Abstract
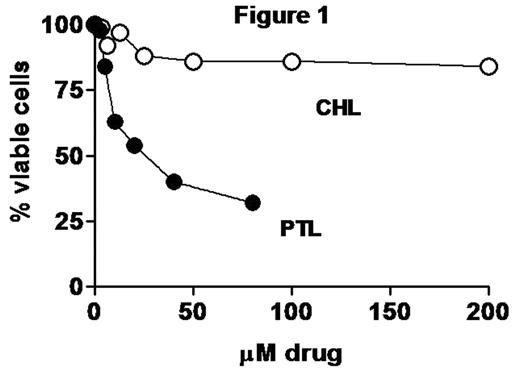
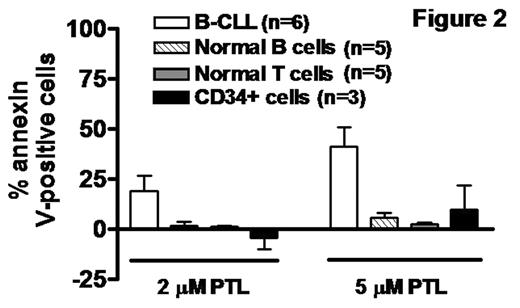
B-chronic lymphocytic leukaemia (CLL) is the most frequent leukaemia in the western world. CLL is incurable using conventional therapy. While the disease is controlled by treatment with chlorambucil (CHL) or fludarabine, extended exposure to these agents results in drug resistance. It is therefore important to identify novel agents which rapidly and selectively induce apoptosis of cells isolated from patients who have become resistant to conventional drugs. The sesquiterpene lactone parthenolide (PTL) is the active component of several medicinal plants which have been used for hundreds of years for the treatment of migraines, pain and inflammatory conditions. In some cell lines, PTL has been shown to block components of the NFκB pathway including the IκB kinase complex and/or the p65 subunit of NFκB. Here we investigated the sensitivity of isolates from 25 CLL patients (representing stages A, B and C) to PTL (1.25–80 μM) and CHL (3.125–200μM). IC50 values were evaluated by the 4,5-dimethylthiazol-2,5-diphenyltetrazolium bromide (MTT) dye reduction assay. Apoptosis induction was quantified by FACScan analysis of annexin V binding and by western blot detection of cleavage of the caspase 3 substrate poly (ADP ribose) polymerase (PARP). CHL resistance varied across the cohort from highly sensitive to highly resistant, with IC50 values in the range 5.3 to >200 μM. In contrast, all isolates tested were sensitive to PTL, with IC50 values in the range 3 to 20 μM. Strikingly, isolates from extensively-treated patients which were highly resistant to elevated levels of CHL in vitro were sensitive to PTL (Figure 1). PTL induced very rapid PARP cleavage which became clearly evident between 3–6 h of exposure to 5 μM PTL. In contrast, PARP cleavage was not detected until >12h exposure to 75 μM CHL in isolates which were sensitive to this drug. Furthermore, pulse/wash-out experiments showed that a very brief (1-2h) exposure to PTL was sufficient to induce commitment to the apoptotic programme. The annexin V-binding assay revealed that CLL cells were strikingly more sensitive to apoptosis induction by 2–5 μM PTL than were normal T or B lymphocytes or CD34+ bone marrow progenitor cells (Figure 2). Western blot analysis revealed that PTL-induced PARP cleavage was preceded by downregulation of anti-apoptotic mcl-1, a key mediator of the survival of B lineage lymphoid cells. However, we failed to detect a PTL-induced decrease in IκBαphosphorylation, suggesting that inhibition of IκB kinase did not contribute to the mechanism of CLL cell killing. In conclusion, the rapid, selective action of PTL and its ability to kill CLL isolates refractory to cytotoxic drugs suggest that this agent may be of value in the treatment of CLL patients who have become resistant to conventional therapeutic regimes.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal