Abstract
Adult chronic immune thrombocytopenic purpura (ITP) is an autoimmune disorder manifested by thrombocytopenia from the effects of antiplatelet autoantibodies and T lymphocyte–mediated platelet cytotoxicity. Multiple studies show that corticosteroid treatment and splenectomy, alone or together, increase platelet counts to safe levels in 60% to 70% of patients. However, there is little information on the outcomes of ITP patients refractory to splenectomy. We studied 114 patients with ITP for whom splenectomy failed and who required additional therapy; long-term follow-up was available on 105 (92%) patients. Seventy-five (71.4%) patients attained stable partial (platelet count greater than 30 × 109/L) or complete (normal platelet count) remission; 51 patients remained in remission after therapy was discontinued, whereas 24 patients required continued treatment. Median time to remission after splenectomy failure was 46 months (range, 1-437 months). Median remission durations were 60 months (range, 10-212 months) for patients off therapy and 48 months (range, 2-167 months) for patients on therapy. Thirty (29.6%) patients remained unresponsive to treatment. Thirty-two patients died, 17 (15.7%) of ITP (bleeding, 11 patients; therapy complications, 6 patients) and 15 (13.9%) of unrelated causes. We conclude that most patients with refractory ITP attain stable remission, though on average this occurs slowly. However, a subpopulation with severe, resistant disease experiences significant morbidity and mortality.
Introduction
Adult chronic immune thrombocytopenic purpura (ITP) is an autoimmune disorder characterized by platelet destruction caused by autoantibodies.1-3 Recent studies suggest that antibody-induced suppression of thrombopoiesis4,5 and T lymphocyte–mediated platelet cytotoxicity6 may also be involved in disease pathogenesis. Initially, most ITP patients are treated with corticosteroids; if no lasting response occurs, they undergo splenectomy. This initial approach results in a stable response in 60% to 70% of ITP patients.
Several large studies with substantial follow-up evaluate the responses of adult patients with chronic ITP to corticosteroid therapy and to splenectomy, alone or in combination.7-16 Little information is available on ITP patients unresponsive to splenectomy. The present study describes the long-term outcomes of 105 adults with chronic ITP for whom splenectomy failed and who required additional therapy. Where appropriate, results are compared with those of adult patients with chronic ITP who did not undergo splenectomy or who attained a stable complete or partial remission after surgery.
Patients, materials, and methods
The institutional human subjects review boards of the Scripps Clinic, Scripps Green Hospital, and the Scripps Research Institute approved this study.
Patient population
Between January 3, 1986 and April 1, 1998, we prospectively studied antiplatelet autoantibodies of 114 patients, aged 14 and older, with adult chronic ITP who were refractory to splenectomy. As a comparator group, we evaluated 172 patients with adult chronic ITP who did not undergo splenectomy or who had stable complete remission (CR) (normal platelet count) or partial remission (PR) (platelet count greater than 30 × 109/L) after splenectomy. All patients met the diagnostic criteria advised by the American Society of Hematology Practice Guidelines.17
Refractory chronic ITP. All patients with refractory chronic ITP (RefITP) did not respond to splenectomy (platelet count after splenectomy either did not reach 30 × 109/L or, after an initial increase, fell below 30 × 109/L) and required additional therapy for symptomatic thrombocytopenia. Of the 114 patients in this group, long-term clinical follow-up data were obtained on 105 patients; 9 patients were lost to follow-up.
Other chronic ITP patients. Patients with other types of chronic ITP (OtherITP) consisted of 55 patients who had stable remission after surgery and 117 patients who did not undergo splenectomy, either because it was not clinically indicated (114 patients), the patient refused surgery (2 patients), or the patient was not a surgery candidate (1 patient). Clinical follow-up was obtained on 45 and 95 patients, respectively.
Definitions
Time to splenectomy indicates months between the date of diagnosis and the date of splenectomy. Time to splenectomy failure indicates months between the date of splenectomy and a decrease in the platelet count to less than 30 × 109/L. Follow-up time indicates months between the date of splenectomy and the date of last follow-up (RefITP) or the date of diagnosis and the date of last follow-up (OtherITP). Response to therapy indicates CR or increase in the platelet count to normal; PR or increase in the platelet count to more than 30 × 109/L; or no response or no change in the platelet count or an increase to less than 30 × 109/L. A response was considered stable if it persisted for more than 2 months. Response duration indicates months between the date of CR or PR and the last follow-up. Response durations are recorded as either on therapy (continued treatment was required to maintain a stable response) or off therapy (discontinuation of all ITP treatment). Response groups indicates arbitrarily defined treatment response groups according to the degree of toxicity associated with the therapies, as follows: group 0, spontaneous remission or remission of uncertain origin; group 1, response to corticosteroids, danazol, colchicine, dapsone, or combinations of these agents; group 2, response to oral cyclophosphamide, azathioprine, cyclosporine, or mycophenolate-mofetil; group 3, response to high-dose cyclophosphamide or combination chemotherapy; group 4, no response. Cause of death indicates 1 of 3 groups: ITP—death caused by bleeding resulting from thrombocytopenia; ITP Rx—death caused by ITP treatment complications; other—death from a cause unrelated to ITP.
Statistics
Comparisons between the 2 ITP patient groups were performed by analyzing contingency tables using Fisher exact test (GraphPad Prism Software, San Diego, CA).
Results
Certain data are available on all patients, but other data are available on only a portion of the patients. For each result category, the number of patients involved is shown in parentheses following the category.
Demographics of the ITP patients
For RefITP patients, median age at diagnosis (mean ± SD) was 37 years (42.0 ± 18.4 years), and the sex distribution was 41 men and 73 women. For OtherITP patients, the values were 43 years (47.0 ± 19.3 years) and 54 men and 118 women.
Time to splenectomy
For 105 RefITP patients, time from diagnosis to splenectomy was less than 1 month (31 patients), 1 to 3 months (24 patients), 3 to 6 months (16 patients), 6 to 12 months (5 patients), 1 to 2 years (15 patients), 2 to 5 years (9 patients), 5 to 10 years (4 patients), and more than 10 years (1 patient).
Time to relapse after splenectomy
Among 98 RefITP patients, no response to splenectomy was noted in 23 patients. The remaining patients had relapses after splenectomy at less than 1 month (19 patients), 1 to 3 months (28 patients), 3 to 6 months (6 patients), 6 to 12 months (7 patients), 1 to 5 years (10 patients), 5 to 10 years (4 patients), and more than 10 years (1 patient).
Additional evidence for autoimmunity
Other autoimmune disorders. RefITP patients had higher incidences of other autoimmune disorders than OtherITP patients (P = .001), as follows: 36 of 114 RefITP patients had—thyroid disease (17 patients), autoimmune hemolytic anemia (AIHA) (12 patients), immune neutropenia (2 patients), myasthenia gravis (2 patients), ulcerative colitis (1 patient), AIHA and thyroid disease (1 patient), and AIHA and antiphospholipid syndrome (APL) (1 patient); 25 of 172 OtherITP patients had—thyroid disease (17 patients), AIHA (2 patients), immune neutropenia (1 patient), ulcerative colitis (1 patient), immune lung disease (1 patient), APL (1 patient), and psoriasis (2 patients). This higher incidence was primarily attributed to the increased frequency of autoimmune hemolytic anemia in the RefITP patient group (12 patients compared with 2 patients; P = .004). There was no pattern for the onset of the other autoimmune diseases. Approximately one third occurred before, one third after, and one third concurrently with ITP.
Antinuclear antibody. Positive results of antinuclear antibody (ANA) tests were common in both ITP groups and were not significantly different. Positive assays were noted in 44 of 98 RefITP patients and in 43 of 100 OtherITP patients (P = .8862).
Patient follow-up
Mean follow-up after splenectomy for 105 RefITP patients was 142.9 months, with a median of 110 months. Ninety-one patients were followed up for more than 4 years; 9 additional patients died during the initial 4 years, but they were observed until their deaths. Mean follow-up for 140 OtherITP patients was 104.3 months, with a median of 92 months.
Overall outcome for RefITP patients after splenectomy failure
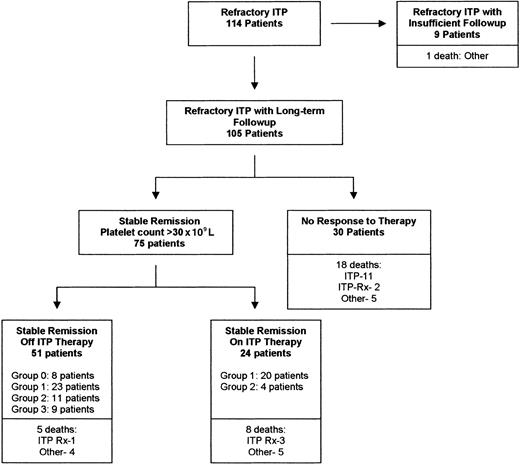
CR or PR.Table 1 and Figure 1 summarize treatment response results. Of 105 patients with RefITP and long-term follow-up, 75 (71.4%) patients attained stable CR or PR. In 51 (48.6%) patients, remission persisted after therapy was discontinued, whereas 24 (22.9%) patients required continued treatment, usually with lowdose corticosteroids or danazol. There was no statistical relationship between the likelihood of attaining stable CR or PR after splenectomy failure and any of the following: patient age (younger than 40 vs older than 40, P = .52; younger than 50 vs older than 50, P = 1.0; younger than 60 vs older than 60, P = .170), time from the diagnosis of ITP to splenectomy (less than 3 months vs more than 3 months, P = .19; less than 6 months vs more than 6 months, P = .18; less than 12 months vs more than 12 months, P = .48), or time from splenectomy to relapse (no response vs temporary response, P = 1.00; less than 1 month vs more than 1 month, P = .25; less than 3 months vs more than 3 months, P = .13; less than 6 months vs more than 6 months, P = .29).
Stable CR or PR in adult ITP patients after splenectomy failure
. | No. patients in CR or PR . | . | . | Time to remission, mo mean/median (range) . | Duration of remission, mo mean/median (range) . | ||
|---|---|---|---|---|---|---|---|
| Treatment group . | On Rx . | Off Rx . | Total . | . | . | ||
| Group 0 | 0 | 8 | 8 | 74/70.5 (3-143) | 86.6/75.5 (36-191) | ||
| Group 1 | 20 | 23 | 43 | 60.6/37 (1-358) | 66/56 (2-177) | ||
| CS | 10 | 10 | 20 | — | — | ||
| Dn | 1 | 2 | 3 | — | — | ||
| Dn/Pred | 5 | 7 | 12 | — | — | ||
| Dn/Co/Pred | 1 | 0 | 1 | — | — | ||
| Dn/Pred/Vin | 0 | 1 | 1 | — | — | ||
| Dn/Pred/Rit | 1 | 0 | 1 | — | — | ||
| Dn/Co | 0 | 1 | 1 | — | — | ||
| Co | 0 | 2 | 2 | — | — | ||
| Dap | 1 | 0 | 1 | — | — | ||
| IFN/Vin | 1 | 0 | 1 | — | — | ||
| Group 2 | 4 | 11 | 15 | 89.3/70 (11-437) | 52.4/42 (10-212) | ||
| Ctx | 0 | 9 | 9 | — | — | ||
| Az | 1 | 2 | 3 | — | — | ||
| CsA | 3 | 0 | 3 | — | — | ||
| Group 3 | 0 | 9 | 9 | 63.6/34 (19-193) | 51.9/26 (12-176) | ||
| HD-Ctx | 0 | 1 | 1 | — | — | ||
| ComboRx | 0 | 8 | 8 | — | — | ||
| Total | 24 | 51 | 75 | 68.1/46 (1-358) | 64/49 (2-212) | ||
. | No. patients in CR or PR . | . | . | Time to remission, mo mean/median (range) . | Duration of remission, mo mean/median (range) . | ||
|---|---|---|---|---|---|---|---|
| Treatment group . | On Rx . | Off Rx . | Total . | . | . | ||
| Group 0 | 0 | 8 | 8 | 74/70.5 (3-143) | 86.6/75.5 (36-191) | ||
| Group 1 | 20 | 23 | 43 | 60.6/37 (1-358) | 66/56 (2-177) | ||
| CS | 10 | 10 | 20 | — | — | ||
| Dn | 1 | 2 | 3 | — | — | ||
| Dn/Pred | 5 | 7 | 12 | — | — | ||
| Dn/Co/Pred | 1 | 0 | 1 | — | — | ||
| Dn/Pred/Vin | 0 | 1 | 1 | — | — | ||
| Dn/Pred/Rit | 1 | 0 | 1 | — | — | ||
| Dn/Co | 0 | 1 | 1 | — | — | ||
| Co | 0 | 2 | 2 | — | — | ||
| Dap | 1 | 0 | 1 | — | — | ||
| IFN/Vin | 1 | 0 | 1 | — | — | ||
| Group 2 | 4 | 11 | 15 | 89.3/70 (11-437) | 52.4/42 (10-212) | ||
| Ctx | 0 | 9 | 9 | — | — | ||
| Az | 1 | 2 | 3 | — | — | ||
| CsA | 3 | 0 | 3 | — | — | ||
| Group 3 | 0 | 9 | 9 | 63.6/34 (19-193) | 51.9/26 (12-176) | ||
| HD-Ctx | 0 | 1 | 1 | — | — | ||
| ComboRx | 0 | 8 | 8 | — | — | ||
| Total | 24 | 51 | 75 | 68.1/46 (1-358) | 64/49 (2-212) | ||
Patients were arbitrarily divided into treatment groups based on the treatment(s) that resulted in CR or PR. Group 0, spontaneous remission or remission of uncertain origin. Group 1, response to corticosteroids (CS); danazol (Dn) alone or in combination with prednisone (Pred), colchicine (Co), vinblastine (Vin), or rituximab (Rit); colchicine; dapsone (Dap); or vinblastine/interferon (IFN). Group 2, response to oral cyclophosphamide (Ctx); azathioprine (Az), or cyclosporine (CsA) alone or in combination with Pred or mycophenolate-mofetil. Group 3, response to intravenous high-dose cyclophosphamide (HD-Ctx) or combination chemotherapy (ComboRx).
Time to remission refers to time in months from splenectomy to stable CR or PR, either on or off therapy.
Duration of remission refers to time in months during which patients remained in CR or PR, either on or off therapy.
— indicates not determined.
Outcomes of patients with refractory adult chronic ITP. Under the category Stable Remission, the number of patients in each of the treatment groups who achieved remission is listed (group 0, spontaneous or uncertain cause; group 1, corticosteroids, danazol, dapsone, colchicine; group 2, azathioprine, oral cyclophosphamide, cyclosporine, mycophenolate-mofetil; group 3, high-dose cyclophosphamide or combination chemotherapy). Causes of death, as listed, are: ITP, death from thrombocytopenia-induced bleeding; ITP Rx, death related to complications of ITP therapy; other, death from causes unrelated to ITP.
Outcomes of patients with refractory adult chronic ITP. Under the category Stable Remission, the number of patients in each of the treatment groups who achieved remission is listed (group 0, spontaneous or uncertain cause; group 1, corticosteroids, danazol, dapsone, colchicine; group 2, azathioprine, oral cyclophosphamide, cyclosporine, mycophenolate-mofetil; group 3, high-dose cyclophosphamide or combination chemotherapy). Causes of death, as listed, are: ITP, death from thrombocytopenia-induced bleeding; ITP Rx, death related to complications of ITP therapy; other, death from causes unrelated to ITP.
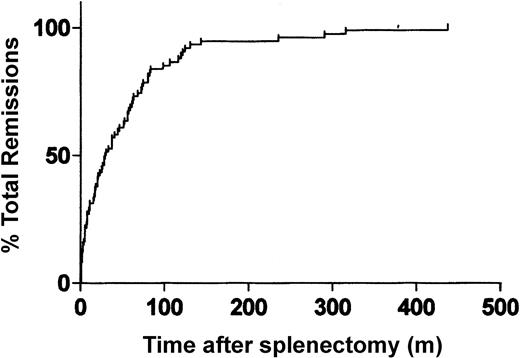
Stable remission after splenectomy failure occurred slowly, with a mean time to remission of 68.1 months (median, 46 months) for the 75 responding patients, though the range was wide (1-437 months) (Figure 2). Times to remission for the individual treatment groups are shown in Table 1.
Time required for adult patients with ITP to attain stable CR or PR after failed splenectomy.
Time required for adult patients with ITP to attain stable CR or PR after failed splenectomy.
Mean duration of stable CR and PR for the total group at the time of last follow-up (Table 1) was 64.2 months (median, 49 months; range, 2-212 months). Remission durations for 51 patients after all ITP therapy was discontinued were 70.5 months (mean), 60 months (median), and 10 to 212 months (range). For the 24 patients on continued ITP therapy, the values were 50.7 months (mean), 48 months (median), and 2 to 167 months (range). Remission durations for the individual treatment groups are shown in Table 1.
No response. Thirty (28.6%) patients were unresponsive to all treatments they received. In this group, 1 patient developed uncontrolled bleeding after splenectomy and died despite highdose corticosteroid therapy and platelet transfusions. Three patients who received corticosteroid therapy after splenectomy without benefit refused further treatment. Their platelet counts were 15 × 109/L to 20 × 109/L, and they had minimal symptoms. The remaining 26 patients received an average of 6.1 (median, 5; range, 3-10) ITP treatments without significant benefit. Eleven patients died of bleeding (“Mortality”), and the remaining patients experienced significant morbidity from ITP and its treatment.
Response to therapy by treatment group
Table 1 and Figure 1 show the responses to therapy by treatment group. Group 0 patients included 1 patient who experienced remission after accessory splenectomy; 2 patients receiving corticosteroids who experienced remission after either the Hong Kong flu or herbal therapy; 3 patients who received corticosteroid therapy for several months and were monitored while they were off therapy (platelet counts less than 30 × 109/L) who experienced remission 9, 10, and 13 years after splenectomy; and 2 patients with severe disease who had received 7 different types of therapy without benefit and who experienced remission 7 and 9 months after their last therapy.
Most patients who achieved CR or PR after splenectomy did so on group 1 drugs. Twenty patients experienced remission after corticosteroid therapy alone, given either continuously (12 patients), as periodic courses (5 patients), or as high-dose pulsed dexamethasone (3 patients). Nineteen patients achieved CR or PR with danazol, given alone (3 patients) or in combination with other drugs (16 patients). Two patients, previously resistant to danazol, became responsive after combination chemotherapy failed. Four patients achieved CR or PR on other group 1 treatments: colchicine (2 patients), dapsone (1 patient), or vinblastine/interferon-γ (1 patient). Group 2 drugs that resulted in CR or PR were azathioprine (3 patients), cyclophosphamide (9 patients), and cyclosporine given alone (1 patient) or with prednisone (1 patient) or mycophenolate-mofetil (1 patient). Nine patients attained CR or PR on group 3 therapy with combination chemotherapy—cyclophosphamide/vincristine/prednisone (CVP), 2 patients; cyclophosphamide/etoposide/prednisone (CEP), 3 patients; cyclophosphamide/ vincristine/prednisone/procarbazine (CMOPP), 1 patient; CMOPP/CEP, 1 patient; and MOPP/adriamycin/bleomycin/vinblastine/dacarbazine (MOPP/ABVD}, 1 patient (given for Hodgkin disease)—or with high-dose cyclophosphamide (50 mg/kg daily for 4 days) (1 patient).
Stable response rates (CR and PR) of patients with refractory ITP to the most common forms of treatment after splenectomy were: corticosteroids, 19.0% (20 of 105 patients); danazol, 33.9% (19 of 56 patients); azathioprine, 15.8% (3 of 19 patients); cyclophosphamide, 25.7% (9 of 35 patients); high-dose cyclophosphamide, 7.1% (1 of 14 patients); and combination chemotherapy, 36.0% (9 of 25 patients). These response rates should be interpreted with caution because the dosages and durations of treatment varied significantly among patients, and sometimes (particularly with danazol) another drug(s) was given concurrently.
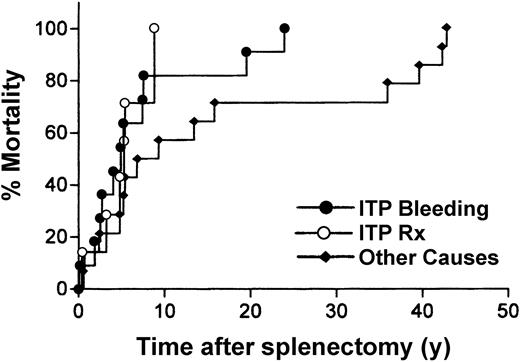
Mortality
RefITP patients. At last follow-up, 76 RefITP patients were alive, and 32 (29.6%) patients had died; the status of the remaining 6 patients is unknown (Figure 1). Figure 3 shows the times from splenectomy until death.
Time from splenectomy to ITP-related death. ITP bleeding, death resulting from thrombocytopenia-induced bleeding; ITP Rx, death resulting from complications attributed to ITP therapy; other causes, death resulting from causes unrelated to ITP.
Time from splenectomy to ITP-related death. ITP bleeding, death resulting from thrombocytopenia-induced bleeding; ITP Rx, death resulting from complications attributed to ITP therapy; other causes, death resulting from causes unrelated to ITP.
ITP. Eleven (10.2%) patients died of bleeding caused by uncontrolled thrombocytopenia, either central nervous system (CNS) bleeding (10 patients) or generalized postoperative bleeding. Mean time from splenectomy to death was 86 months (median, 59 months) and ranged from less than 1 month to 278 months.
Aside from the patient who died of postoperative bleeding, patients who died of bleeding had a similar clinical pattern. Each had undergone an average of 7.2 failed treatment regimens (range, 5-10), and failure was characterized by either no response or a brief response followed by relapse. Each had frequent mucosal bleeding episodes (buccal blisters, epistaxis, vaginal bleeding, gastrointestinal bleeding) that required multiple hospital admissions. Five had 1 or more CNS bleeding episodes before death. Five had severe mucosal bleeding and platelet counts higher than 10 × 109/L, suggesting that their antibodies might have affected platelet function.
ITP therapy. Six (5.6%) deaths were attributed to treatment complications—sepsis associated with immunosuppression and asplenia (3 patients), postoperative pancreatitis and sepsis (1 patient), and transfusion-related hepatitis C with liver failure (2 patients). Mean time from splenectomy to death was 63 months (range, 5-106 months).
Other causes. Fifteen (13.9%) patients died of causes unrelated to ITP. Six died of malignancy (breast cancer, 2 patients; lung cancer, 2 patients; colon cancer, 1 patient; acute granulocytic leukemia (AGL), 1 patient), 7 died of cardiovascular events (cerebrovascular accident, 2 patients; cardiac arrest, 2 patients; congestive heart failure, 1 patient; myocardial infarction, 1 patient; and ruptured aortic aneurysm, 1 patient), 1 died of AIHA, and 1 died of an unknown cause in a nursing home. Mean time from splenectomy until death was 184 months (median, 82 months), with a range of 7 to 508 months. The patient who died of AGL received cyclophosphamide for ITP. It is possible that this agent induced leukemia.
OtherITP patients. No deaths from bleeding occurred in the OtherITP group, and only 1 death was attributed to ITP therapy (pneumonia in a patient with neutropenia who was not a surgery candidate because of age and other medical problems). Fourteen deaths resulted from unrelated causes, and this incidence was not significantly different between the 2 groups (P = .31). When overall mortality for RefITP patients is compared with that of OtherITP patients, the increase is significant (P = .0001)
Other possibly related disorders
Of 104 RefITP patients, 7 acquired other potentially related autoimmune or malignant disorders several years after ITP diagnosis. They were systemic lupus erythematosus (SLE) (2 patients, 11.5 and 14 years later), polymyalgia rheumatica (1 patient, 13 years later), non-Hodgkin lymphoma (2 patients, 5.5 and 24 years later), and Hodgkin disease (2 patients, 7 and 8 years later). In the OtherITP group, 1 patient had SLE 3 years after the ITP diagnosis.
Venous disease
Thirteen patients had evidence of venous thrombosis: 10 patients had deep venous thrombosis (DVT), 2 patients had pulmonary embolus, and 1 patient had thrombosis of her toes that necessitated amputation. DVT was associated with a central line in 2 patients, factor V Leiden in 1 patient, antiphospholipid syndrome in 1 patient, and protein C deficiency in 1 patient. When the incidence of venous disease in ITP patients (105 patients) was compared with the incidence in a population-based study,18 there was a significant increase in the group with venous disease if all 13 patients were included (observed/expected, 3.52; 95% confidence interval [95% CI], 1.87-6.02), but the increase was not significant if the 5 patients with other risk factors were excluded (observed/expected, 2.17; 95% CI, 0.93-4.27).
Discussion
A recent population-based study suggests that adult chronic ITP is a more benign disease than previously suspected, with frequent remissions that occur spontaneously or in response to first-line therapy and with a low requirement for splenectomy.19 Several earlier studies show that approximately 60% to 70% of patients who require therapy respond to corticosteroids or splenectomy.7-16 However, there is little information on the long-term outcomes of patients whose conditions do not improve after splenectomy and who require further treatment.
The present prospective study describes the clinical outcomes of 114 RefITP patients. Long-term (mean, 11.9 years) follow-up data were available on 92% of the patients. Does this study give an exact picture of the long-term outcomes of patients with RefITP? Given that our institution is a tertiary center, it is possible that referral bias affected these results. The ideal study would be a population-based one from a defined medical region. However, such a study would be difficult to conduct because of the extremely large numbers of patients required and the long follow-up involved. For instance, the population-based study described19 enrolled only 30 patients requiring splenectomy over 6 years, and most did not need additional treatment. In any case, because most RefITP patients are managed at tertiary centers, the present data should be useful in anticipating the clinical course of this patient group.
In the present study, RefITP patients were predominantly women whose median age was 37. Other autoimmune diseases were more common in RefITP patients when compared with the OtherITP patient group, primarily because of the increased incidence of AIHA. Most (75 of 105) of these RefITP patients eventually attained stable CR or PR, either spontaneously or after treatment. On average, stable remissions occurred slowly; the median time to remission was approximately 4 years. Approximately two thirds of patients remained in remission after discontinuing all medications, whereas the other one third required continued treatment. Once achieved, remissions were durable; median duration was 49 months at last follow-up.
Conversely, there is a subpopulation of RefITP patients who are extremely resistant to therapy and who have a significantly higher mortality rate from ITP and its treatment (17.6% in this series) than ITP patients who do not require or who respond to surgery. This subpopulation is characterized by chronic severe thrombocytopenia and continuous bleeding problems that necessitate frequent hospitalization and emergency treatment. Cohen et al,20(p1630) in their review of 17 ITP case series, came to a similar conclusion that “idiopathic thrombocytopenic purpura with persistent low platelet counts carries a grave prognosis.”
The only series that is comparable to ours is a single institution study by Bourgeois et al 21 that includes 28 adult RefITP patients who met our criteria (patients who required additional treatment after splenectomy failure). This group also reported a high remission rate (21 of 28 patients), with most stable off therapy. They noted similar mortality from ITP (2 deaths from bleeding) but a lower incidence of patients refractory to therapy (5 of 28).
In our patient group, we also noted 7 patients who had another autoimmune disease (3 patients) or a lymphoid malignancy (4 patients) several years after splenectomy. Whether this reflects a lack of immunoregulation, thought to be associated with autoimmune diseases, or can be attributed to long-term immunosuppression treatment is unknown.
In summary, approximately 75% of patients with RefITP eventually achieved remission, though remission occurred slowly. Patients who did not achieve remission instead experienced an extremely difficult disease course with significant morbidity and mortality. It is possible that newer forms of treatment, such as rituximab, thrombopoietic factors, and monoclonal antibodies affecting key pathways in the immune system, may alter outcomes for this extremely resistant subgroup. New therapeutic approaches are certainly needed.
Prepublished online as Blood First Edition Paper, April 20, 2004; DOI 10.1182/blood-2003-11-3908.
Supported by National Institutes of Health grants HL61809 and M01 RR00833.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank all the physicians, their office staffs, and the patients who helped us obtain follow-up information to make this study possible.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal