Abstract
The synthesis of nitric oxide (NO) in the circulation has been attributed exclusively to the vascular endothelium. Red blood cells (RBCs) have been demonstrated to carry a nonfunctional NO synthase (NOS) and, due to their huge hemoglobin content, have been assumed to metabolize large quantities of NO. More recently, however, RBCs have been identified to reversibly bind, transport, and release NO within the cardiovascular system. We now provide evidence that RBCs from humans express an active and functional endothelial-type NOS (eNOS), which is localized in the plasma membrane and the cytoplasm of RBCs. This NOS is regulated by its substrate l-arginine, by calcium, and by phosphorylation via PI3 kinase. RBC-NOS activity regulates deformability of RBC membrane and inhibits activation of platelets. The NOS-dependent conversion of l-arginine in RBCs is comparable to that of cultured human endothelial cells. RBCs in eNOS-/- mice in contrast to wild-type mice lack NOS protein and activity, strengthening the evidence of an eNOS in RBCs. These data show an eNOS-like protein and activity in RBCs serving regulatory functions in RBCs and platelets, which may stimulate new approaches in the treatment of NO deficiency states inherent to several vascular and hematologic diseases.
Introduction
Nitric oxide (NO) is a signaling molecule of major importance present in various cell types.1,2 It modulates not only the function of the vascular wall but also that of blood cells, such as platelets and leukocytes. NO is synthesized by a family of NO synthases (NOSs) through the conversion of l-arginine to l-citrulline, using molecular oxygen. Until recently, the expression pattern of NOS isoforms appeared to be cell specific. Constitutively expressed neuronal and endothelial NOS (referred as NOS1 and NOS3) were identified in and cloned from neuronal and endothelial cells at first. Inducible NOS (NOS2) was originally isolated from activated macrophages.3,4 In the vascular system under resting conditions, NO synthesis has been attributed exclusively to the vascular endothelium expressing a NOS3 (eNOS) isoform. Initially thought to be a simple calmodulin-regulated enzyme, it is clear that eNOS has evolved to be tightly controlled by cofactors and posttranslational modifications, phosphorylation on multiple residues, and regulated protein-protein interactions.5,6
To date, human blood and, in particular, hemoglobin-carrying red blood cells (RBCs) have been considered as a major sink of NO.7,8 Although early reports postulated a NOS resident in RBCs,9 subsequent studies were unable to confirm an active NOS within RBCs.10 Current information on the NOS isoform, its localization, and functional activity within RBCs is still inconsistent and subject to considerable debate. Most importantly, a NOS-dependent formation and release of NO-related species from RBCs has not been shown so far. In fact, the diffusion-limited chemical inactivation of NO by intra-erythrocytic hemoglobin would suggest that even if RBCs contain NOS, NO production from such would represent a futile vestigial function derived from an earlier stem-cell precursor (prior to RBC hemoglobinization).
Indeed, the characterization and proof of a functional NOS in RBCs has been hampered by the high content of hemoglobin. First, the complex and oxygen-sensitive biochemistry of NO with intracellular and extracellular proteins8 demands a composite analysis of the various constituents of the circulating NO pool to assess RBC-based NOS activity in blood. Second, the extraordinary high protein content of RBCs precludes standard procedures for characterization of NOS protein. Therefore RBC-specific approaches have to be elaborated to allow identification and localization of NOS and its regulation.
Using immunofluorescence confocal microscopy, standard thin-section and immunogold cryosection, freeze-fracture electron microscopy, Western blotting, and reverse transcriptase-polymerase chain reaction (RT-PCR) we provide unequivocal evidence that human RBCs express an active NOS. Activity of NOS was analyzed by the release of NO and NO-related species and the conversion rate of the NOS substrate l-arginine. In human RBCs, NOS-derived NO regulates deformability of RBC membrane and inhibits platelet function. Further examinations in eNOS-deficient mice revealed an endothelial type of NOS. These data challenge the current dogma that intravascular NO availability is directed merely through the balance of the NO-synthesizing endothelium and NO-inactivating RBCs.
Patients, materials, and methods
RBC preparation
For all investigations blood was taken from the antecubital vein of healthy human volunteers. For the measurements of RBC-NOS activity and the determination of eNOS mRNA and protein, RBCs were separated via differential centrifugation. Purity of the RBC preparation was controlled by 3 independent methods: (i) Pappenheim staining of blood slides, (ii) flow cytometry (MÖLAB, Hilden, Germany), and (iii) differentiating platelets and white blood cells (WBCs) from RBCs by fluorescence-activated cell sorter (FACS) analysis with labeled CD45 and CD42 antibodies. Erythrocyte membranes (ghosts) were isolated as previously described11 for measurement of the NOS activity by the citrulline assay. Murine blood was taken by cardiac puncture (C57BL6 [wild type; WT] and homozygous eNOS knock-out [eNOS-/-] mice; genetic background C57BL612 ). The study was performed in accordance with the rules of the internal review board and the tenets of the Helsinki protocol. All subjects gave written informed consent before participating in the study.
Determination of eNOS protein
Antibodies. Endothelial nitric oxide synthase (eNOS) was immunolabeled using a mouse monoclonal antibody (clone 3; BD Transduction Labs, Lexington, KY) or polyclonal antibodies (L12932/b, Alexis Biochemicals, Grünberg, Germany; temp, Biomol, Hamburg, Germany; N3893, Sigma-Aldrich, München, Germany). Neuronal NOS (nNOS) was immunolabeled using a polyclonal antibody of human nNOS (clone pAb; BD Transduction Labs). Inducible NOS (iNOS) was immunolabeled using a polyclonal antibody of mouse iNOS (clone pAb; BD Transduction Labs). The monoclonal antibody GARP-50 to detect stomatin was a gift of Prof Dr R. Prohaska (Institute of Medical Biochemistry, University of Vienna, Austria). The immunolabeling to detect eNOS shown in Figures 1, 2, 3 was carried out using the rabbit polyclonal antibodies against human eNOS (Biomol, Alexis Biochemicals) and the phosphorylated eNOS (Ser1177, peNOS; Upstate, Lake Placid, NY; Figure 5). Antibodies against Lamp-1 and proteins of the inner nuclear membrane, LAP2β and emerin, were used as controls. Primary antibodies were diluted to a final concentration of 0.25 to 0.5 μg/mL. For purity control of the RBC preparation, specific antibodies for surface proteins of WBCs and platelets were selected (CD42 and CD45 antibodies, PE labeled; BD Biosciences Pharmingen, Heidelberg, Germany).
Immunofluorescence and confocal microscopy. Fixation and staining of RBCs was done according to standard protocols.13 For eNOS staining, RBCs were fixed in 4% paraformaldehyde in 0.1 M phosphate-buffered saline (PBS) at room temperature for 30 minutes. After extensive washing, they were incubated for 1 hour in PBS containing 1% bovine serum albumin (BSA) to block nonspecific binding and 0.05% Tween 20 for permeabilization. RBCs were immunolabeled with anti-eNOS antibodies for 1 hour, followed by washing and incubation with anti-mouse or anti-rabbit FITC-conjugated secondary antibodies (Dianova, Hamburg, Germany) for 1 hour. The preparations were mounted in fluorescent mounting medium (DAKO Cytomation, Hamburg, Germany) and examined in a fluorescence microscope or confocal laser scanning microscope equipped with a 100 ×/1.4 oil immersion objective lens (LSM 5 Pascal with Visual Macro Editor software; Zeiss, Jena, Germany).14,15 For immunohistochemistry of the phosphorylated NOS,16 untreated or insulin-treated RBCs (each n = 8) were fixed with 4% paraformaldehyde in 0.1 M PBS for 30 minutes. After several washing steps in 0.1 M PBS, RBCs were stroked on glass and heat fixed. Thereafter they were washed in 0.1 M tris-buffered saline (TBS), permeabilized for 30 minutes with 0.1% trypsin, placed in a solution of 2% hydrogen peroxide and 80% methanol PBS for 20 minutes, and treated with 3% milk powder in 0.1 M TBS for 30 minutes at room temperature. Incubation with the primary antibody was performed for 40 minutes in a 0.1 M TBS solution containing 0.3% milk powder, 0.03% Tween 20, and the primary polyclonal rabbit antibody against peNOS (1:500). After rinsing with TBS, the sections were incubated with the secondary goat antirabbit antibody (Dako, Glostrup, Denmark) at a dilution of 1:400 for 30 minutes. For negative controls, RBCs without primary antibody incubation were used. A streptavidin-horseradish-peroxidase conjugate (Amersham, Little Chalfont, England) was applied as a detection system (1:150 dilution) for 30 minutes. For analysis, only insulin-treated and controls from one preparation and staining were compared. Immunohistochemistry was examined using a Leica RM2000 microscope (Leica, Wetzlar, Germany) equipped with a 40 ×/0.75 objective lens, a Sony DXC 1850 P CCD camera (Sony, Cologne, Germany), and Image G software (National Institutes of Health, Bethesda, MD).
Thin-section electron microscopy and ultrathin cryosection electron microscopy. RBCs were fixed in 2% glutaraldehyde and 0.5% osmium tetroxide in 0.1 M PBS, dehydrated with ethanol, and embedded in Epon using standard procedures.14 Thin sections were cut using an ultramicrotome and contrasted with uranyl acetate and lead citrate. For cryoimmunoelectron microscopy, RBCs were fixed in 1% paraformaldehyde in 0.1 M PBS prepared according to Tokuyasu17 and immunogold labeled for eNOS (described in “Freeze-fracture replication,” “Immunolabeling of freeze-fracture replicas and cryosections,” and “Electron microscopy”).
Freeze-fracture replication. Unfixed RBCs were centrifuged briefly in 30% glycerol (< 1 minute), fixed in Freon 22 cooled with liquid nitrogen, and freeze fractured in a BA 310 freeze-fracture unit (Balzers, Balzers, Lichtenstein) at -100°C. Replicas of the freshly fractured cells were immediately made by electron beam evaporation of platinum-carbon and carbon at angles of 38° and 90° and to thicknesses of 2 nm and 20 nm, respectively. The replicas were incubated overnight in 5% sodium dodecyl sulfate (SDS) to remove cellular material except for those molecules adhering directly to the replicas. They were then washed in distilled water and incubated briefly in 5% BSA before immunolabeling.18-20
Immunolabeling of freeze-fracture replicas and cryosections. Freeze-fracture replicas and ultrathin cryosections of RBCs were immunogold labeled with anti-eNOS antibodies followed by a secondary antibody 18-nm gold conjugate. Double immunogold labeling of freeze-fracture replicas of RBCs was carried out using a mixture of anti-eNOS and antistomatin antibodies followed by a mixture of goat anti-rabbit 18-nm and goat anti-mouse 12-nm gold conjugates (both conjugates from Jackson Immuno Research, West Grove, PA). Control specimens, prepared without the primary antibodies, were essentially free of gold particles. Antibodies against Lamp-1, LAP2β, and emerin did not bind to replicas or cryosections of RBCs.
Electron microscopy. Examination of thin sections, immunogold-labeled ultrathin cryosections, and immunogold-labeled freeze-fracture replicas was carried out using a Philips 410 transmission electron microscope with original magnification, × 1200 (Philips, Amsterdam, The Netherlands) and ditabilis imaging software (ditabilis, Erlangen, Germany). Observations on freeze-fracture/immunogold replicas and ultrathin cryosections were based on examination of over 200 cells.
Western blotting. For Western blot analysis, 50 μg protein of human RBC membranes as well as 20 μg of human aortic endothelial-cell extracts (HAECs) were electrophoretically separated on a 7.5% SDS polyacrylamide gel. The proteins were transferred to nitrocellulose membrane and probed with the eNOS antibody. Immunoreactive bands were detected using the Super Signal West Femto Maximum Sensitivity System (Pierce, Bonn, Germany).
Determination of eNOS mRNA
Total RNA was isolated and reverse transcribed according to OneStep RT-PCR Kit (Qiagen, Hilden, Germany) using the following eNOS primers: 5′-TGGCGAAGCGAGTGAAGGCGACAA-3′,3′-AAAGGCGCAGAAGTGGGGGTATG-5′; product, 450 bp. Primer sequences as well as length of mRNA products for endoglin were taken from Li et al,21 for β-3 integrin from GenBank (GenBank accession nos. G26607, M25108), and for β-globin from Smith et al.22 All primer pairs were synthesized by Invitrogen (Carlsbad, CA). In order to amplify CD45 mRNA we used commercially available primers (Maxim Biotech, Rockville, MD). Human umbilical venous endothelial-cell (HUVEC) eNOS mRNA fragments served as a positive control. In addition, iNOS and nNOS fragments were amplified by RT-PCR using commercially available primer pairs (Stratagene, Amsterdam, The Netherlands). To verify the eNOS-specific product, a nucleic acid fragmentation was done using BstEII.
Each RT-PCR reaction was carried out according to the protocol of the manufacturer (Qiagen Onestep RT-PCR Kit) and accompanied by a negative control without RT enzymes or RNA template. WBCs and platelets were prepared at a cell count equivalent to whole blood and subjected to the same protocol. mRNA products were separated on 1% agarose and visualized by ethidium bromide staining.
Measurement of NO formation and NOS activity
Rate of NO formation was measured by the conversion of l-arginine to citrulline in membrane preparation from RBCs.23 NO release from RBCs was quantified using the oxyhemoglobin assay.24 NO release was quantified continuously; oxyhemoglobin solution was pumped (2 mL/min) along a RBC reservoir. Control buffer, l-arginine (3 mM), and NG-monomethyl-l-arginine acetate (l-NMMA; 3 mM) were applied consecutively into the flow system. Head space nonreductive chemiluminescence (CLD) served as a second independent method to detect RBC-NOS-dependent NO release. RBCs were separated and placed in a flow reaction chamber. Control buffer, l-arginine (3 mM), and l-NMMA (3 mM) were consecutively applied into the reaction chamber. The oxidative metabolites nitrite and nitrate were quantified by flow injection analysis after specific sample processing with or without prior vanadium-chloride incubation, respectively.25,26 Reductive CLD was used to determine the nitros(yl)ated adducts (RXNO, the sum of all nitroso compounds).27,28 Plasma nitrite was determined at baseline and 30 minutes after incubation (37°C) of 2 mL of blood with either l-arginine (3 mM), d-arginine (3 mM), Nω-nitro-l-arginine (l-NNA; 3 mM), EDTA (5 mM), wortmannin (20 nM), insulin (197.3 pM [27.5 μU]), Ca-ionophore (A-23187; 5 μM), or buffer as control. Dose dependency of RBC-NOS activity for its substrate was determined by measuring plasma nitrite after incubation of blood with l-arginine (0.3, 3, 30, 300, 3000 μM, with prior arginine depletion by arginase [4 U/mL] and inhibition of arginase activity with l-Valin [30 mM], subsequent). Plasma nitrite, nitrate, and RXNO were determined at baseline and 30 minutes (7.5 minutes for RXNO) after incubation (37°C) with l-arginine (3 mM), l-NNA (3 mM), or buffer. All incubation protocols were done at physiologic pH in venous blood samples.
Hemorheologic assays
Deformability of RBCs was determined after incubation of whole blood with l-arginine (3 mM), l-NNA (3 mM), l-NNA with oxyhemoglobin (100 μM), or buffer for 30 minutes. The analyses were performed using filter membranes with a pore size of 5 μm. RBCs (hematocrit of 0.35 [35%] in buffer) were passed through the filter with constant suction (-10 cm H2O).29 Platelet aggregation in platelet-rich-plasma (PRP) was recorded turbidimetrically, and VASP phosphorylation of platelets was detected by Western blot.30 Therefore, whole blood was incubated for 10 minutes with either 3 mM l-arginine, 3 mM l-NNA, or buffer after stimulation with ADP (10 μM). The same incubation set up was also carried out on PRP without RBCs.
Statistical analysis
Data are expressed as mean ± SEM. Student t or Mann-Whitney test was used where appropriate. P values less than or equal to .05 were accepted as significant.
Results
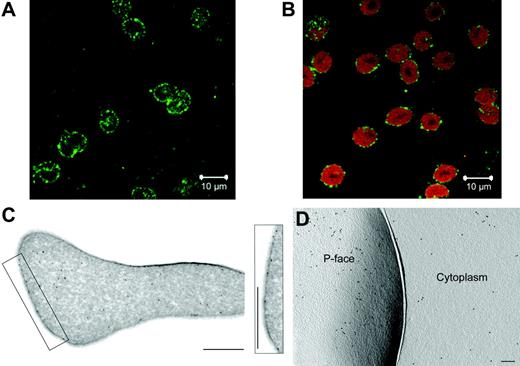
In RBCs of healthy volunteers, confocal microscopies demonstrated a distinct ring of eNOS immunofluorescence staining surrounding the cytoplasm and, to a lesser extent, punctuate immunofluorescence structures throughout the entire cytoplasm (Figure 1A). Coincubation with antibodies directed toward RBC-specific glycophorin A indicated that RBCs were uniformly positive for the eNOS protein (Figure 1B). Control experiments using double staining with eNOS and CD42 antibodies (n = 3) excluded the possibility that eNOS signal was derived from activated platelets clustered to the outer RBC membrane. RBCs did not stain for iNOS or nNOS (n = 3; data not shown).
Evidence of eNOS protein in human RBCs. eNOS was detected in RBCs from healthy volunteers using immunofluorescence confocal microscopy (A-B), standard thin-section and immunogold cryosection (C), and freeze-fracture electron microscopy (D). (A-B) Every single RBC stains positive for eNOS (FITC labeled, green; A), shown via double-staining with an RBC-specific antibody (glycophorin A, PE labeled, red; B; n = 3). (C-D) Higher spatial-resolution confirms these results and labels eNOS in the cytoplasm and in the plasma membrane with 2 independent preparation techniques (n = 5). The concentration of eNOS label is lower in the cytoplasm than in the P-face of the plasma membrane. Bars indicate (C and inset) 1 μm; (D) 0.2 μm.
Evidence of eNOS protein in human RBCs. eNOS was detected in RBCs from healthy volunteers using immunofluorescence confocal microscopy (A-B), standard thin-section and immunogold cryosection (C), and freeze-fracture electron microscopy (D). (A-B) Every single RBC stains positive for eNOS (FITC labeled, green; A), shown via double-staining with an RBC-specific antibody (glycophorin A, PE labeled, red; B; n = 3). (C-D) Higher spatial-resolution confirms these results and labels eNOS in the cytoplasm and in the plasma membrane with 2 independent preparation techniques (n = 5). The concentration of eNOS label is lower in the cytoplasm than in the P-face of the plasma membrane. Bars indicate (C and inset) 1 μm; (D) 0.2 μm.
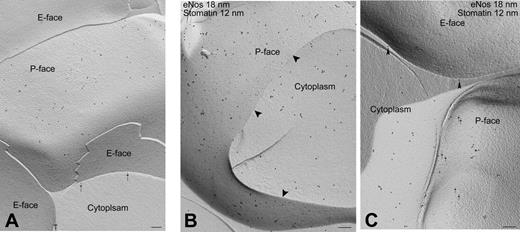
In ultrathin cryosection immunolabeling, eNOS was seen in the cytoplasm and along the plasma membrane of RBCs (Figure 1C insert). Fracturing of frozen RBCs splits membranes into their 2 constituent half-membrane leaflets along a plane between the hydrophobic tails of the phospholipids in the bilayer, revealing one leaflet attached to the extracellular space (E-face) and the other leaflet attached to the cytoplasm (P-face). The eNOS label was found exclusively on the P-face of the plasma membrane. The eNOS label was widely dispersed across the P-face of the plasma membrane, with its expression being 20% to 30% greater in the membrane than in the RBC cytoplasm (Figure 1D). Stomatin, a protein exclusively located at RBC membranes, was exclusively found on the P-face of the plasma membrane but not in the cytoplasm (Figure 2A) or on the E-face of the plasma membrane (Figure 2C). By double immunogold labeling, using gold markers of distinct sizes, eNOS and stomatin are both seen in the P-face of the plasma membrane (Figure 2B) but not on the E-face of the plasma membrane (Figure 2C).
Subcellular localization of NOS protein in RBCs. (A) Stomatin label is found exclusively on the P-face of the plasma membrane. No label is seen on the E-face or the cytoplasm. The arrows indicate stomatin label over cross-fractured P-face. (B) Fracture of a single RBC permits simultaneous viewing of portions of the plasma membrane (P-face) and the cytoplasm. Gold markers of distinct sizes were used to identify eNOS (18-nm gold) and stomatin (12-nm gold). Both are present on the P-face of the plasma membrane, whereas merely eNOS is found in the cytoplasm. Arrowheads indicate the line of fracture plane between the plasma membrane and the cytoplasm. (C) In contrast to the positive staining in the cytoplasm and the P-face of the RBC membrane, neither eNOS label nor stomatin label is found on the E-face of the plasma membrane. Bars, 0.2 μm.
Subcellular localization of NOS protein in RBCs. (A) Stomatin label is found exclusively on the P-face of the plasma membrane. No label is seen on the E-face or the cytoplasm. The arrows indicate stomatin label over cross-fractured P-face. (B) Fracture of a single RBC permits simultaneous viewing of portions of the plasma membrane (P-face) and the cytoplasm. Gold markers of distinct sizes were used to identify eNOS (18-nm gold) and stomatin (12-nm gold). Both are present on the P-face of the plasma membrane, whereas merely eNOS is found in the cytoplasm. Arrowheads indicate the line of fracture plane between the plasma membrane and the cytoplasm. (C) In contrast to the positive staining in the cytoplasm and the P-face of the RBC membrane, neither eNOS label nor stomatin label is found on the E-face of the plasma membrane. Bars, 0.2 μm.
Using Western blot analysis, an eNOS-specific protein was detected within human RBCs (Figure 3A). In purified human RBCs, RT-PCR identified eNOS-encoding mRNA (Figure 3B). Restriction analysis with endonuclease BstEII (received products 166 bp and 283 bp) confirmed the validity of the detected eNOS mRNA (n = 3). Since NOS may be present in platelets,3 WBCs,31 or circulating endothelial progenitor cells,32 we carefully quantified other blood cells and defined the purity of the RBC fraction to be 99.99 997% (only 2 platelets in 6 million RBCs, no WBCs; n = 5). To further strengthen the findings on purity, we amplified mRNA fragments from purified blood cell fractions and compared them with whole blood as positive control using the following reference protein mRNA sequences: endoglin, CD45, β-3 integrin, and β-globin for HUVECs, WBCs, platelets, and RBCs, respectively (Figure 3B). These results confirmed the specificity of eNOS mRNA detected within RBCs, performing cell type-specific control PCR. iNOS or nNOS mRNA were not detected in RBCs (n = 5).
Evidence of eNOS expression in RBCs. (A) Western blot analysis revealed an eNOS-specific band at 140 kDa in preparations of RBCs (lanes 2 and 3 are derived from diluted preparations [Hct 20%, 10%, and 5%, respectively; with 15, 7.5, and 3.8 μg protein/lane]). This band is equivalent to positive controls of human aortic endothelial cells (HAECs; 2 μg protein/line) and myocardium (cell lysate; 1 μg protein/line). (B) The 450-bp fragment of eNOS mRNA from RBCs corresponds to the control of HUVECs and whole blood. The purity of the RBC fraction was confirmed by mRNA amplification of reference proteins: endoglin for HUVECs, β-globin for RBCs, β-3 integrin for platelets, and CD45 for WBCs. Whole blood was taken as positive control.
Evidence of eNOS expression in RBCs. (A) Western blot analysis revealed an eNOS-specific band at 140 kDa in preparations of RBCs (lanes 2 and 3 are derived from diluted preparations [Hct 20%, 10%, and 5%, respectively; with 15, 7.5, and 3.8 μg protein/lane]). This band is equivalent to positive controls of human aortic endothelial cells (HAECs; 2 μg protein/line) and myocardium (cell lysate; 1 μg protein/line). (B) The 450-bp fragment of eNOS mRNA from RBCs corresponds to the control of HUVECs and whole blood. The purity of the RBC fraction was confirmed by mRNA amplification of reference proteins: endoglin for HUVECs, β-globin for RBCs, β-3 integrin for platelets, and CD45 for WBCs. Whole blood was taken as positive control.
Enzyme activity of RBC-NOS was determined by specific conversion of l-arginine to citrulline (0.3 ± 0.1 pmol/min/mg protein; n = 5; Figure 4A). This enzyme activity was comparable to that in cultured HUVECs (0.7 ± 0.1 pmol/min/mg protein; n = 5). In addition, we determined the release of NO itself or related intermediates releasing NO into the surrounding plasma—in the following described as the “rate of NO release”—using 2 independent methods: the rate of NO release was 5.9 ± 0.8 pmol/min/mL determined by nonreductive CLD and 12.4 ± 3.5 pmol/min/mL determined using the oxyhemoglobin assay during stimulation with l-arginine (Figure 4B-C).
In addition to these assays, the changes of NO metabolites in plasma were assessed by measurement of accumulated nitrite, nitrate, and RXNO in venous blood samples following NOS stimulation with l-arginine or NOS inhibition with l-NNA. After incubation with saline, plasma levels were detected as 39 ± 6 μM for nitrate, 38 nM for nitrite, and 19 nM for RXNO. During NOS stimulation with l-arginine, nitrate, nitrite, and RXNO increased significantly by 10%, 157%, and 89% (nitrate to 43 μM; nitrite to 98 nM, RXNO to 36 nM), whereas NOS inhibition with l-NNA prevented the increase of all plasma NO metabolites (Figure 4D-F).
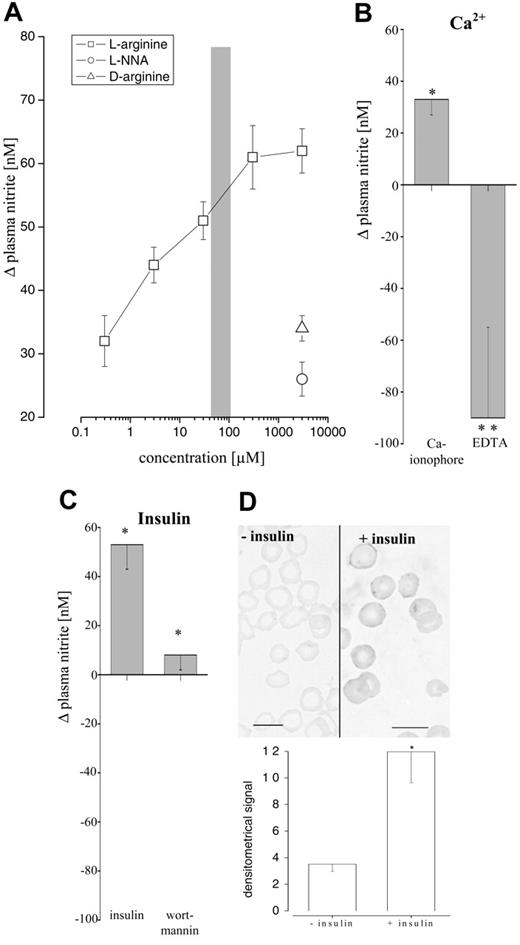
To further study mechanisms regulating RBC-NOS activity, changes in plasma nitrite were measured in whole blood at physiologic hematocrit (Hct). Nitrite has been shown to reflect acute changes of eNOS activity in humans.33,34 Apart from the endothelium-derived or RBC-derived NO formation increases in plasma, nitrite may be counterbalanced by the rapid uptake of nitrite into RBCs and further oxidation35 or reduction.36 In endothelial cells the activity of eNOS has been shown to depend on an adequate supply of l-arginine and calcium and the phosphorylation by Akt-phosphatidylinositol-3′-kinase (PI3K).37,38 In RBCs we found an identical pattern of regulatory mechanisms (Figure 5A-D). Interestingly, the changes in plasma nitrite upon stimulation of whole blood with l-arginine were dose dependent within a physiologic range of l-arginine levels, previously described in plasma and RBCs,39 pointing toward the possibility of a tight control of RBC-NOS activity by substrate availability.
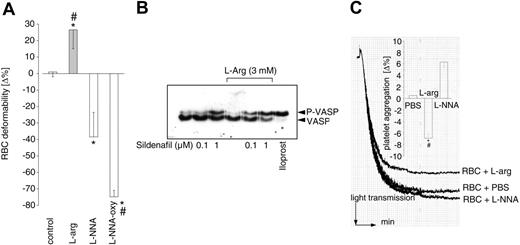
RBC membrane fluidity and deformability is crucial for the adequate passage of RBCs through the microvasculature. RBC deformability was assessed in relation to RBC flow rate through a filter system. l-arginine significantly increased RBC deformability, whereas NOS inhibition (l-NNA) or addition of the NO scavenger oxyhemoglobin reduced RBC deformability, preventing the adequate passage of RBCs through the filter (Figure 6A). Phosphorylation of the vasodilator-stimulated phosphoprotein (VASP) is known to prevent platelet activation.30,40 When studied in the presence of the phosphodiesterase-5 inhibitor sildenafil, a significant (P < .05; n = 5) phosphorylation of VASP in platelets (on top of the effect of sildenafil) was observed when whole blood was incubated with l-arginine. l-arginine-challenged RBCs in whole blood suppressed platelet aggregation to ADP. This reduction of platelet aggregation was prevented by NOS inhibition with l-NNA (Figure 6B). As a control, the incubation of PRP with l-arginine in absence of RBCs did not affect platelet aggregation and VASP phosphorylation (Figure 6C; P < .05).
Evidence of NOS activity in RBCs. (A) NOS activity was detected by enzymatic conversion of l-arginine23 in RBC membranes derived from human blood samples (n = 4). (B-C) RBC-NOS-dependent rate of NO release was measured with 2 independent methods. (B) The oxyhemoglobin assay. Purified RBCs from venous blood were placed in a reservoir separated from circulating oxyhemoglobin by a dialysis membrane (2.5-3.0 nm [25-30 Å]), inhibiting exchange of RBCs and oxyhemoglobin. In order to measure NO release by NO-dependent conversion of oxyhemoglobin to methemoglobin, time-dependent changes in absorption between 411 nm (isosbestic point) and 401 nm (the highest difference in absorbance) were determined via difference spectrophotometric analysis.24 Buffer (control), l-arginine (l-arg), and l-NMMA were applied subsequently to the system. Arrows indicate the duration of infusion of the respective agents. l-arginine led to an increase of NO release from 0.6 to 14 pmol/mL/min. Inhibition with l-NMMA reduced NO release to 1.4 pmol/mL/min. (C) The nonreductive CLD. Purified RBCs from venous blood were reconstituted with buffer (control) and placed into a reaction chamber flowed with helium (to avoid excessive foaming, antifoaming reagent was added and the Hct diluted to 0.08 [8%]). Time-dependent NO release in the presence or absence of l-arginine or l-NMMA was detected directly in the gas phase (calculated to mL whole blood per measurement period). (D-F) Changes in accumulated plasma RXNO, nitrite, and nitrate were determined in blood samples after incubation with l-arginine (stimulation) and l-NNA (inhibition). Changes were compared with control conditions (incubation with PBS). * indicates significant difference from control; and #, difference from l-arg, P less than .05.
Evidence of NOS activity in RBCs. (A) NOS activity was detected by enzymatic conversion of l-arginine23 in RBC membranes derived from human blood samples (n = 4). (B-C) RBC-NOS-dependent rate of NO release was measured with 2 independent methods. (B) The oxyhemoglobin assay. Purified RBCs from venous blood were placed in a reservoir separated from circulating oxyhemoglobin by a dialysis membrane (2.5-3.0 nm [25-30 Å]), inhibiting exchange of RBCs and oxyhemoglobin. In order to measure NO release by NO-dependent conversion of oxyhemoglobin to methemoglobin, time-dependent changes in absorption between 411 nm (isosbestic point) and 401 nm (the highest difference in absorbance) were determined via difference spectrophotometric analysis.24 Buffer (control), l-arginine (l-arg), and l-NMMA were applied subsequently to the system. Arrows indicate the duration of infusion of the respective agents. l-arginine led to an increase of NO release from 0.6 to 14 pmol/mL/min. Inhibition with l-NMMA reduced NO release to 1.4 pmol/mL/min. (C) The nonreductive CLD. Purified RBCs from venous blood were reconstituted with buffer (control) and placed into a reaction chamber flowed with helium (to avoid excessive foaming, antifoaming reagent was added and the Hct diluted to 0.08 [8%]). Time-dependent NO release in the presence or absence of l-arginine or l-NMMA was detected directly in the gas phase (calculated to mL whole blood per measurement period). (D-F) Changes in accumulated plasma RXNO, nitrite, and nitrate were determined in blood samples after incubation with l-arginine (stimulation) and l-NNA (inhibition). Changes were compared with control conditions (incubation with PBS). * indicates significant difference from control; and #, difference from l-arg, P less than .05.
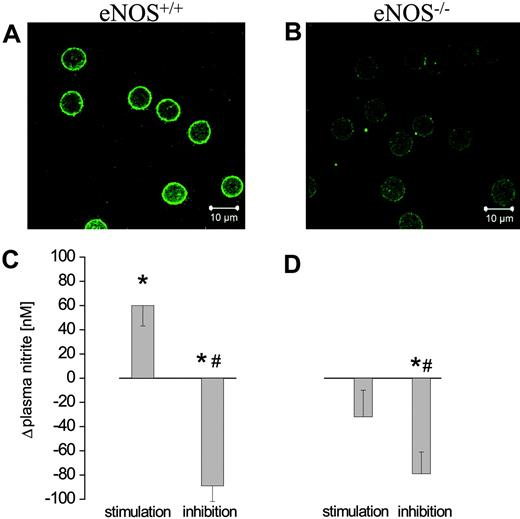
To further characterize the isoform of functional RBC-NOS and to confirm the data obtained in humans we studied eNOS activity and protein in RBCs from WT and eNOS-/- mice. In comparison to WT mice (Figure 7A), RBCs obtained from eNOS-/- mice (Figure 7B) did not show any immunofluorescence signal. Incubation of RBCs from WT mice with l-arginine increased the plasma nitrite concentration, which was completely prevented by NOS inhibition (Figure 7C). In contrast, RBCs obtained from eNOS-/- mice were devoid of NOS activity (Figure 7D).
Discussion
The key novel findings are that an eNOS-like protein is localized in the cytoplasm leaflet and in the cytoplasm with activity and regulatory mechanisms resembling those of endothelium-derived eNOS, serving essential regulatory functions for RBC deformability and platelet aggregation.
Nature of RBC NO synthase
Previous data pointed toward the possibility that RBCs might carry NOS protein,9,10,41,42 being either a NOS2 or NOS3 isoform.43 With NOS being present in RBCs, these studies failed to demonstrate NOS activity, suggesting either an unspecific antibody binding or, in case a NOS protein was present, that the NOS was inactive. In contrast, NO formation was demonstrated in fractionated RBCs.41 No differentiation between enzymatic and nonenzymatic NO production (eg, the conversion of nitrite to NO by hemoglobin36 or the liberation of NO from S-nitrosohemoglobin or nitrosylhemoglobin) was made and no evidence for a NOS protein was presented.41 Finally, up to now the origin of NO synthesis within the blood compartment (RBCs vs non-RBCs) could not be determined reliably.9,41,42 Taken together, specific evidence for NOS (protein) and its function have not been shown so far.
Here we report the discovery of a constitutive blood-borne NO synthesis almost exclusively derived from RBCs. Using immunofluorescence confocal microscopy, NOS protein was found in each single RBC, suggesting a significant role of NOS for RBC function and almost ruling out the possibility that RBC-NOS reflects merely a nonfunctional residual protein of RBC maturation.44 Analysis of subcellular localization using ultrathin cryosection electron microscopy and freeze-fracture immunogold label technique revealed NOS protein in the cytosol and in the membrane. Further analysis of membrane topography by additional immunogold labeling for stomatin, a protein specifically restricted to the P-face of the RBC membrane, demonstrated that RBC-NOS is localized only on the internal side of the membrane. Studies have shown that eNOS activity in other cell types depends on the subcellular localization and trafficking between different cellular compartments.5 Our finding, in the present study, of conspicuous gold labeling for eNOS in the plasma membrane and the cytoplasm hints at the possibility of a close functional linkage between the 2 compartments. In addition, the lack of NOS protein and activity in RBCs from eNOS-/- mice in contrast to those from WT mice further supports the presence of an active eNOS isoform in RBCs and confirms results obtained in humans.
Regulation of RBC NO synthase activity
RBC-NOS resembles a variety of specific regulatory pathways of endothelium-derived eNOS, in that it is stereospecifically stimulated by the substrate l-arginine, it is sensitive to common NOS inhibitors, and its activity depends on the intracellular calcium level and the phosphorylation at serine 1177 regulated by the PI3K.37,38,45 Strikingly, the concentration of l-arginine in RBCs is several-fold lower than those in endothelial cells and up to 30% lower than that in plasma.39 RBCs carry important enzymes of l-arginine metabolism, such as arginase degrading the eNOS substrate, dimethylarginine dimethylaminohydrolase (an enzyme metabolizing endogenous NOS inhibitors),46 and cationic amino acid transporters.47 In RBCs pretreated with arginase, only tiny amounts of l-arginine dose-dependently increased RBC-NOS activity. Nearly maximal enzyme activity was detected, supplying l-arginine levels in the physiologic range. Although admittedly speculative, RBCs might fine-tune their NO production via control of substrate availability. Further studies are warranted to assess the potential role of major determinants in blood flow regulation such as shear stress, pH, pO2, and pCO2 on RBC-NOS activity.
Regulation of RBC eNOS activity. eNOS activity in RBCs was measured depending on the availability of substrate (A) and calcium (B) and the level of phosphorylation of eNOS protein (C-D). (A) Changes in accumulated plasma nitrite were determined in blood samples after incubation with increasing concentrations of l-arginine, d-arginine, and l-NNA. Changes were compared with total depletion of l-arginine (achieved by arginase).  indicates physiologic range of l-arginine concentration in human plasma. (B) Effects of Ca-Ionophore or Ca-Ionophore plus EDTA (n = 6) on plasma nitrite levels were determined after incubation of blood samples and compared with control (buffer). Changes in plasma nitrite reflect the sum of the release (due to NOS-dependent NO formation) and the reuptake of nitrite by RBCs. Thus complete inhibition of RBC-NOS by EDTA significantly reduced plasma nitrite compared with control buffer, unmasking the continuous uptake of plasma nitrite by RBCs during incubation period. (C) Challenging RBCs with insulin increased plasma nitrite whereas addition of the PI3K inhibitor wortmannin prevented this increase (n = 6). * indicates significant (P < .05) difference; and **, highly significant (P < .001) differences from control. (D) Phosphorylation of eNOS at Ser1177 was used to examine the phosphorylation-dependent activation status of the eNOS. RBCs incubated with insulin showed a significant rise of eNOS phosphorylated at Ser1177 compared with control (P < .05; n = 8). Bars, 10 μm.
indicates physiologic range of l-arginine concentration in human plasma. (B) Effects of Ca-Ionophore or Ca-Ionophore plus EDTA (n = 6) on plasma nitrite levels were determined after incubation of blood samples and compared with control (buffer). Changes in plasma nitrite reflect the sum of the release (due to NOS-dependent NO formation) and the reuptake of nitrite by RBCs. Thus complete inhibition of RBC-NOS by EDTA significantly reduced plasma nitrite compared with control buffer, unmasking the continuous uptake of plasma nitrite by RBCs during incubation period. (C) Challenging RBCs with insulin increased plasma nitrite whereas addition of the PI3K inhibitor wortmannin prevented this increase (n = 6). * indicates significant (P < .05) difference; and **, highly significant (P < .001) differences from control. (D) Phosphorylation of eNOS at Ser1177 was used to examine the phosphorylation-dependent activation status of the eNOS. RBCs incubated with insulin showed a significant rise of eNOS phosphorylated at Ser1177 compared with control (P < .05; n = 8). Bars, 10 μm.
Regulation of RBC eNOS activity. eNOS activity in RBCs was measured depending on the availability of substrate (A) and calcium (B) and the level of phosphorylation of eNOS protein (C-D). (A) Changes in accumulated plasma nitrite were determined in blood samples after incubation with increasing concentrations of l-arginine, d-arginine, and l-NNA. Changes were compared with total depletion of l-arginine (achieved by arginase).  indicates physiologic range of l-arginine concentration in human plasma. (B) Effects of Ca-Ionophore or Ca-Ionophore plus EDTA (n = 6) on plasma nitrite levels were determined after incubation of blood samples and compared with control (buffer). Changes in plasma nitrite reflect the sum of the release (due to NOS-dependent NO formation) and the reuptake of nitrite by RBCs. Thus complete inhibition of RBC-NOS by EDTA significantly reduced plasma nitrite compared with control buffer, unmasking the continuous uptake of plasma nitrite by RBCs during incubation period. (C) Challenging RBCs with insulin increased plasma nitrite whereas addition of the PI3K inhibitor wortmannin prevented this increase (n = 6). * indicates significant (P < .05) difference; and **, highly significant (P < .001) differences from control. (D) Phosphorylation of eNOS at Ser1177 was used to examine the phosphorylation-dependent activation status of the eNOS. RBCs incubated with insulin showed a significant rise of eNOS phosphorylated at Ser1177 compared with control (P < .05; n = 8). Bars, 10 μm.
indicates physiologic range of l-arginine concentration in human plasma. (B) Effects of Ca-Ionophore or Ca-Ionophore plus EDTA (n = 6) on plasma nitrite levels were determined after incubation of blood samples and compared with control (buffer). Changes in plasma nitrite reflect the sum of the release (due to NOS-dependent NO formation) and the reuptake of nitrite by RBCs. Thus complete inhibition of RBC-NOS by EDTA significantly reduced plasma nitrite compared with control buffer, unmasking the continuous uptake of plasma nitrite by RBCs during incubation period. (C) Challenging RBCs with insulin increased plasma nitrite whereas addition of the PI3K inhibitor wortmannin prevented this increase (n = 6). * indicates significant (P < .05) difference; and **, highly significant (P < .001) differences from control. (D) Phosphorylation of eNOS at Ser1177 was used to examine the phosphorylation-dependent activation status of the eNOS. RBCs incubated with insulin showed a significant rise of eNOS phosphorylated at Ser1177 compared with control (P < .05; n = 8). Bars, 10 μm.
Functional aspects of the RBC-NOS
Due to the high concentration of hemoglobin in RBCs, coupled with the near-diffusion-limited reaction rate of NO with oxyhemoglobin, RBCs have been considered as a major sink for NO.7,8,48,49 Furthermore, the formations of S-nitrosohemoglobin and nitrosylhemoglobin have been considered as conservers of NO bioactivity transported within RBCs.50,51 Recent reports suggest that the consumption of NO by RBCs in vivo is several orders of magnitude slower than the mere in vitro reaction kinetics between oxyhemoglobin and NO would predict.52 Fluid-dynamic parameters and intravascular flow,53 an unstirred layer of plasma surrounding RBCs,54-56 the unique characteristics of the RBC membrane,53,57,58 and the relatively lipophilic nature of NO59 have been suggested to represent an intrinsic barrier of RBCs to consume NO. More recently it has been demonstrated that hemoglobin reduces nitrite to NO and dilates detector vessels in an oxygen-sensitive manner.36,60,61 In light of our findings, these reports raise several important questions. Is NOS-dependent NO formation sufficient to affect RBC function? Is NO or a yet unidentified NO-related species released from RBCs, and if so is this NO-related species bioactive? How does it get out of the cell?
We observed a RBC-NOS-dependent increase in extracellular nitrate, nitrite, RXNO, and free NO. Nitrate is the stable oxidative end product of NO metabolism in blood. The level of plasma nitrite reflects the sum of a NOS-dependent formation of NO subsequently oxidized to nitrite counterbalanced by the rapid uptake of plasma nitrite into RBCs. RXNO determined by reductive CLD may comprise NO itself, nitros(yl)ated NO adducts, HNO2, N2O3, nitrated lipids, or yet unidentified species.62 The mechanisms of transit of these species from the cytosol or the inner side of the membrane of the RBC into plasma remain to be clarified. Using the oxyhemoglobin assay and the nonreductive CLD, we measured a NOS-dependent release of NO itself from RBCs. Although most of the NO produced by RBCs might possibly be consumed by hemoglobin, the release of NO and bioactive NO-related species may substantially increase the local NO concentration at the immediate vicinity of the membrane, thus contributing to an intrinsic barrier preventing consumption of NO derived from other sources than RBCs themselves. Intrinsic NOS activity may alter the electromechanical properties of the RBC membrane such that proteins and lipoproteins prevent consumption of NO by RBCs.63 The localization of RBC-NOS at the cytoplasm leaflet may preferentially increase methemoglobin concentration near the internal side of the membrane. Taken together, these mechanisms may additionally alter the gradient of NO-related species across the RBC membrane and their diffusion chemistry, in particular considering the naturally formed hemoglobin-spectrin conjugates at the RBC membrane.64
Therefore, we hypothesized that RBC-NOS-dependent NO formation might alter functional characteristics of RBC membrane. NO donors have been shown to affect membrane fluidity63 and also the deformability of RBCs.65,66 Furthermore, in transgenic mice overexpressing erythropoietin, systemic inhibition of NO synthesis was associated with occlusive RBC accumulation in terminal arterioles and death of all animals within hours.67 These results point to the relevance of RBC deformability for the passage of blood through the microvasculature. We therefore measured RBC deformability in relation to RBC-NOS activity. Inhibition of NO formation by l-NNA drastically reduced deformability of RBCs. This deleterious effect was exaggerated by addition of exogenous oxyhemoglobin, suggesting that not only the continuous formation of NO determines membrane deformability but also NO-related intermediates resident within the membrane. It has to be kept in mind that hemoglobin itself may affect membrane function. The impairment of RBC deformability via scavenging of RBC-derived NO may explain the deleterious effects of blood substitutes containing free hemoglobin and also the microcirculatory damage observed in sickle cell patients during hemolytic crises.68,69 NO availability is crucial in patients with sickle cell disease,68 and modification of the circulating NO pool by inhaled NO or l-arginine exerts beneficial effects in acute vaso-occlusive crises and pulmonary hypertension.69,70 In line with these reports, l-arginine improved RBC deformability in our ex vivo experiments, although extrapolation of in vitro data to the in vivo situation should be done with caution.
Functional effects of RBC-derived NO. (A) Flow rate of RBCs through a microfilter after incubation of whole blood with l-arginine, l-NNA, and, in addition, oxyhemoglobin (oxyHb) was taken as a measure of RBC membrane deformability (n = 7). l-arginine (l-arg) increased deformability of RBCs, whereas inhibition of NOS drastically decreased deformability. Removal of bioactive NO through the addition of oxyhemoglobin further reduced deformability. (B) Phosphorylation of platelet VASP was induced by a functional RBC-NOS. Western blot of VASP phosphorylation in the presence of the phosphodiesterase-5 inhibitor sildenafil was observed when whole blood was incubated with l-arginine (P < .05). (C) Changes in ADP-induced platelet aggregation were measured after incubation of whole blood with either l-arginine, l-NNA, or buffer (PBS) and subsequent centrifugation of platelet-rich plasma shown as original registration (inset, summarized data). RBC-derived NO induced by l-arginine significantly decreased platelet aggregation (n = 3), which was prevented by NOS inhibition with l-NNA. l-arginine inhibited aggregation of platelets only in the presence of RBCs. (A, C) *Significant difference from control. #Significant difference from l-NNA.
Functional effects of RBC-derived NO. (A) Flow rate of RBCs through a microfilter after incubation of whole blood with l-arginine, l-NNA, and, in addition, oxyhemoglobin (oxyHb) was taken as a measure of RBC membrane deformability (n = 7). l-arginine (l-arg) increased deformability of RBCs, whereas inhibition of NOS drastically decreased deformability. Removal of bioactive NO through the addition of oxyhemoglobin further reduced deformability. (B) Phosphorylation of platelet VASP was induced by a functional RBC-NOS. Western blot of VASP phosphorylation in the presence of the phosphodiesterase-5 inhibitor sildenafil was observed when whole blood was incubated with l-arginine (P < .05). (C) Changes in ADP-induced platelet aggregation were measured after incubation of whole blood with either l-arginine, l-NNA, or buffer (PBS) and subsequent centrifugation of platelet-rich plasma shown as original registration (inset, summarized data). RBC-derived NO induced by l-arginine significantly decreased platelet aggregation (n = 3), which was prevented by NOS inhibition with l-NNA. l-arginine inhibited aggregation of platelets only in the presence of RBCs. (A, C) *Significant difference from control. #Significant difference from l-NNA.
Proof of eNOS-type NOS in a transgenic mouse model. (A) RBCs in blood samples from WT mice exhibited positive staining for eNOS. (B) Negative staining of RBCs was observed in blood samples derived from eNOS-/- mice (n = 3). l-arginine-induced changes in accumulated nitrite concentration in blood confirm the activity of (C) RBC-NOS in WT mice but not in (D) eNOS-/- mice. *Significant difference from control. #Significant difference from l-NNA.
Proof of eNOS-type NOS in a transgenic mouse model. (A) RBCs in blood samples from WT mice exhibited positive staining for eNOS. (B) Negative staining of RBCs was observed in blood samples derived from eNOS-/- mice (n = 3). l-arginine-induced changes in accumulated nitrite concentration in blood confirm the activity of (C) RBC-NOS in WT mice but not in (D) eNOS-/- mice. *Significant difference from control. #Significant difference from l-NNA.
Stimulated by our analytical findings that NO, and possibly other NO-related species, are released from RBCs and that plasma levels of RXNO increase after challenging RBCs with l-arginine, we studied the effects of RBC-NOS on platelet function. Stimulating RBC-NOS activity suppresses platelet activation and aggregation, whereas NOS inhibition increased platelet aggregation. The RBC-NOS-dependent modulation of platelet function may be mediated by NO itself or by NO-related intermediates such as plasma nitroso compounds, which have been shown to suppress platelet activation.71,72
To estimate the relative proportion of RBCs and endothelia to NO formation we obtained data with the citrulline assay, quantifying the conversion of l-arginine to l-citrulline. This may reflect more precisely the total rate of NOS-dependent NO formation in RBCs compared with a mass analysis of all oxidative and nitros(yl)ated NO metabolites released into plasma. Measurement of NO-related species in plasma does not consider the substantial rate of reuptake into RBCs of some of these metabolites and their conversion into each other within RBCs. Strikingly, the eNOS activity was comparable in both cell types: 0.3 pmol/pg/min for RBCs and 0.7 pmol/pg/min for endothelial cells. Apart from a similar NOS activity, the total protein content of both cell types is also comparable in human beings: 1.1 kg protein in RBCs and 1.5 kg protein in endothelial cells (adult man with 70 kg body weight). Nevertheless, these theoretical considerations cannot simply be extrapolated to the in vivo situation because NO formation by RBCs and endothelial cells as well as the uptake and consumption of NO-related species may vary considerably along the vascular tree.
Future directions
Apart from the vascular endothelium, RBCs have now been identified as a vascular source of NOS-dependent NO formation. Both endothelia and RBCs substantially contribute to the circulating NO pool. Heart failure and atherosclerosis are associated with endothelial dysfunction and reduced NO bioactivity. Our findings may provide a rationale for recent observations that anemia worsens the prognosis in heart failure and myocardial infarction,73 since in those patients reduction of endothelium-derived and RBC-derived NO synthesis occurs. Further elucidation of the regulatory mechanisms of RBC-derived NO formation is required. New diagnostic approaches to reliably quantify eNOS expression in RBCs and to measure the circulating NO pool may allow us to identify patients with NO deficiency and to target new strategies to enhance expression and activity of RBC NO synthase. This may be relevant not only to atherosclerotic diseases but also to hematologic and infectious disorders.74
Prepublished online as Blood First Edition Paper, December 20, 2005; DOI 10.1182/blood-2005-10-3992.
Supported by the Deutsche Forschungsgemeinschaft, Sonderforschungsbereich 612 (M.K.) and 492 (H.R.).
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The indispensable technical assistance of Mrs D. Herzfeld, G. Schoder, S. Matern, K. Schlattmann, and C. Köppler is gratefully acknowledged.

![Figure 3. Evidence of eNOS expression in RBCs. (A) Western blot analysis revealed an eNOS-specific band at 140 kDa in preparations of RBCs (lanes 2 and 3 are derived from diluted preparations [Hct 20%, 10%, and 5%, respectively; with 15, 7.5, and 3.8 μg protein/lane]). This band is equivalent to positive controls of human aortic endothelial cells (HAECs; 2 μg protein/line) and myocardium (cell lysate; 1 μg protein/line). (B) The 450-bp fragment of eNOS mRNA from RBCs corresponds to the control of HUVECs and whole blood. The purity of the RBC fraction was confirmed by mRNA amplification of reference proteins: endoglin for HUVECs, β-globin for RBCs, β-3 integrin for platelets, and CD45 for WBCs. Whole blood was taken as positive control.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/107/7/10.1182_blood-2005-10-3992/5/m_zh80070693530003.jpeg?Expires=1769095003&Signature=HMj9oLcxRvFlCfreWygVO1zYfbKd1qSe8wnSHRtK6qEIM2BB2e2-M6n9ivOm5RDu-GkelfkR8yYVuTBMLiw7xQRZAaxVT6gOru377Fu7ad1KIclz82DSlCD4R0qRCAEFUhWPwoi~APpdZoDQTKnYMiEf8fkrbhwbnmCT6VeAG4tLQmmTvT7KaCyvwN3nW464PszztpMu9LmDTreorhkMsvJ3I-7aeMg5mhx1FtJs4EUBEkknx7Jswm3IUc4DKRHoyTFE8jpuequIrtXFs8yi~VnBw2JLtGbJ~F4~Pz0sAVtY3FNeNdVHSZTt6bIuiRo2~CIakl~T4xsHq4dDnFiRbg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 4. Evidence of NOS activity in RBCs. (A) NOS activity was detected by enzymatic conversion of l-arginine23 in RBC membranes derived from human blood samples (n = 4). (B-C) RBC-NOS-dependent rate of NO release was measured with 2 independent methods. (B) The oxyhemoglobin assay. Purified RBCs from venous blood were placed in a reservoir separated from circulating oxyhemoglobin by a dialysis membrane (2.5-3.0 nm [25-30 Å]), inhibiting exchange of RBCs and oxyhemoglobin. In order to measure NO release by NO-dependent conversion of oxyhemoglobin to methemoglobin, time-dependent changes in absorption between 411 nm (isosbestic point) and 401 nm (the highest difference in absorbance) were determined via difference spectrophotometric analysis.24 Buffer (control), l-arginine (l-arg), and l-NMMA were applied subsequently to the system. Arrows indicate the duration of infusion of the respective agents. l-arginine led to an increase of NO release from 0.6 to 14 pmol/mL/min. Inhibition with l-NMMA reduced NO release to 1.4 pmol/mL/min. (C) The nonreductive CLD. Purified RBCs from venous blood were reconstituted with buffer (control) and placed into a reaction chamber flowed with helium (to avoid excessive foaming, antifoaming reagent was added and the Hct diluted to 0.08 [8%]). Time-dependent NO release in the presence or absence of l-arginine or l-NMMA was detected directly in the gas phase (calculated to mL whole blood per measurement period). (D-F) Changes in accumulated plasma RXNO, nitrite, and nitrate were determined in blood samples after incubation with l-arginine (stimulation) and l-NNA (inhibition). Changes were compared with control conditions (incubation with PBS). * indicates significant difference from control; and #, difference from l-arg, P less than .05.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/107/7/10.1182_blood-2005-10-3992/5/m_zh80070693530004.jpeg?Expires=1769095003&Signature=IOk129ejZTLUvctOmnHLrYhJuWWBxzfxuZdmh442wjClti0RTb-KxcR42Ty9JJckerl4S2fSCNkHCDKA1La9byZjKaMpPJs9C5FL3OPo0zzw8Hlplng-rFc-rA5JgS9VS74ccavx8uQv4KIgW8ehIov-LOCWMo~MOIuTBxGZDNInD0ZeVVKf2HZy5oE6KF5EGIprx3Jiimo2zVtrf7weuvWBy1z5THdUGtBismhv6YB5rWyc8cQX65pJBtvJ~LFhHUEcKpj6K7ZfRRjZLNEN4MG0tI6qgzMIwFjaR8OIsd1UNxzy8QzlNFHCx3dhqenXw8Mjx~V8Iby5WuZ6ERwMtA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal