Comment on Westerhuis et al, page 2215
New data suggest that a mild preparative regimen of antibodies that block CD40 ligand and deplete host NK cells may make allogeneic hematopoietic stem cell transplants safe, establish long-term immunologic tolerance, and broaden the applicability of cord blood as a source of stem cells by making engraftment more efficient.
In Greek mythology, “chimera,” derived from the Greek word for “billy goat,” referred to a fire-breathing she-demon that was part lion, part goat, and part dragon or snake. Getting rid of this killer was quite an achievement, and Bellerophon was heaped with praise and riches for his courageous and clever dispatch of the beast. The term “chimera” has come down to us through the ages with 3 definitions: the original monster, an impossible and fanciful creation of the imagination (eg, Woody Allen's malefactor with the body of a crab and the head of social worker), and an organism containing tissues from at least 2 genetically distinct parents. It is this last definition that is of compelling medical interest, based largely on the work of Ray Owen.
In 1945, Dr Owen was the first to demonstrate immunologic chimerism, when he found that the majority of dizygotic bovine twins had identical blood types.1 This chimerism was thought to result from blood (and, by inference, hematopoietic stem cell) mixing through placental vascular anastomoses. The implied immunologic tolerance associated with the condition was formally documented in 1952 by Billingham et al,2 who showed that dizygotic chimeric twin cattle were tolerant to skin grafts from each other but rapidly rejected third-party grafts.
Chimerism and its associated immunologic tolerance are easy to induce in fetuses and neonates but difficult to induce in adults with their own immunologic integrity. Many barriers exist to engraftment of donor lymphoid and hematopoietic tissues in adult hosts, but most of these barriers can be overcome by eliminating or greatly suppressing host immune defenses. Clinically, this elimination is usually accomplished by a cytotoxic preparative regimen that usually involves drugs but occasionally also uses radiation therapy. However, these regimens generally do not eliminate natural killer (NK) cells or NK activity. The more recent exploration of nonmyelosuppressive preparative regimens has chiefly sought to block the host T-cell response but has largely ignored NK activity. But since the work of Gustavo Cudkowicz (see, for example, Cudkowicz and Stimpfling3 ) in the 1960s, we have known that donor marrow can be rejected even in the face of major histocompatibility complex (MHC) compatibility, and subsequent work from many groups has confirmed a role for NK cells in this process.
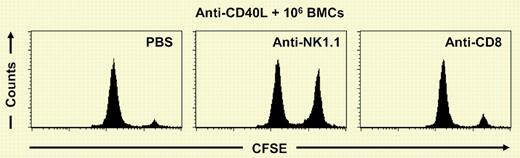
In this issue of Blood, Westerhuis and colleagues demonstrate that immunologic tolerance across a major histocompatibility barrier associated with immunologic chimerism is greatly facilitated by depleting host NK cells, in this case with anti-NK1.1 monoclonal antibody (see figure). In the experiment shown here, C57BL6 mice were treated with anti-CD40 ligand antibody (anti-CD154) and given 1 million allogeneic BALB/c bone marrow cells on day 0. At days 23 and 27, mice received either phosphate-buffered saline (PBS), anti-NK1.1 to deplete NK cells, or anti-CD8 to deplete cytotoxic T cells. On day 28, a novel in vivo cytotoxicity assay was performed in which 10 million BALB/c donor splenocytes labeled with carboxyfluorescein succinimidyl ester (CFSE) were administered to the mice intravenously, and the elimination of the cells by the host was followed by flow cytometry on peripheral blood samples 2 days later. The results demonstrate that NK cells mediate elimination of 94% of the donor cells after anti-CD40 ligand antibody is used as a nonmyelosuppressive preparative regimen for allogeneic transplantation. The rejection of donor type cells is largely prevented by depleting NK cells. In other experiments, adding NK cell depletion to the preparative regimen enhanced allogeneic bone marrow donor cells' ability to establish stable chimerism by at least 3-fold. Without NK cell depletion, an inoculum of 30 million BALB/c marrow cells established donor chimerism in only one of 5 C57BL6 mice; with NK cell depletion, the same dose of donor cells was 100% effective at establishing long-term donor chimerism.
NK cells mediate the elimination of donor cells after anti-CD40L mAb treatment.
NK cells mediate the elimination of donor cells after anti-CD40L mAb treatment.
This paper is important because it focuses again on the NK cell as an important barrier in establishing chimerism and immunologic tolerance. Early work demonstrated that host NK depletion facilitated engraftment and hematologic recovery in both syngeneic and allogeneic bone marrow transplants.4 This paper joins others that have supported the idea that NK cells may be important targets for allograft engineering. It would seem that the time has come for a clinical test of the hypothesis that host NK cell depletion can enhance donor marrow cell engraftment. Given the magnitude of the effect of NK depletion reported here, if the result were verified in humans, important applications would include nonmyelosuppressive allogeneic transplantation and cord blood transplantation. In both settings, the capacity to permit complete hematopoietic engraftment with lower doses of donor cells might permit safe allogeneic transplants with a lower incidence of graft-versus-host disease. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal