vector were transfected into the ecotropic packaging cell line Phoenix NX by calcium-phosphate precipitation. After 24 hours, 32Dcl3 cells were cocultured with transfected Phoenix cells for another 48 hours in 32Dcl3 medium plus 4 μg/mL polybrene Sigma. Subsequently, 32Dcl3 cells were selected in puromycin (2 μg/mL), and subclones were generated by transfer of single cells into 96-well dishes using an automated Quickcell transfer device (Stoelting, Wood Dale, IL).34
To define whether C/EBPϵ can transactivate Hp expression in myeloid progenitors, C/EBPϵ activity was induced in 32Dcl3-C/EBPϵ-ER cells by the addition of 200 nM 4-HT (Sigma) to the medium. 32Dcl3-ER cells induced by 4-HT served as control. Total RNA was isolated from cells using TRIzol (Invitrogen) before and after 4-HT induction at indicated time points. Subsequently, Hp expression was assayed by real-time RT-PCR.
Real-time RT-PCR
Expression of Hp transcripts in 32Dcl3-C/EBPϵ-ER and 32Dcl3-ER cells were assessed as described previously.44 Briefly, first-strand cDNA was generated by reverse transcription of 5 μg total RNA at 42°C for 1 hour with the use of a T7-oligo(dT)24 primer and Superscript II, as described by the manufacturer (Invitrogen). First-strand cDNA was then subjected to real-time PCR using the following primers and probes: β-actin forward primer, GAA GTC CCT CAC CCT CCC A; β-actin reverse primer, GGC ATG GAC GCG ACC A; β-actin probe, AAG CCA CCC CCA CTC CTA AGA GGA GG; Hp forward primer, TTC AGG GCT CAC TAG AAG GCT G; Hp reverse primer, TTC CCC CTC TTC CAT GGC; Hp probe, ACA TGG CAG GGC AGG CTG GG. The constitutively expressed housekeeping gene β-actin was used to normalize Hp expression.
Results
Hp is synthesized during granulocyte differentiation
The hallmark of granulocyte differentiation is the sequential formation of azurophil, specific, and gelatinase granules and their constituent granule proteins. Accordingly, granule proteins are readily identified by their unique gene-expression profiles during granulocyte differentiation.29-31 We recently characterized the transcriptional program of terminal granulocyte differentiation by comprehensive microarray analysis of populations highly enriched in promyelocytes (PMs), myelocytes/metamyelocytes (MYs), bone marrow neutrophils (bm-PMNs), and peripheral-blood neutrophils (pb-PMNs).31 By hierarchic clustering of differentially regulated genes in our data set, we identified clusters of genes whose expression profiles were identical to those of defined azurophil, specific, and gelatinase granule proteins. This analysis demonstrated that Hp was annotated to the gene cluster encompassing various specific granule proteins including lactoferrin (Lf), a designated marker protein of specific granules. Hence, Hp transcripts were highly expressed in MYs (Figure 1A). Immunocytochemistry revealed that Hp protein, like Lf, is detectable in the cytosol of populations highly enriched in MYs, bm-PMNs, and pb-PMNs, but not PMs (Figure 1B). Overall, these findings demonstrate that Hp is synthesized in MYs and remains stored in a cytosolic compartment throughout granulocyte differentiation.
Hp and lactoferrin are synthesized at the myelocyte stage and stored in the cytosol of cells throughout granulocyte differentiation. BM populations highly enriched in PMs, MYs, bm-PMNs, and pb-PMNs were isolated from healthy donors. (A) Total RNA was purified from BM and PB populations and subjected to microarray analysis to monitor the expression profiles for Hp and Lf (marker for specific granules) transcripts during granulocyte differentiation (mean ± SD; n = 3).31 (B) Immunocytochemical staining of BM and PB populations using rabbit anti-human Hp and Lf antibodies demonstrates the cytoplasmic localization (red) of Hp and Lf from the myelocyte stage throughout granulocyte differentiation. BM populations highly enriched in PMs stained with rabbit anti-human Hp or Lf antibodies and populations stained with irrelevant rabbit IgG antibodies were all negative. Original magnification, × 400.
Hp and lactoferrin are synthesized at the myelocyte stage and stored in the cytosol of cells throughout granulocyte differentiation. BM populations highly enriched in PMs, MYs, bm-PMNs, and pb-PMNs were isolated from healthy donors. (A) Total RNA was purified from BM and PB populations and subjected to microarray analysis to monitor the expression profiles for Hp and Lf (marker for specific granules) transcripts during granulocyte differentiation (mean ± SD; n = 3).31 (B) Immunocytochemical staining of BM and PB populations using rabbit anti-human Hp and Lf antibodies demonstrates the cytoplasmic localization (red) of Hp and Lf from the myelocyte stage throughout granulocyte differentiation. BM populations highly enriched in PMs stained with rabbit anti-human Hp or Lf antibodies and populations stained with irrelevant rabbit IgG antibodies were all negative. Original magnification, × 400.
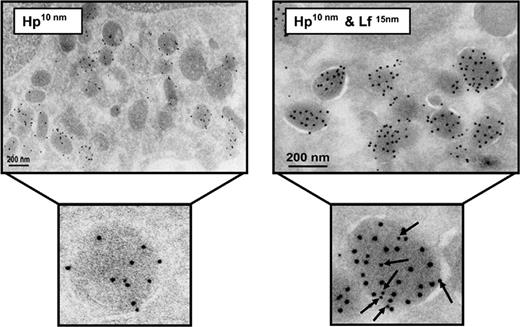
Hp and Lf colocalize in specific granules of neutrophils
To investigate the subcellular localization of Hp in neutrophils, we isolated subcellular fractions from disrupted neutrophils by 3-layer density gradient centrifugation. With this method, fractions highly enriched in azurophil, specific, and gelatinase granules and secretory vesicles are readily identified based on their high content of distinct marker proteins, including myeloperoxidase (MPO), gelatinase (Gel), and plasma albumin (Alb), respectively (Figure 2). As depicted in Figure 2, Western blot analysis demonstrated that the major part of Hp colocalized in subcellular fractions with a high content of Lf, a marker protein of specific granules. In contrast, subcellular fractions with high contents of MPO (azurophil granules), Gel (gelatinase granules), and Alb (secretory vesicles) contained only low amounts of Hp (Figure 2). To further substantiate the colocalization of Hp and Lf in specific granules of neutrophils, we performed immunoelectron microscopy on intact neutrophils using antibodies raised against Hp and Lf. As shown in Figure 3, Hp and Lf indeed colocalized in electron-dense specific granules. Hp was not observed in organelles other than those containing Lf. Taken together, these findings indicate that Hp is a genuine specific granule protein.
Neutrophils release Hp in response to activation
Once neutrophils have been attracted to sites of infection or injury, they respond to various inflammatory stimuli by immediate exocytosis of effector proteins primarily stored in granules and secretory vesicles. Exocytosis of effector proteins can be mimicked by in vitro activation of neutrophils using various stimuli. Several studies by our laboratory have documented that neutrophils stimulated by phorbol myristate acetate (PMA) release proteins contained in specific/gelatinase granules and secretory vesicles but only minor amounts of proteins contained in azurophil granules, whereas neutrophils stimulated by the calcium ionophore ionomycin release proteins stored in all 4 organelles.37,45 In addition, inflammatory stimuli such as fMLP, TNF-α, and serum-opsonized bacteria have been shown to activate neutrophils and to induce exocytosis of granule proteins in vitro.37,46
To investigate whether stimuli affecting the activation of neutrophils also affected the release of Hp, purified neutrophils were stimulated by PMA, ionomycin, fMLP, TNF-α, and serum-opsonized bacteria. Subsequent Western blot analysis of supernatants collected from PMA and ionomycin-stimulated neutrophils revealed a marked corelease of Hp and Lf (Figure 4A). Consistent with these findings, ELISA and Western blot analyses of supernatants and cell pellets collected after the stimulation of neutrophils by fMLP, TNF-α, and serum-opsonized bacteria revealed marked corelease of Hp, Lf, and gelatinase but not of MPO (Figure 4B). In contrast, unstimulated neutrophils did not release Hp, Lf, or gelatinase (Figure 4A-B).
Highly glycosylated Hp and lactoferrin colocalize in subcellular fractions enriched in specific granules. Subcellular fractions were isolated from purified peripheral-blood neutrophils and assayed by ELISA and Western blot analysis. Lines indicate subcellular fractions containing relative concentrations for MPO (marker for azurophil granules, peak concentration in fraction 5-433 μg/mL), Lf (marker for specific granules, peak concentration fraction 11-187 μg/mL), Gel (marker for gelatinase granules, peak concentration in fraction 16-33 μg/mL), and Alb (marker for secretory vesicles, peak concentration in fraction 21-2.2 μg/mL). Two forms of Hp were detected by Western blot analysis, an abundant form with a highly glycosylated β-chain of approximately 45 to 65 kDa that colocalized in fractions with high content of the specific granule protein Lf (fractions 10-15) and a scarce form with a β-chain of 39 kDa that colocalized in fractions containing Alb (fractions19-23), a protein endocytosed from plasma and stored in secretory vesicles of neutrophils.
Highly glycosylated Hp and lactoferrin colocalize in subcellular fractions enriched in specific granules. Subcellular fractions were isolated from purified peripheral-blood neutrophils and assayed by ELISA and Western blot analysis. Lines indicate subcellular fractions containing relative concentrations for MPO (marker for azurophil granules, peak concentration in fraction 5-433 μg/mL), Lf (marker for specific granules, peak concentration fraction 11-187 μg/mL), Gel (marker for gelatinase granules, peak concentration in fraction 16-33 μg/mL), and Alb (marker for secretory vesicles, peak concentration in fraction 21-2.2 μg/mL). Two forms of Hp were detected by Western blot analysis, an abundant form with a highly glycosylated β-chain of approximately 45 to 65 kDa that colocalized in fractions with high content of the specific granule protein Lf (fractions 10-15) and a scarce form with a β-chain of 39 kDa that colocalized in fractions containing Alb (fractions19-23), a protein endocytosed from plasma and stored in secretory vesicles of neutrophils.
Overall, these observations substantiate the colocalization of Hp and Lf in specific granules of neutrophils.
Neutrophil-derived Hp stored in specific granules is more glycosylated than plasma-derived Hp
Humans have 2 variants of the HP gene, the Hp 1 variant with a short α1-chain (approximately 10 kDa) and the Hp 2 variant with a long α2-chain (approximately 18 kDa), resulting from partial gene duplication of the α-chain. Both Hp variants have a common β-chain (approximately 39 kDa) that contains 4 N-linked glycans. In the present study, we identified 2 forms of Hp in neutrophils: (1) an abundant form with a β-chain of high molecular weight (approximately 45-65 kDa) that colocalized in subcellular fractions with a high content of Lf (Figure 2, fractions 10-15; Figure 5A, β-fractions) and (2) a scarce form with a β-chain of low molecular weight (approximately 39 kDa) that primarily colocalized in subcellular fractions with a high content of albumin, a plasma protein that is endocytosed and stored in secretory vesicles (Figure 2, fractions 19-23; Figure 5A, γ fractions).
Consistent with these findings, Western blot analysis of nonreduced samples, obtained from patients with the Hp 1-1 and Hp 2-1 phenotypes, revealed that Hp dimers and Hp multimers contained in pooled subcellular β-fractions—ie, specific granules—have higher molecular weights than those contained in plasma (Figure 5B).
To investigate whether the higher molecular weight of neutrophil-derived Hp compared with plasma-derived Hp was the result of a higher degree of β-chain glycosylation, pooled subcellular β-fractions (β-chain, approximately 45-65 kDa) and purified plasma Hp (β-chain, approximately 39 kDa) were subjected to N-deglycosylation by PNGase-F. Western blot analysis demonstrated a complete deglycosylation of β-chains contained in pooled subcellular β-fractions and plasma, resulting in β-chain bands with identical molecular weights of 30 kDa (Figure 5A).
Taken together, these findings demonstrate that neutrophils contain 2 forms of Hp, a scarce form of low molecular weight, endocytosed from plasma and stored in secretory vesicles, and a previously undescribed abundant form of high molecular weight that is synthesized in MYs and stored in specific granules.
Neutrophil-derived Hp stored in specific granules binds to Hb
It is well established that plasma-derived Hp can bind Hb and facilitate its clearance by macrophages. To investigate whether the highly glycosylated form of Hp contained in specific granules of neutrophils is capable of binding Hb, we performed affinity precipitation and surface plasmon resonance (SPR) analysis.
Affinity precipitation using pooled subcellular β-fractions and Hb-Sepharose beads resulted in precipitation of the highly glycosylated neutrophil-derived form of Hp, indicating tight binding to Hb (Figure 6A). Subsequently, SPR analysis revealed similar binding curves and kinetics for neutrophil- and plasma-derived Hp to Hb, indicating a similar functional affinity (Figure 6B). Because the neutrophil-derived Hp was prepared from pooled buffy coats (including Hp phenotypes 1-1, 2-1, 2-2) and therefore contained various multimeric Hp forms, an exact affinity constant could not be calculated from the binding curve. However, the estimated dissociation rate constants (Kd granula, 3.9 × 10 -4 s-1; Kd plasma, 1.7 × 10-4 s-1) were similar, indicating that neutrophil-derived Hp binds to Hb with a tightness similar to that of plasma-derived Hp.
Hp and lactoferrin colocalize in specific granules of neutrophils. Cryosections of peripheral-blood neutrophils were labeled with rabbit anti-human Hp antibodies followed by a 10-nm protein A-gold probe (left). In addition, cryosections (right) were double-labeled, first with a rabbit anti-human Hp antibody and a 10-nm protein A-gold probe and subsequently with a rabbit anti-human Lf antibody and a 15-nm protein A-gold probe. Immunoelectron microscopy demonstrates the ultrastructural colocalization of Hp (arrows) and Lf in specific granules.
Hp and lactoferrin colocalize in specific granules of neutrophils. Cryosections of peripheral-blood neutrophils were labeled with rabbit anti-human Hp antibodies followed by a 10-nm protein A-gold probe (left). In addition, cryosections (right) were double-labeled, first with a rabbit anti-human Hp antibody and a 10-nm protein A-gold probe and subsequently with a rabbit anti-human Lf antibody and a 15-nm protein A-gold probe. Immunoelectron microscopy demonstrates the ultrastructural colocalization of Hp (arrows) and Lf in specific granules.
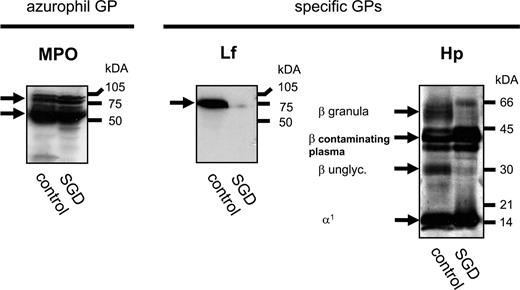
Blood cells from a patient with SGD lack neutrophil-derived Hp
SGD is a rare congenital disorder (5 reported cases) characterized by the lack of specific and gelatinase granules and their constituent granule proteins in neutrophils. Neutrophils from patients with SGD display atypical bilobed nuclei and are defective in chemotaxis and antibacterial activity. As a result, SGD patients are severely immunocompromised and experience early and frequent bacterial infections of the skin and respiratory tract.47 Because SGD neutrophils lack specific granule proteins, such as Lf, but contain azurophil granule proteins, such as MPO, we reasoned that Hp of high molecular weight (β-chain, approximately 45-65 kDa) should not be detected in blood cells from SGD patients. To test this hypothesis, we obtained blood-cell lysates from a child with a diagnosis of SGD.33 Immediately after birth, the child presented with postnatal sepsis and delayed separation of the umbilical cord. These incidents were succeeded by recurrent opportunistic infections requiring frequent courses of intravenous broad-spectrum antibiotic treatment. Peripheral-blood smears demonstrated neutrophils with abnormal morphology, including nuclei with Pelger-Huet anomaly (bilobed rather than trilobed appearance), and electron microscopy demonstrated azurophil but not specific granules in blood neutrophils.33
Neutrophils release Hp in response to activation. (A) Purified peripheral-blood neutrophils were stimulated by the calcium ionophore ionomycin (1 μM) and PMA (2.5 μg/mL) for 15 minutes, and the contents of exocytosed Hp and Lf in the supernatant were detected by Western blot analysis. Ionomycin- and PMA-activated neutrophils released Hp and Lf, whereas unstimulated neutrophils did not. (B) Purified neutrophils from one donor were stimulated for 15 or 30 minutes by PMA (2.5 μg/mL), fMLP (100 nM), TNF-α (50 ng/mL), and 10% autologous serum-opsonized E coli (multiplicity of infection, 10 bacteria per cell). Supernatants containing exocytosed granule proteins and cell pellets were subjected to ELISA analysis (MPO, Lf, Gel, top histogram) or Western blot analysis (Hp, lower histogram). The percentage of MPO, Lf, and Gel released by neutrophils was calculated as the amount of protein detected in the supernatant divided by the total amount of protein detected in the supernatant and pellet multiplied by 100.
Neutrophils release Hp in response to activation. (A) Purified peripheral-blood neutrophils were stimulated by the calcium ionophore ionomycin (1 μM) and PMA (2.5 μg/mL) for 15 minutes, and the contents of exocytosed Hp and Lf in the supernatant were detected by Western blot analysis. Ionomycin- and PMA-activated neutrophils released Hp and Lf, whereas unstimulated neutrophils did not. (B) Purified neutrophils from one donor were stimulated for 15 or 30 minutes by PMA (2.5 μg/mL), fMLP (100 nM), TNF-α (50 ng/mL), and 10% autologous serum-opsonized E coli (multiplicity of infection, 10 bacteria per cell). Supernatants containing exocytosed granule proteins and cell pellets were subjected to ELISA analysis (MPO, Lf, Gel, top histogram) or Western blot analysis (Hp, lower histogram). The percentage of MPO, Lf, and Gel released by neutrophils was calculated as the amount of protein detected in the supernatant divided by the total amount of protein detected in the supernatant and pellet multiplied by 100.
Blood samples obtained from the SGD patient and a healthy donor were depleted of erythrocytes, and lysates, including total nuclear cells (neutrophils and mononuclear cells) and residual plasma were subjected to Western blot analysis with the use of anti-human Hp, Lf, and MPO antibodies. Hp of high molecular weight (β-chain, approximately 45-65 kDa) and Lf were detected in cell lysates prepared from the healthy donor, but neither protein was detected in cell lysates from the patient with SGD (Figure 7). In contrast, comparable amounts of the azurophil granule protein MPO were detected in SGD and control lysates (Figure 7). Because of plasma contamination, Hp of low molecular weight (β-chain, approximately 39 kDa) was detected in SGD and control lysates. These results substantiate our findings that Hp is a genuine specific granule protein and are consistent with previous reports indicating that patients with SGD have a selected defect in the transcriptional regulation of granule protein expression in myeloid cells (but apparently not other cell types).
Hp located in specific granules of neutrophils is more glycosylated than plasma-derived Hp. (A) Pooled subcellular fractions isolated from peripheral-blood neutrophils and purified plasma Hp were analyzed by Western blot analysis using rabbit anti-human Hp antibody. Western blots to the left demonstrate pooled subcellular fractions highly enriched in azurophil granule proteins (α-fraction), specific granule protein (β1-fraction), gelatinase granule proteins (β2-fractions), and secretory vesicles containing mainly plasma proteins (γ-fractions). These Western blots show that the β-chain of Hp, primarily present in β1- and β2-fractions, has a higher molecular weight (approximately 45-65 kDa) than the β-chain of plasma-derived Hp (39 kDa) primarily present in γ-fractions (secretory vesicles). Western blots to the right demonstrate that Hp β-chains from specific granules (pooled β-fractions) and plasma samples have an identical molecular weight of 30 kDa after complete N-deglycosylation by PNGase-F. (B) Western blot analysis of nonreduced pooled β-fractions and plasma samples, prepared from patients with the Hp 1-1 and Hp 2-1 phenotypes with the use of rabbit anti-human Hp antibody. These Western blots demonstrate that Hp dimer and Hp multimers contained in pooled subcellular β-fractions (ie, specific granules) have higher molecular weights than those contained in plasma.
Hp located in specific granules of neutrophils is more glycosylated than plasma-derived Hp. (A) Pooled subcellular fractions isolated from peripheral-blood neutrophils and purified plasma Hp were analyzed by Western blot analysis using rabbit anti-human Hp antibody. Western blots to the left demonstrate pooled subcellular fractions highly enriched in azurophil granule proteins (α-fraction), specific granule protein (β1-fraction), gelatinase granule proteins (β2-fractions), and secretory vesicles containing mainly plasma proteins (γ-fractions). These Western blots show that the β-chain of Hp, primarily present in β1- and β2-fractions, has a higher molecular weight (approximately 45-65 kDa) than the β-chain of plasma-derived Hp (39 kDa) primarily present in γ-fractions (secretory vesicles). Western blots to the right demonstrate that Hp β-chains from specific granules (pooled β-fractions) and plasma samples have an identical molecular weight of 30 kDa after complete N-deglycosylation by PNGase-F. (B) Western blot analysis of nonreduced pooled β-fractions and plasma samples, prepared from patients with the Hp 1-1 and Hp 2-1 phenotypes with the use of rabbit anti-human Hp antibody. These Western blots demonstrate that Hp dimer and Hp multimers contained in pooled subcellular β-fractions (ie, specific granules) have higher molecular weights than those contained in plasma.
Neutrophil-derived Hp stored in specific granules binds to Hb. (A) Nonreduced pooled subcellular β-fractions from neutrophils were incubated with Hb-Sepharose beads and Sepharose control beads. Subsequently, beads were precipitated, and Hb, control eluates (contr. eluate), and pooled subcellular β-fractions (granula control [gran. contr.]) were subjected to Western blot analysis using rabbit anti-human Hp antibody. The Western blot demonstrates the presence of highly glycosylated neutrophil-derived Hp in eluates from Hb-Sepharose beads but not from Sepharose control beads, indicating that Hp contained in specific granules binds to Hb. (B) SPR analysis demonstrating the binding curve of highly glycosylated neutrophil-derived (granula) Hp and plasma-derived Hp to a Hb BIAcore sensor chip. Response units (RUs) correspond to the response difference between Hp and control samples. SPR analysis demonstrates similar binding curves/kinetics and dissociation rate constants (Kd granula, 3.9 × 10-4 s-1; Kd plasma,1.7 × 10-4 s-1) for both types of Hp.
Neutrophil-derived Hp stored in specific granules binds to Hb. (A) Nonreduced pooled subcellular β-fractions from neutrophils were incubated with Hb-Sepharose beads and Sepharose control beads. Subsequently, beads were precipitated, and Hb, control eluates (contr. eluate), and pooled subcellular β-fractions (granula control [gran. contr.]) were subjected to Western blot analysis using rabbit anti-human Hp antibody. The Western blot demonstrates the presence of highly glycosylated neutrophil-derived Hp in eluates from Hb-Sepharose beads but not from Sepharose control beads, indicating that Hp contained in specific granules binds to Hb. (B) SPR analysis demonstrating the binding curve of highly glycosylated neutrophil-derived (granula) Hp and plasma-derived Hp to a Hb BIAcore sensor chip. Response units (RUs) correspond to the response difference between Hp and control samples. SPR analysis demonstrates similar binding curves/kinetics and dissociation rate constants (Kd granula, 3.9 × 10-4 s-1; Kd plasma,1.7 × 10-4 s-1) for both types of Hp.
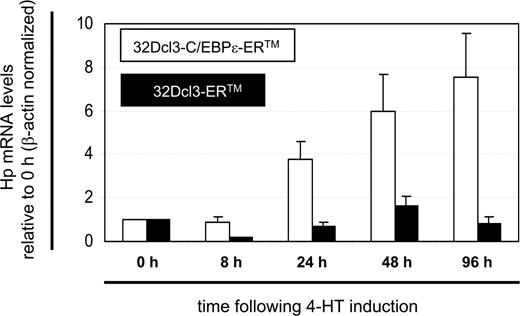
Induction of C/EBP-epsilon increases Hp transcript levels in myeloid 32Dcl3 cells
Hp expression in the liver is partially regulated by C/EBPβ.48,49 Another member of the C/EBP transcription factor family, C/EBPϵ, has been defined as a key regulator of terminal granulocyte differentiation (transition from promyelocytes into mature neutrophils).50 Functional loss of C/EBPϵ in mice, and some but not all currently reported SGD patients, results in the generation of dysfunctional neutrophils lacking specific and gelatinase granule proteins.47,51,52 Consistent with these findings, we have demonstrated that C/EBPϵ transcripts and protein are highly expressed in MYs (but not PMs or bm-PMNs) when specific granule proteins, including Hp and Lf, are synthesized.31,53 In addition, C/EBPϵ has been shown to induce expression of the specific granule protein Lf in vitro.54 Taken together, these findings suggest that C/EBPϵ might contribute to the transcriptional regulation of Hp expression in myeloid cells.
Hp and lactoferrin are absent in blood cells from a patient with SGD. Blood samples from a patient with SGD and a healthy donor (control) were depleted of erythrocytes, and lysates including total nuclear cells (neutrophils and mononuclear cells) and residual plasma were subjected to Western blot analyses using rabbit anti-human MPO, Lf, and Hp antibodies. Western blot analyses demonstrated that blood cells from the SGD patient expressed the azurophil granule protein MPO at comparable levels but expressed neither the specific granule protein Lf nor the highly-glycosylated Hp β-chain with a molecular weight of 45 to 65 kDa. Contamination of cell lysates with residual plasma resulted in the detection of Hp β-chain with a low molecular weight (39 kDa) in the control sample and the sample obtained from the SGD patient.
Hp and lactoferrin are absent in blood cells from a patient with SGD. Blood samples from a patient with SGD and a healthy donor (control) were depleted of erythrocytes, and lysates including total nuclear cells (neutrophils and mononuclear cells) and residual plasma were subjected to Western blot analyses using rabbit anti-human MPO, Lf, and Hp antibodies. Western blot analyses demonstrated that blood cells from the SGD patient expressed the azurophil granule protein MPO at comparable levels but expressed neither the specific granule protein Lf nor the highly-glycosylated Hp β-chain with a molecular weight of 45 to 65 kDa. Contamination of cell lysates with residual plasma resulted in the detection of Hp β-chain with a low molecular weight (39 kDa) in the control sample and the sample obtained from the SGD patient.
To investigate whether C/EBPϵ can induce the expression of Hp in vitro, we generated a myeloid 32Dcl3 cell line constitutively expressing a fusion protein containing the C/EBPϵ wild-type protein and the ligand-binding domain of the estrogen receptor (32Dcl3-C/EBPϵ-ER). With this cell line, the C/EBPϵ-ER fusion protein is maintained in the cytoplasm and only translocates to the nucleus to exert C/EBPϵ activity in the presence of the estrogen derivative 4-HT. Hence, the transcriptional activity of C/EBPϵ can be analyzed in an inducible manner. A 32Dcl3 cell line expressing only the ligand-binding domain of the estrogen receptor served as control (32Dcl3-ER).
Induction of 32Dcl3-C/EBPϵ-ER cells by 4-HT resulted in a 3.8-fold increase of Hp transcript levels within 1 day; after 4 days of 4-HT induction, Hp transcript levels were maximally increased (7.3-fold higher than baseline; Figure 8). Induction of 32Dcl3-ER control cells by 4-HT did not result in any increase of Hp transcript levels compared with baseline (0.2- to 1.6-fold change). These findings indicate that the expression of Hp in myeloid cells, as in hepatocytes, is at least partially regulated by members of the C/EBP family.
Discussion
The present study provides evidence that Hp is a genuine specific granule protein of human neutrophils by several means. First, Hp transcripts were highly expressed in MYs during granulocyte differentiation. In agreement with this finding, immunocytochemistry demonstrated the presence of Hp protein in cells from the MY stage and throughout granulocyte differentiation. In addition, immunoelectron microscopy and subcellular fractionation studies demonstrated the colocalization of Hp and Lf in specific granules, a finding consistent with the absence of Hp and Lf in blood cells collected from a patient with SGD. Finally, functional studies revealed that neutrophils corelease Hp and Lf, but not MPO, in response to PMA and various inflammatory stimuli that induce exocytosis of proteins primarily stored in secretory vesicles and specific/gelatinase granules, but not in azurophil granules.
Although immunoelectron microscopy and exocytosis assays are excellent tools to assess the subcellular localization of proteins in azurophil compared with specific/gelatinase granules, their levels of resolution might be insufficient to distinguish whether proteins are localized primarily in specific or gelatinase granules. Accordingly, more subtle assays, including subcellular fractionation and gene-expression profiling, are the methods of choice to subcategorize specific and gelatinase granule proteins of neutrophils. In the present study, subcellular fractionation showed that Hp colocalized with Lf, not gelatinase. In addition, gene-expression profiling demonstrated that transcripts for Hp and Lf were expressed at significantly lower levels in bm-PMNs compared with MYs and were barely detectable in pb-PMNs. In contrast, transcripts for gelatinase were expressed at the highest levels in MYs and bm-PMNs and at high levels in pb-PMNs (data not shown).31 Hence, Hp synthesis is terminated simultaneously with that of Lf during granulocyte differentiation and earlier than that of gelatinase. Based on these criteria, Hp is subcategorized as a specific rather than a gelatinase granule protein.
Hp expression in myeloid 32Dcl3 cells is induced by C/EBPϵ. Myeloid 32Dcl3 cells constitutively expressing a fusion protein containing the C/EBPϵ wild-type and the ligand-binding domain of the estrogen receptor (32Dcl3-C/EBPϵ-ER) were induced with 4-HT, resulting in nuclear translocation of C/EBPϵ-ER. Hp mRNA levels were measured relative to β-actin levels by reverse transcription (RT) real-time PCR at the indicated time points. Changes of Hp mRNA levels at indicated time points after 4-HT induction were calculated relative to the Hp mRNA level before 4-HT induction (0 hour) (mean ± SD; n = 3). Myeloid 32Dcl3 cells constitutively expressing the ligand-binding domain of the estrogen receptor (32Dcl3-ER) served as control.
Hp expression in myeloid 32Dcl3 cells is induced by C/EBPϵ. Myeloid 32Dcl3 cells constitutively expressing a fusion protein containing the C/EBPϵ wild-type and the ligand-binding domain of the estrogen receptor (32Dcl3-C/EBPϵ-ER) were induced with 4-HT, resulting in nuclear translocation of C/EBPϵ-ER. Hp mRNA levels were measured relative to β-actin levels by reverse transcription (RT) real-time PCR at the indicated time points. Changes of Hp mRNA levels at indicated time points after 4-HT induction were calculated relative to the Hp mRNA level before 4-HT induction (0 hour) (mean ± SD; n = 3). Myeloid 32Dcl3 cells constitutively expressing the ligand-binding domain of the estrogen receptor (32Dcl3-ER) served as control.
Hp is a highly glycosylated protein whose β-chains contain 4 N-linked glycans. Of interest, neutrophils contain 2 forms of Hp, a hitherto undescribed abundant form with highly glycosylated β-chains (45-65 kDa) that is stored in specific granules and a scarce form with “normally” glycosylated β-chains (39 kDa) that is stored in secretory vesicles and thus is endocytosed from plasma. Wagner et al32 recently reported that fully differentiated pb-PMNs store but do not synthesize Hp, leading to the hypothesis that neutrophil-derived Hp is endocytosed from the plasma and thus is primarily of liver origin. Results presented here are consistent with the presence of scarce amounts of liver-derived Hp endocytosed from plasma and stored in secretory vesicles of pb-PMNs. However, the results presented here extend earlier findings substantially by demonstrating that the major part of Hp present in fully differentiated pb-PMNs is not of liver origin but rather is synthesized in MYs and stored in specific granules. Affinity precipitation and SPR analysis demonstrated that highly glycosylated Hp from specific granules binds to Hb with a tightness similar to that of plasma-derived Hp. These findings support the idea that the glycosylation pattern of β-chains is characteristic for the cellular origin of Hp and does not interfere with its functional ability to bind Hb. However, it cannot be ruled out that neutrophil- and plasma-derived Hp differ with respect to anti-inflammatory activities. Hence, future studies are needed to delineate the functional properties of the highly glycosylated Hp contained in specific granules of neutrophils.
The promoter region of the Hp gene harbors functionally well-characterized APR-related binding sites, namely 2 C/EBP sites and a binding site for the signal transducer and activator of transcription 3 (STAT3).55,56 The proinflammatory cytokine IL-6 and glucocorticoids are principal regulators of Hp expression in the human liver.57,58 IL-6 mediates the phosphorylation of STAT3 in hepatocytes and enhances Hp expression through binding of STAT3 and C/EBPβ to the STAT and C/EBP binding sites, respectively.49,58
The hematopoietic growth factor G-CSF is an important regulator of granulocyte differentiation, underscored by the finding that mice deficient in G-CSF and the G-CSF receptor develop severe neutropenia.59,60 As IL-6 signaling mediates STAT3 phosphorylation in the liver, G-CSF induces STAT3 phosphorylation through the G-CSF receptor signaling pathway in myeloid cells.61,62 G-CSF signaling and resultant STAT3 phosphorylation have been shown to induce expression of the specific granule protein NGAL and the transcription factor C/EBPϵ in myeloid 32Dcl3 cells.54,63,64 In the present study, we showed that C/EBPϵ induces Hp expression in myeloid 32Dcl3 cells. Consistent with our previous observation that C/EBPϵ mRNA and protein are highly expressed in vivo in MYs when Hp is synthesized, these findings indicate that C/EBPϵ contributes to the regulation of Hp expression during granulocyte differentiation.31,53 Because MYs also express STAT3 and the G-CSF receptor,31,65 one might speculate that G-CSF signaling mediates a cooperative regulation of Hp expression by C/EBPϵ and STAT3 during granulocyte differentiation.
At present Hp is thought of as a plasma protein primarily synthesized by hepatocytes to mediate anti-inflammatory activities and immediate clearance of Hb released into plasma by erythrocytes as a consequence of hemolysis. However, the inflammatory mediator LPS has been shown to induce Hp in other cell types, including adipocytes, alveolar cells, and epidermal cells, suggesting a function for Hp at extravascular sites.66 In line with these observations, the present study demonstrates that Hp, like other specific granule proteins, is exocytosed within minutes by neutrophils after stimulation by PMA and various inflammatory stimuli. In agreement with our previous findings that the specific granule proteins Lf and human cathelicidin antimicrobial peptide are exocytosed by neutrophils in vivo after migration into skin lesions, the data presented here indicate that neutrophils represent the primary local source of Hp at sites of infection or injury.67,68
In conclusion, the present study supports a model in which neutrophils promote anti-inflammatory activities and clearance of Hb at sites of infection or injury through the release of Hp in order to reduce tissue damage and bacterial growth.
Prepublished online as Blood First Edition Paper, March 16, 2006; DOI 10.1182/blood-2005-09-3890.
Supported in part by the Danish Medical Research Council, the Danish Cancer Research Foundation, the Novo Nordisk Foundation, the Amalie Jørgensens Memorial Foundation, the Gangsted Foundation, and the Lundbeck Foundation.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Charlotte Horn and Marianne Lodahl their expert technical assistance. K.T.M. is the recipient of a scholarship from Rigshospitalet and the Danish Medical Research Council.





![Figure 6. Neutrophil-derived Hp stored in specific granules binds to Hb. (A) Nonreduced pooled subcellular β-fractions from neutrophils were incubated with Hb-Sepharose beads and Sepharose control beads. Subsequently, beads were precipitated, and Hb, control eluates (contr. eluate), and pooled subcellular β-fractions (granula control [gran. contr.]) were subjected to Western blot analysis using rabbit anti-human Hp antibody. The Western blot demonstrates the presence of highly glycosylated neutrophil-derived Hp in eluates from Hb-Sepharose beads but not from Sepharose control beads, indicating that Hp contained in specific granules binds to Hb. (B) SPR analysis demonstrating the binding curve of highly glycosylated neutrophil-derived (granula) Hp and plasma-derived Hp to a Hb BIAcore sensor chip. Response units (RUs) correspond to the response difference between Hp and control samples. SPR analysis demonstrates similar binding curves/kinetics and dissociation rate constants (Kd granula, 3.9 × 10-4 s-1; Kd plasma,1.7 × 10-4 s-1) for both types of Hp.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/108/1/10.1182_blood-2005-09-3890/2/m_zh80130697720006.jpeg?Expires=1769086415&Signature=P8eHl9p84NTj9WANf5ZP3CO67DwwGNw5Uxgns2IiILzlwktbgS7M7pAA4j6bqDqUPKBsYmBxG5ZcwqqPCvnxlfMXW8LV7~rgqtHy25YeWLDh9iNFUyJAuOSa-WEHHWF7-xnCGW~Gi8pGSIxP4EzmNuVLK2XCTKv6fFvQhXYMDeUeLVzNdgfq7sYkxpT7ywH0h4LPBB9I39bagHuGH88TIKeveqAyhTJZFrjU2hHYPZ2KLtN93JX6oc4nwglhQ5U94HQlgA6KkF8-TPlnA0C~kEh-ynp1YOHLw5EJO3upf8cSd3HwSEUbtJVsSKj4U0ru~bWZLyC9jsJ2RiF0L8vc5A__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal