Abstract
We performed a randomized trial to compare the safety and efficacy of itraconazole with fluconazole in preventing fungal infections in patients undergoing allogeneic stem cell transplantation (SCT). Itraconazole (intravenous 200 mg daily, or oral solution 2.5 mg/kg 3 times daily) and fluconazole (intravenous or oral, 400 mg daily) were administered with the start of conditioning therapy, until at least 120 days after SCT. After enrollment of the first 197 patients, a data and safety monitoring board reviewed potential drug-related toxicities. Patients who received itraconazole developed higher serum bilirubin and creatinine values in the first 20 days after SCT, with highest values in patients who received itraconazole concurrent with cyclophosphamide (CY) conditioning. Analysis of CY metabolism in a subset of patients demonstrated higher exposure to toxic metabolites among recipients of itraconazole compared with fluconazole. These data suggest that azole antifungals, through differential inhibition of hepatic cytochrome P-450 isoenzymes, affect CY metabolism and conditioning-related toxicities.
Introduction
Two placebo-controlled trials performed in the early 1990s established the efficacy of high-dose fluconazole (400 mg daily), initiated with the start of conditioning chemotherapy, in preventing candidiasis in patients undergoing stem cell transplantation (SCT).1,2 Because molds have since become prominent pathogens, alternative prophylaxis strategies, using mold-active antifungals such as itraconazole, are being considered.
Itraconazole and fluconazole both inhibit and are metabolized by hepatic cytochrome P-450 isoenzymes. Itraconazole is a potent inhibitor of the P-450 isoenzyme CYP3A4. At high doses (≥ 200 mg), fluconazole can also inhibit CYP3A4, although with less potency.3 Consequently, both drugs can increase levels of CYP3A4-metabolized drugs, such as cyclosporine and benzodiazepines. Fluconazole, but not itraconazole, can also inhibit CYP2C9, resulting in additional interactions with phenytoin and warfarin.3 Fluconazole can inhibit CYP2C19 in vitro, but the clinical significance of this interaction is not known.3
Cyclophosphamide (CY) is an alkylating agent used frequently for myeloablative conditioning therapy prior to SCT. Metabolism is complex; CY is administered as a prodrug that is oxidized within hepatocytes to the active metabolite 4-hydroxycyclophosphamide (HCY) by CYP2B6, 3A4, 2C9, and 2A6.4,5 In the liver, intracellular decomposition of HCY yields a DNA alkylator, phosphoramide mustard, and a toxic metabolite, acrolein. Alternative metabolism of HCY occurs via: (1) cytochrome P-450 detoxification to 4-ketocyclophosphamide (ketoCY); (2) aldehyde dehydrogenase-1 conversion to carboxyethylphosphoramide mustard (CEPM); and (3) glutathione conjugation to glutathionyl-CY.6,7 We have previously shown that CY-containing conditioning-related toxicities, particularly hepatic sinusoidal obstruction syndrome, also known as veno-occlusive disease (VOD), is associated with exposure to high levels of the HCY metabolite, acrolein.7
For many years, our institutional practice has been to coadminister fluconazole with myeloablative conditioning therapy, as was performed in the randomized trials.1,2 Although one can hypothesize that this may alter metabolism of cytochrome P-450–metabolized chemotherapeutic drugs, clinically significant interactions have been recognized for only a few combinations. Specifically, vincristine-induced neurotoxicities, hypertension, and gastrointestinal toxicities have been reported with itraconazole coadministration.8-10 Clinically significant azole interactions with CY have not been appreciated. We describe here toxicities and CY pharmacokinetics in a subset of patients enrolled in a recently completed randomized prophylaxis trial of fluconazole versus itraconazole. Relative differences in early toxicities, uncovered after interim review by a data and safety monitoring board (DSMB), triggered a more detailed investigation of CY metabolism (detailed in this study); overall safety and efficacy analyses after completion of the trial are presented in a separate study.11
Study design
Antifungal prophylaxis trial
In a randomized trial to compare fluconazole with itraconazole for prophylaxis after allogeneic SCT, patients (age ≥ 13 years) were randomized to receive fluconazole (intravenous or oral, 400 mg daily) or itraconazole (intravenous 200 mg daily, or oral 2.5 mg/kg 3 times daily), beginning with the start of conditioning chemotherapy. Patients who required corticosteroids (≥ 1 mg/kg prednisone equivalent) for therapy of graft versus host disease (GVHD) continued study drugs for 180 days, or until development of drug-related toxicities or fungal infection. Myeloablative conditioning and SCT were performed as per standard practice. The most common conditioning regimen was CY (60 mg/kg) and total body irradiation (TBI).7,12 Analysis of the early safety of these 2 regimens was performed by a DSMB after approximately 25% of projected enrollment. The incidence of nephrotoxicities (doubling of baseline serum creatinine concentration) and hepatotoxicities (median daily total bilirubin level) were compared in itraconazole and fluconazole recipients during the first 20 days after SCT. This study was approved by the Fred Hutchinson Cancer Research Center (FHCRC) Institutional Review Board. All patients provided informed consent.
Pharmacokinetics of CY
To examine the hypothesis that early hepatic and renal toxicities observed in fluconazole and itraconazole recipients were related to the impact of the azoles on CY metabolism, we examined data obtained from the subset of patients who were enrolled in a concurrent study on CY metabolism performed at our center between 1997 and 2000.7 As part of this study, CY metabolites were measured from patients who received myeloablative conditioning of CY plus TBI. Briefly, CY and metabolites (4-hydroxy-cyclophosphamide [HCY], O-carboxyethylphosphoramide mustard [CEPM], deschloroethyl-cyclophosphamide [DCCY], 4-keto-cyclophosphamide [ketoCY], and hydroxyprophylphosphoramide mustard [HPPM]) were measured mid-infusion, at the end of infusion, and at 1, 3, 7, 20, and 24 hours after infusion. Exposure to CY metabolites was expressed as the area under the curve (AUC; mM/h) derived from the time of the first CY dose to 24 hours after the second CY dose.7 Comparative data on metabolite exposure was available for 9 patients who received itraconazole as part of the randomized trial, and 140 patients who received fluconazole, both as part of the trial and as standard practice.
Statistical considerations
Continuously valued outcomes were compared using a Wilcoxon rank sum test. Categorical outcomes were compared using χ2 or Fisher exact tests, as appropriate. All reported P values are 2-sided.
Results and discussion
Among 209 patients who received azole antifungals concurrent with conditioning therapy as part of the randomized trial (105 itraconazole and 104 fluconazole), there was a trend to higher average serum bilirubin levels before day 20 in those who received itraconazole compared to fluconazole (medians, 1.49 mg/dL versus 1.32 mg/dL, respectively, P = .09), particularly in those who received CY for conditioning (n = 188; medians, 1.49 mg/mL versus 1.27 mg/mL, respectively, P = .07; Figure 1). There were also more recipients of itraconazole whose baseline creatinine level increased at least 2-fold within the first 20 days of SCT (36 of 105, 34% itraconazole versus 21 of 104, 20% fluconazole, P = .03; Figure 1).
Serum creatinine and serum bilirubin values. Daily (A) serum creatinine (mg/dL) and (B) total serum bilirubin (mg/dL) values for the first 20 days after SCT in patients who received fluconazole and itraconazole concomitant with CY-based conditioning therapy.
Serum creatinine and serum bilirubin values. Daily (A) serum creatinine (mg/dL) and (B) total serum bilirubin (mg/dL) values for the first 20 days after SCT in patients who received fluconazole and itraconazole concomitant with CY-based conditioning therapy.
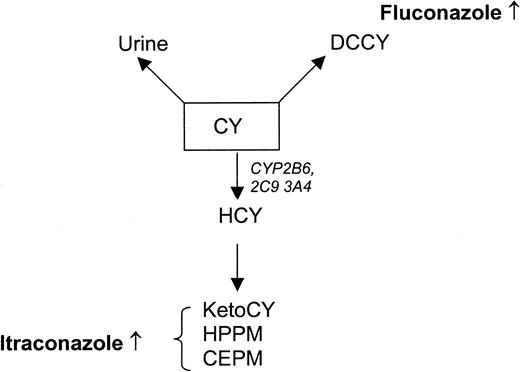
We investigated the hypothesis that early toxicities were associated with altered CY metabolism by quantifying metabolites in the subset of 9 itraconazole and 140 fluconazole patients with available CY metabolism data. Despite the small numbers of patients sampled, strong differences emerged. Patients who received fluconazole had greater exposure to CY (AUC 6198 ± 1229 versus 5077 ± 991, Wilcoxon P = .0065) and DCCY (AUC 615 ± 267 versus 371 ± 148, P = .007); itraconazole recipients had greater exposure to HCY (AUC 231 ± 46 versus 147 ± 59, P < .001) and ketoCY (AUC 348 ± 121 versus 227 ± 88, P < .001). There was a less marked trend to increased CEPM in itraconazole recipients (AUC 472 ± 135 versus 412 ± 188, P = .16). A schematic diagram of CY metabolism and the impact of these azoles is shown in Figure 2.
Schematic of CY metabolism. A fraction of CY is excreted unchanged in urine. The remaining prodrug (CY) is converted to DCCY or oxidized to HCY by CYP2B6, 3A4, and 2C9. HCY is further degraded to alternative metabolites (shown here are ketoCY, HPPM, and CEPM). Relative quantities of metabolites measured in fluconazole and itraconazole recipients are shown.
Schematic of CY metabolism. A fraction of CY is excreted unchanged in urine. The remaining prodrug (CY) is converted to DCCY or oxidized to HCY by CYP2B6, 3A4, and 2C9. HCY is further degraded to alternative metabolites (shown here are ketoCY, HPPM, and CEPM). Relative quantities of metabolites measured in fluconazole and itraconazole recipients are shown.
These data suggest that differential toxicities may be associated with alternative metabolism of CY because toxicities were apparent only in patients who received CY-based conditioning regimens, and quantification of CY metabolites revealed differences in exposure to metabolites previously implicated in sinusoidal obstruction syndrome.7 Because of a limited duration of overlap between the antifungal prophylaxis trial and the CY metabolism study, we had metabolite data available from only a small number of itraconazole recipients. Although this limits definitive conclusions, quantities of CY metabolites were strikingly different. Itraconazole recipients, compared to fluconazole recipients, had approximately 20% increased CY clearance (P = .007), with a resultant increased exposure to HCY (P < .001) and HCY metabolites, ketoCY (P < 0001) and CEPM (although the latter difference was not statistically significant, P = .15). Coordinately, itraconazole recipients had approximately 40% decreased exposure to DCCY (P < .001). The observation that toxicities occurred in patients who had higher exposure to HCY, and its degradation products, is consistent with the results of prior studies that established a link between hepatic sinusoidal injury and acrolein, which is generated by decomposition of HCY after it enters cells as its tautomer aldocyclophosphamide (aldoCY).7
All patients in this study received either fluconazole or itraconazole during CY administration; as such, we lack the true controls that are required to define the precise mechanisms contributing to differences in CY metabolism or toxicities. However, given the known metabolism of the drugs, these observations may be explained by azole inhibition of different P-450 isoenzymes. One possibility is that fluconazole inhibition of CYP2C9 may decrease formation of HCY, resulting in more DCCY exposure and fewer toxic HCY metabolites.13 This would suggest that the difference in toxicities observed between the 2 azoles may be associated with a relative protective effect of fluconazole, through inhibition of HCY formation.
We have found that itraconazole and fluconazole alter metabolism of CY in unique fashions, potentially having impacts on toxicities early after SCT. Further studies are necessary to define mechanisms; however, we believe that these observations are sufficient to encourage caution with coadministration of azole antifungals and cytochrome-metabolized cytotoxic agents.
Prepublished online as Blood First Edition Paper, September 22, 2003; DOI 10.1182/blood-2003-07-2512.
Supported in part by grants from the National Institutes of Health (CA18029, CA15704, and K08AI0571). Partial funds for substudy analyses were provided by Ortho Biotech Products, LP.
K.A.M. has served as a consultant for and received grant funding from Ortho Biotech Products. K.A.M. and M.B. served as consultants for Pfizer.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors gratefully acknowledge the members of the data and safety monitoring board: Drs Paul Martin, Richard Nash, Barry Storer, and Anna Wald.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal