At present there is some controversy about the appropriate appellation “disease” versus “lymphoma” but none about the malignant character of the cells described by Sternberg1 and Reed2 slightly more than 100 years ago. The identity of clonal B cells was masked by lack of expression of immunoglobulins and down-regulation of characteristic B-cell antigens. It now appears that in the subset of Hodgkin lymphoma cases associated with Epstein-Barr virus (EBV), a viral protein may explain both the survival of B-lineage cells without immunoglobulin expression and, as detailed in this issue of Blood, the down-regulation of B-cell antigens.
Hodgkin lymphoma is arguably the first malignancy to have been associated with EBV, for the association with the clinical syndrome of infectious mononucleosis in the anecdotal literature anticipated the discovery of the virus by decades. The discovery of a herpesvirus in endemic Burkitt lymphoma led to the discovery that EBV immortalizes lymphocytes in vitro. Early on it appeared that this capacity might provide the key to understanding this virus' association with malignancy. Investigation of the molecular basis of lymphocyte immortalization in vitro identified a handful of genes with very interesting properties and these genes in aggregate appear to drive some posttransplantation lymphoma. However, many of the viral genes required for lymphocyte immortalization are not expressed in other EBV-associated malignancies. Conversely, genes not required for lymphocyte immortalization may play an important role in the pathogenesis of malignancy.
The latency membrane protein 2A (LMP2A) functions to block B-cell receptor (BCR) activation and signaling with failure to activate downstream signaling molecules. Teleologically speaking, this makes some sense. The B lymphocyte is the virus' home, and having invested in setting up housekeeping, the virus would not be well served if antigens in the environment were masters of the house. However, simply removing the BCR signal does not ensure survival of the infected cell insofar as B cells are programmed to self-destruct in the absence of immunoglobulin signaling. LMP2A circumvents that problem by providing a survival signal. Expression of an LMP2A transgene in a mouse allows B cells lacking immunoglobulin expression to colonize peripheral lymphoid organs.
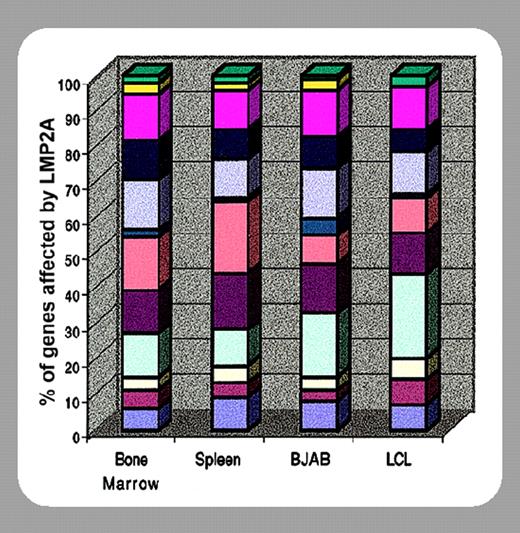
Thus, in Hodgkin lymphoma, the expression of LMP2A protein in B-lineage cells lacking immunoglobulin expression provides circumstantial evidence that the viral gene plays a role in tumor cell survival. In the present paper by Portis and colleagues (page 4166) new evidence is presented that in addition to modulating cell cycle and apoptosis pathways, LMP2A expression may also modulate other aspects of the phenotype of Reed-Sternberg cells, particularly down-regulation of the expression of B-cell–specific factors. Among the important questions looming are why EBV-associated Hodgkin lymphoma develops in only rare patients infected with EBV, how a similar phenotype evolves in the absence of the virus in other cases of Hodgkin lymphoma, and how this knowledge might be applied to prevention or treatment.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal