Placental/umbilical cord blood (PCB) is a source of hematopoietic stem cells for bone marrow reconstitution. Engraftment speed and survival are related to the total nucleated cell (TNC) dose of the graft. This study explored the possible influence on engraftment of nucleated red blood cells (NRBCs) in the graft. Automated hematology analyzers were used to enumerate TNCs. NRBCs were counted by visual examination or by using an automated analyzer. Hematopoietic progenitor cells were enumerated as either colony-forming cells or CD34+ cells. Transplant centers reported on transplant outcome in 1112 patients given PCB grafts through September 2001. NRBCs correlated with progenitor cell numbers. Both white blood cell and NRBC dose were independently predictive of myeloid engraftment speed. Because NRBC dose predicted engraftment speed, inclusion of NRBCs in the TNC count does not reduce the effectiveness of the prefreezing TNC count as an index of the quality of a PCB unit as a graft. The correlation between the number of NRBCs and the number of hematopoietic progenitor cells probably reflects the involvement of early stem cells in erythroid responses.
Introduction
At birth, blood from the umbilical cord and placenta (placental/umbilical cord blood [PCB]) contains sufficient concentrations of hematopoietic stem and progenitor cells to routinely reconstitute ablated bone marrow.1-9 Engraftment speed, overall probability of engraftment, and disease-free survival correlate with the dose of total nucleated cells (TNCs), as well as progenitor cells, per kilogram of the recipient's body weight.6-10However, nucleated red blood cells (NRBCs) can represent a substantial proportion of the TNCs in cord blood. Thus, TNC counts in PCB units offered for transplantation may not accurately represent the white blood cell (WBC) content, which is presumed to be a more accurate measure of engraftment potential than the TNC count. In this study, we investigated the influence on engraftment of the presence of NRBCs in umbilical cord blood.
Study design
Collection of PCB
Since 1993, the Placental Blood Program of the New York Blood Center (NYBC) has collected, tested, processed, and cryopreserved PCB and provided units for transplantation to unrelated recipients.2-4,7,9 10 Approval was obtained from the institutional review board of the New York Blood Center. Informed consent was provided according to the Declaration of Helsinki.
Testing placental blood
Through May 2000, TNCs were enumerated with an H1 hematology analyzer (Technicon Instruments, North Chicago, IL). Thereafter, counts were done with a Sysmex XE-2100 instrument (Roche Diagnostics, Indianapolis, IN), which also enumerated NRBCs. NRBCs were also counted retrospectively, under code, on a smear of placental blood obtained at the time of PCB collection as the number of erythroblasts, proerythroblasts, and cytoplasm-free RBC nuclei per 100 nucleated cells. NRBC and WBC concentrations were then calculated from the respective TNC concentrations.
Hematopoietic colony-forming cells (CFCs) were assayed in a subset of PCB units from the start of the program through March 2000.10 Beginning in January 2000, the absolute number of CD34+ cells was measured in all units using a FACSCalibur flow cytometer and a ProCOUNT progenitor cell–enumeration kit with ProCOUNT software (Becton Dickinson Immunocytometry Systems, San Jose, CA). The hematopoietic progenitor cell subset was contained among a CD34 subset of cells showing intermediate fluorescence intensity (referred to hereafter as CD34+ progenitor cells).11
Patients and transplant study end point
By the end of September 2001, the Placental Blood Program of the NYBC had provided single-unit PCB transplants to 1112 patients (including 562 patients previously reported on).7NRBCs were enumerated manually on slides from all but 2 of 1111 PCB units given to these patients (2 patients shared one large unit and slides from 2 other units were unreadable). The transplant end point of interest for the current analysis was the speed of myeloid engraftment, which was defined as the time to achieve an absolute neutrophil count (ANC) of at least 500/μL.7 Transplant centers reported on the occurrence and timing of myeloid engraftment in 93% of patients.
Statistical analysis
Correlations between NRBCs and other blood or progenitor cells were assessed using the Spearman nonparametric correlation coefficient.12 Time to achieve an ANC of at least 500 was estimated by using the Kaplan-Meier method, as previously reported.7,10,13 In assessing the significance of associations between cell dose and time to engraftment, we used the log-rank statistic with multivariate analyses carried out by using Cox logistic regression under an assumption of proportional hazards (all analyzed variables included in the model).14 All statistical analyses were done with SPSS software (version 10.1; SPSS, Chicago, IL).
Results and discussion
Frequency distribution of NRBCs and relation to TNCs, WBCs, and progenitors
The frequency distribution of NRBCs per microliter approximated a Poisson model. In an ethnically stratified subset of 1200 PCB units (300 each white, African-American, Hispanic, and Asian), the mean NRBC count was 1015/μL (8.4/100 WBCs). The mean NRBC count for transplanted PCB units was somewhat higher (1424/μL). In a subset of 248 PCB units tested by using the Sysmex XE-2100 (Roche Diagnostics, Indianapolis, IN), duplicate instrument counts of NRBCs were highly consistent (R2 = 0.994; P < .001), as was the correlation between triplicate manual counts and instrument counts (R2 = 0.805; P < .001).
NRBC count correlated with TNC count and with WBC count, although not as strongly (R2 = 0.21 and 0.07, respectively;P < .001 for each). NRBC count also correlated with CFC count (R2 = 0.22; P < .001) and CD34+ cell count (R2 = 0.27;P < .001). These relations were stronger than those between WBCs and progenitors (CFCs, R2 = 0.16, and CD34+ cells, R2 = 0.14;P < .001 for both comparisons). NRBC count correlated with granulocyte-macrophage or mixed-cell colony-forming units (R2 = 0.14 and 0.16, respectively;P < .001) but only weakly with the number of erythroid burst-forming units identified in culture (R2 = 0.025;P < .001).
Myeloid engraftment
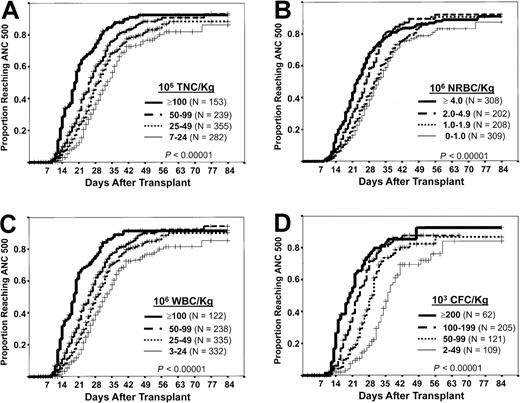
Patient characteristics are shown in Table1. Data on time to reach an ANC of at least 500 were available for 1029 patients: 70% reached this end point, 90% by Kaplan-Meier analysis (80% by day 42 after transplantation). Time to reach an ANC of at least 500 correlated with the dose of TNCs, NRBCs, WBCs, and CFCs per kilogram of body weight (Figures 1A, 1B, 1C, and 1D, respectively). In a multivariate model, both NRBC count and WBC count were significant predictors of the speed of myeloid engraftment (Table2). When CFC dose was included in the model, however, only CFC dose was predictive of engraftment speed (odds ratio [OR], 2.7 [P ≤ .001] for CFC dose ≥ 100 × 103/kg; and OR, 1.8 [P = .003] for CFC dose of 50-99 × 103/kg compared with the lowest dose category). When other factors reported to be related to engraftment speed (diseases associated with poor engraftment, HLA match, methotrexate prophylaxis for graft-versus-host disease, and whether the transplant center was in the United States) were included in the multivariate analysis, NRBC dose remained a significant predictor of time to reach an ANC of at least 500 (OR, 1.3 [P = .033] for 2.0-3.9 NRBCs × 106/kg; and OR, 1.3 [P = .026], for ≥ 4 NRBCs × 106/kg).7 10
Characteristics of 1112 patients given single-unit, unrelated-donor PCB transplants from the NYBC through September 30, 2001
| Characteristic . | No. (%) of patients . |
|---|---|
| Sex: M/F | 660 (59)/452 (41) |
| Ethnicity* | |
| Asian | 39 (4) |
| African-American | 161 (15) |
| Hispanic | 181 (17) |
| Caucasian | 658 (63) |
| Other | 26 (2) |
| Age at transplantation, y | |
| < 2 | 221 (20) |
| 2-5 | 247 (22) |
| 6-11 | 258 (23) |
| 12-17 | 146 (13) |
| ≥ 18 | 240 (22) |
| Diagnosis | |
| Leukemia† | 727 (65) |
| Lymphoma | 26 (2) |
| Genetic disease‡ | 255 (23) |
| Other acquired disease1-153 | 104 (9) |
| Transplant center location | |
| United States | 907 (82) |
| Outside the United States | 205 (18) |
| Characteristic . | No. (%) of patients . |
|---|---|
| Sex: M/F | 660 (59)/452 (41) |
| Ethnicity* | |
| Asian | 39 (4) |
| African-American | 161 (15) |
| Hispanic | 181 (17) |
| Caucasian | 658 (63) |
| Other | 26 (2) |
| Age at transplantation, y | |
| < 2 | 221 (20) |
| 2-5 | 247 (22) |
| 6-11 | 258 (23) |
| 12-17 | 146 (13) |
| ≥ 18 | 240 (22) |
| Diagnosis | |
| Leukemia† | 727 (65) |
| Lymphoma | 26 (2) |
| Genetic disease‡ | 255 (23) |
| Other acquired disease1-153 | 104 (9) |
| Transplant center location | |
| United States | 907 (82) |
| Outside the United States | 205 (18) |
Unknown for 23 patients.
Includes 322 patients with acute lymphoblastic leukemia, 270 with acute myelogenous leukemia, and 109 with chronic myelocytic leukemia.
Includes 35 patients with Fanconi anemia, 36 with severe combined immunodeficiency, and 27 with Wiskott-Aldrich syndrome.
Includes 33 patients with severe aplastic anemia and 51 with myelodysplasia.
Myeloid engraftment.
Incidence of achieving an ANC of at least 500/μL after transplantation, according to cell dose per kilogram of patient's body weight. The plus sign indicates patients who died, had autologous recovery, received another back-up graft, or relapsed before they achieved an ANC of at least 500. (A) TNC dose. (B) NRBC dose. (C) WBC dose. (D) CFC dose.
Myeloid engraftment.
Incidence of achieving an ANC of at least 500/μL after transplantation, according to cell dose per kilogram of patient's body weight. The plus sign indicates patients who died, had autologous recovery, received another back-up graft, or relapsed before they achieved an ANC of at least 500. (A) TNC dose. (B) NRBC dose. (C) WBC dose. (D) CFC dose.
OR for faster myeloid engraftment, according to cell dose per kilogram (before cryopreservation)
| Variable . | No. of patients . | OR for faster time to ANC ≥ 500 . | |
|---|---|---|---|
| Univariate (95% CI;P) . | Multivariate (95% CI; P) . | ||
| NRBCs/kg (× 106) | |||
| < 1.0 | 309 | 1.0 | 1.0 |
| 2.0-1.9 | 207 | 1.1 (0.9-1.4; .25) | 1.1 (0.8-1.3; .6) |
| 2.0-3.9 | 202 | 1.6 (1.3-1.9; < .001) | 1.4 (1.1-1.8; .002) |
| ≥ 4.0 | 308 | 1.7 (1.4-2.1; < .001) | 1.3 (1.03-1.6; .026) |
| WBCs/kg (× 106): | |||
| < 25 | 331 | 1.0 | 1.0 |
| 25-49 | 335 | 1.3 (1.1-1.6; .003) | 1.3 (1.1-1.6; .011) |
| 50-99 | 238 | 1.7 (1.4-2.1; < .001) | 1.6 (1.3-2.0; < .001) |
| ≥ 100 | 122 | 2.8 (2.2-3.6; < .001) | 2.5 (1.9-3.3; < .001) |
| Variable . | No. of patients . | OR for faster time to ANC ≥ 500 . | |
|---|---|---|---|
| Univariate (95% CI;P) . | Multivariate (95% CI; P) . | ||
| NRBCs/kg (× 106) | |||
| < 1.0 | 309 | 1.0 | 1.0 |
| 2.0-1.9 | 207 | 1.1 (0.9-1.4; .25) | 1.1 (0.8-1.3; .6) |
| 2.0-3.9 | 202 | 1.6 (1.3-1.9; < .001) | 1.4 (1.1-1.8; .002) |
| ≥ 4.0 | 308 | 1.7 (1.4-2.1; < .001) | 1.3 (1.03-1.6; .026) |
| WBCs/kg (× 106): | |||
| < 25 | 331 | 1.0 | 1.0 |
| 25-49 | 335 | 1.3 (1.1-1.6; .003) | 1.3 (1.1-1.6; .011) |
| 50-99 | 238 | 1.7 (1.4-2.1; < .001) | 1.6 (1.3-2.0; < .001) |
| ≥ 100 | 122 | 2.8 (2.2-3.6; < .001) | 2.5 (1.9-3.3; < .001) |
Results are from a Cox regression analysis. The analysis excluded 83 patients whose time to achieve an ANC of at least 500 was unknown, 2 patients whose NRBC dose was unknown, and 16 patients who died or relapsed before posttransplantation day 9, the day that the first patient had engraftment.
The correlation between the concentration of NRBCs and hematopoietic progenitors, measured as either CFCs15 or CD34+cells, probably accounts for the unexpected correlation between NRBCs and speed of myeloid engraftment after transplantation. The association also implies the existence of an intrinsic numerical balance between true stem cells and their more mature progeny in the rapidly growing fetus, such that increased production and release of mature blood cells must also involve replication and release of stem cells. In this regard, it is of interest that genetic variation in the control of the numbers of cells capable of engraftment has been demonstrated in mice.16
The findings in this study have practical implications in cord-blood graft selection, given that the number of TNCs per kilogram of the patient's body weight is commonly used to evaluate the engraftment potential of hematopoietic stem cell grafts.5-10 17-22 The presence of relatively high numbers of NRBCs in some cord-blood units has raised concern from 2 perspectives. First, NRBCs lyse more easily than WBCs on thawing and cause unexpectedly high TNC losses when frozen cord-blood units with many NRBCs are thawed before transplantation (P.W., personal communication, June 2001). From this perspective, CFC or CD34+ cell counts provide a more stable index. Alternatively, the contribution of NRBCs to the TNC count should be reported so that clinicians can anticipate this loss. Second, there is concern that inclusion of NRBCs in the TNC count might exaggerate estimation of the effective cell dose. Our results indicate, however, that the presence of NRBCs in a PCB graft does not reduce its engraftment potential. Rather, high NRBC counts identified PCB units that engrafted faster than units supplying the same TNC dose but lacking NRBCs.
In summary, the presence of some NRBCs in the peripheral blood at birth is the “norm.” The significant correlation between the NRBC and progenitor cell counts and their positive association with engraftment indicates that inclusion of NRBCs in the TNC count does not reduce the effectiveness of the prefreezing TNC count as an index of the quality of PCB units as grafts. Thus, the presence of high NRBC counts in umbilical cord blood should not a priori disqualify a PCB unit for transplantation, although an elevated number might justify further investigation into its possible causes. Accurate NRBC counts, however, would inform transplantation physicians to expect the apparent, but unimportant, reduction in nucleated cell counts on thawing of PCB grafts that contain high concentrations of NRBCs.
We thank the hospital physicians and nursing staff who have supported the NYBC's Placental Blood Program since its inception; the Placental Blood Program staff in the hospitals who collected the cord-blood samples, obtained consent, and gathered the data (Michael Moucatel, Sally South, Ali-Deena Baptiste, Carmen Alba, Nelly Marquez, Dona Goorshammy, Diana Santiago, and Christine Boehm); and the laboratory staff who performed the assays (George Chen, Diana Daniels, Shang-Te Yu, Jill Wittenburg, Armando Hernandez, Guo-Zhen Xu, and Gabriel Alespeiti).
Supported in part by National Heart, Lung, and Blood Institute award HL48031 (1992-1995) and by special gifts from Citicorp, Baxter Healthcare, and the Starr Foundation.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Cladd E. Stevens, New York Blood Center, 310 East 67th St, New York, NY 10021; e-mail: cstevens@nybc.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal