Abstract
In most cases, Hodgkin and Reed-Sternberg (HRS) cells of classical Hodgkin disease (HD) carry rearranged immunoglobulin (Ig) genes and thus derive from B cells. In rare cases, HRS cells originate from T cells. However, based on the unusual immunophenotype of HRS cells, often showing coexpression of markers typical for different hematopoetic lineages, and the regular detection of numerical chromosomal abnormalities, it has been speculated that HRS cells might represent cell fusions. Five cases of HD with 2 rearranged IgH alleles were analyzed for the presence of additional IgH alleles in germline configuration as a potential footprint of a cell fusion between a B and a non-B cell. Similarly, one case of T-cell–derived HD with biallelic T-cell receptor β (TCRβ) rearrangements was studied for the presence of unrearranged TCRβ alleles. In none of the 6 cases was evidence for additional IgH (or TCRβ) alleles obtained, strongly arguing against a role of cell fusion in HRS cell generation.
Introduction
In most cases of classical Hodgkin disease (HD), Hodgkin and Reed-Sternberg (HRS) cells carry clonal immunoglobulin (Ig) gene rearrangements and thus derive from B cells.1Specifically, the pattern of somatic mutations in the rearranged Ig genes indicates that these cells represent transformed preapoptotic germinal center B cells.1,2 In rare cases, HRS cells derive from T cells.3,4 However, the morphology and immunophenotype of HRS cells is untypical for B and also T cells. HRS cells lack expression of most B-cell markers,5,6 and molecules typical for other lineages are regularly expressed by these cells.5,7 Another typical feature of HRS cells is their abnormal karyotype. Numerical chromosomal abnormalities with additional copies of several chromosomes are not only observed in the multinucleated Reed-Sternberg cells but also in the mononuclear Hodgkin cells.8,9 Based on these observations, it has been speculated that HRS cells might represent cell fusions.10-13 For example, the coexpression of B and dendritic cell markers was taken as an indication that these cells derive from a fusion of a B lymphocyte with a dendritic cell. To clarify this matter, we analyzed single HRS cells from 5 cases of HD with 2 rearranged IgH alleles for the presence of additional IgH alleles in germline configuration as a footprint for a fusion of a B cell with a non-B cell. Likewise, one case of T-cell–derived HD with 2 rearranged T-cell receptor (TCR)β loci was analyzed for additional TCRβ germline alleles.
Study design
Patients and tissues
The 6 cases investigated here were previously analyzed for Ig and/or TCRβ V gene rearrangements (Table1). They were selected from a collection of 26 cases of HD analyzed by us. Two VH region genes had been amplified from 5 of the cases, and 1 case analyzed for DHJH joints harbored such a joint besides a VHDHJH joint.
Micromanipulation and single-cell PCR
Single HRS cells were micromanipulated from immunostained frozen tissue sections.2,14 Before gene-specific polymerase chain reaction (PCR) was carried out, genomic DNA of single cells was preamplified with a random 15-mer primer.15 IgH and TCRβ VDJ and DJ gene rearrangements and fragments specific for germline configuration of IgH and TCRβ loci were amplified by seminested PCR and sequenced (Figure1).2,3 16 To rule out that germline polymorphisms at the binding sites for the IgH germline-specific PCR primers (DH7-27 and JH1) hamper amplification of germline fragments, fragments covering these sites were amplified from whole-tissue DNA of cases 2 to 5 (not shown). No polymorphisms were detected at the primer binding sites. In cases 2, 3, and 5, successful amplification of both IgH alleles was confirmed by a polymorphism near the DH7-27 gene. For patient 1, single micromanipulated T cells of the tumor tissue and, for patient 6, micromanipulated B cells were used for control amplification of germline-specific IgH or TCRβ fragments. For case 1, IgH germline-specific amplificates were obtained from 6 of 11 micromanipulated T cells and, from case 6, TCRβ germline-specific amplificates were obtained from 10 of 13 B cells.
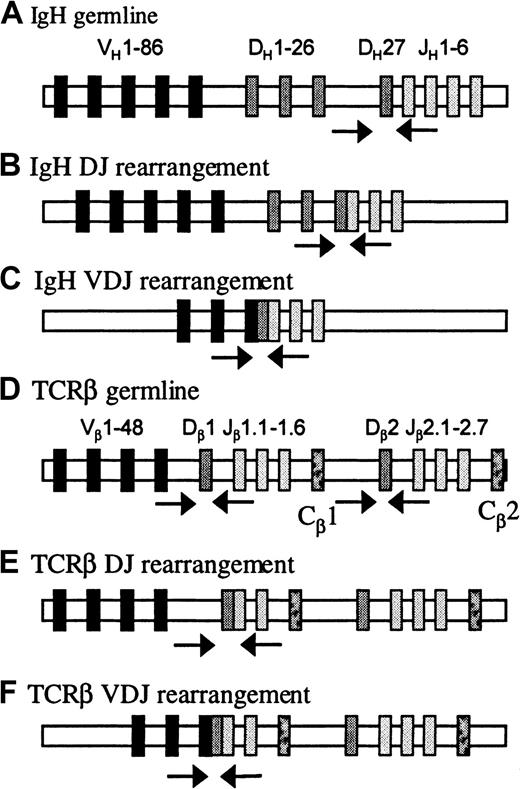
PCR strategies to type the rearrangement status of human IgH and TCRβ loci.
The human IgH locus harbors about 90 to 123 VH gene segments (depending on haplotype), 27 DH genes, and 6 JH genes. The human TCRβ locus is composed of 65 Vβ gene segments and 2 tandemly arranged D-J-C clusters: the first with 1 Dβ, 6 Jβ, and 1 Cβ genes, the second with 1 Dβ, 7 Jβ, and 1 Cβ genes. (A) IgH germline configuration is detected with a primer upstream of the most 3′ DH element (DH7-27) and the nested JH1 primers. Because DH7-27 is located only 80 base pairs upstream of the JH1 gene segment, the DH7-27–JH primer combination not only detects DH7-27–JH rearrangements but also the germline configuration of the IgH locus. (B) DHJH joints are amplified with a collection of 7 DH-family–specific primers and the nested JH primer mixes. (C) VHDHJH rearrangements are amplified with 6 VH-family–specific primers binding to the framework region 1 of human VH genes and the nested JHprimer mixes. (D) Germline configuration of the TCRβ locus is detected with primers binding intronic sequences 5′ and 3′ of the Dβ1 and Dβ2 genes. (E) DβJβ joints are amplified with the 5′ Dβ primers and nested Jβ primer mixes. (F) TCRβ VDJ rearrangements are amplified with a collection of 24 Vβ-family–specific primers and the 2 Jβprimer mixes. Arrows indicate location of primers.
PCR strategies to type the rearrangement status of human IgH and TCRβ loci.
The human IgH locus harbors about 90 to 123 VH gene segments (depending on haplotype), 27 DH genes, and 6 JH genes. The human TCRβ locus is composed of 65 Vβ gene segments and 2 tandemly arranged D-J-C clusters: the first with 1 Dβ, 6 Jβ, and 1 Cβ genes, the second with 1 Dβ, 7 Jβ, and 1 Cβ genes. (A) IgH germline configuration is detected with a primer upstream of the most 3′ DH element (DH7-27) and the nested JH1 primers. Because DH7-27 is located only 80 base pairs upstream of the JH1 gene segment, the DH7-27–JH primer combination not only detects DH7-27–JH rearrangements but also the germline configuration of the IgH locus. (B) DHJH joints are amplified with a collection of 7 DH-family–specific primers and the nested JH primer mixes. (C) VHDHJH rearrangements are amplified with 6 VH-family–specific primers binding to the framework region 1 of human VH genes and the nested JHprimer mixes. (D) Germline configuration of the TCRβ locus is detected with primers binding intronic sequences 5′ and 3′ of the Dβ1 and Dβ2 genes. (E) DβJβ joints are amplified with the 5′ Dβ primers and nested Jβ primer mixes. (F) TCRβ VDJ rearrangements are amplified with a collection of 24 Vβ-family–specific primers and the 2 Jβprimer mixes. Arrows indicate location of primers.
Results and discussion
Experimental strategy
Due to their extreme diversity, V gene rearrangements represent ideal markers for distinct IgH alleles in a B cell. Most B cells in the human carry rearrangements on both IgH alleles,17 either 2 VHDHJH rearrangements (one functional and one nonfunctional joint) or a VHDHJH rearrangement together with a DHJH joint. Non-B cells have IgH loci in germline configuration (or rarely DHJH joints). On this basis, the detection of 3 or 4 distinct IgH alleles in a cell would represent a strong indication that this cell derived from a cell fusion.
That HRS cells are fusions of B cells is highly unlikely because, among more than 40 cases of classical HD analyzed, not a single case with more than 2 VHDHJH rearrangements was observed.2,3,14 18-20 However, if HRS cells represent fusions of B cells with non-B cells, one would expect to detect IgH loci in germline configuration in addition to the B-cell–derived IgH alleles. HRS tumor clones that harbor only one rearranged IgH allele would not be informative in the analysis, because the assay does not distinguish between one or more germline alleles in a cell. Hence, we restricted ourselves to cases in which we had detected 2 clonal IgH gene rearrangements in previous studies. For the characterization of the IgH loci of HRS cells, we analyzed single cells for VHDHJH rearrangements and with a DH7-27–specific primer (or a DH primer collection) together with JH primers to detect germline configuration. This is based on the fact that in almost all DHJH and all VHDHJH rearrangements the primer binding site upstream of DH7-27 is deleted (Figure 1).
Because the principles of gene rearrangements in IgH alleles also apply to the TCRβ locus (as far as rearrangements and germline configuration for 1 of the 2 Cβ clusters are concerned, see Figure 1), we also analyzed a case of T-cell–derived HD with 2 rearranged TCR Cβ loci using corresponding primer combinations.
Reliability of the experiments
To confirm the reliability of the results, 4 types of controls were performed: (1) Because of the whole-genome preamplification, aliquots of amplified DNA from a given HRS cell could be analyzed for VDJ and DJ rearrangements and germline configuration. Through this approach we tested the samples for the presence of amplifyable DNA. (2) In parallel with the HRS cells, single-flow cytometrically isolated T cells (or B cells in case 6) were analyzed for the presence of germline fragments. Germline-specific amplificates were obtained from nearly all samples (Table 1), showing that the PCR worked very efficiently. (3) To rule out that a lack of germline-specific amplificates from HRS cells of a given case is due to polymorphisms at the primer binding sites, we confirmed that in each of the 6 cases amplification of germline-specific fragments was feasible (see “Study design”). (4) PCR contamination was controlled by analyzing samples containing buffer aspirated from the tissue sections used for HRS cell isolation. With a single exception, all buffer samples were negative (Table 1).
Molecular analysis of HRS cells for VDJ and DJ rearrangements and germline configuration of the IgH or TCRβ loci
For cases 1 to 5, between 14 and 65 single HRS cells were analyzed for VHDHJH gene rearrangements, and 10 to 14 cells of cases 1 to 4 also were analyzed for DHJH joints. In each of the 5 cases, 2 clonal IgH gene rearrangements were detected (Table 1). For case 6 with T-cell–derived HRS cells, a clonal VβDβJβ and a clonal DβJβ rearrangement were each repeatedly amplified (Table 1). Both rearrangements involved D and J segments of the Cβ1 cluster.
When the HRS cells of cases 1 to 5 were analyzed for IgH germline amplificates, only 2 products were obtained from a total of 80 HRS cells (Table 1). In the analysis of case 6 for TCRβ germline configuration of the Cβ1 cluster, a single amplificate was obtained from 30 HRS cells.
No indication for cell fusion in HD
In each of the 6 cases analyzed, 2 clonal IgH (or TCRβ) gene rearrangements were detected. Because 5 of the cases were analyzed for both VDJ and DJ rearrangements, this finding further supports that HRS cells do not represent fusions of B cells (as discussed above).
In the analysis for the presence of additional germline-specific fragments, only 3 amplificates, each from a different case, were obtained from a total of 110 HRS cells. These PCR products most likely represent contamination: A germline-specific product was also obtained from a buffer control, and the frequencies of buffer contamination (1 of 42) and germline products from HRS cells (3 of 110) were comparable. Furthermore, a similar level of contamination was occasionally observed in previous studies using the same micromanipulation approach.15 18 Finally, because the germline-specific PCR worked very efficiently (Table 1), germline-specific fragments should be amplified at least as efficiently as the clonal IgH (or TCRβ) gene rearrangements. On this background, one would expect to detect IgH or TCRβ alleles in germline configuration—if present in the HRS cells— in at least 30% to 50% of the cells. Taking these aspects together, the results of the present study represent strong evidence against the presence of IgH (or TCRβ) alleles in germline configuration in the 6 cases analyzed.
Because this study was restricted to the analysis of chromosome 14 in cases 1 to 5 or chromosome 7 in case 6, one might argue that there could be a preferential loss of these chromosomes in fused cells. However, the frequent detection of HRS cells with several copies of chromosome 14 and/or 721 argues against this idea (no cytogenetic data are available for the cases analyzed here). Thus, it appears likely that additional copies of chromosomes in Hodgkin cells derive from duplication and that multinucleated Reed-Sternberg cells derive from mononucleated Hodgkin cells through endomitosis and not cell fusion. In Epstein-Barr virus–positive cases of HD, the generation of multinucleated cells may be promoted by latent membrane protein-1 expression.22
Given that HRS cells do not represent natural hybridomas, the question arises as to how the unusual phenotype of HRS cells can be explained. Perhaps this is related to the proposed origin of HRS cells from preapoptotic germinal center B cells.1,2 A (premalignant) germinal center B cell that lost its capacity to express an appropriate high-affinity antigen receptor but is prevented from undergoing apoptosis may down-regulate expression of Ig and other B-cell–specific genes and undergo differentiation processes related to other hematopoietic lineages. This idea would be reminescent of the phenotype of Pax5-deficient mice, in which pro-B cells prevented from developing into mature B cells can develop into other cell types like T cells and monocytes.23
Acknowledgments
We thank Christiane Gerhardt, Tanja Schaffer, and Julia Jesdinsky for technical assistance.
Supported by grants from Deutsche Forschungsgemeinschaft (through SFB502 and a Heisenberg stipend to R.K.) and the Deutsche Krebshilfe, Mildred Scheel Stiftung. M.M. holds a postdoctoral fellowship from the Cancer Research Institute (New York, NY).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Ralf Küppers, University of Cologne, Department of Internal Medicine I, LFI E4 R706, Joseph-Stelzmannstr. 9, D-50931 Cologne, Germany; e-mail: rkuppers@mac.genetik.uni-koeln.de.