Abstract
Kaposi sarcoma-associated herpesvirus encodes viral IL-6 (vIL-6). To investigate the potential role of vIL-6 in the pathogenesis of human immunodeficiency virus (HIV)- related primary effusion lymphomas (PEL), a sensitive enzyme-linked immunosorbent assay was developed for vIL-6 and applied to the study of PEL. Whereas vIL-6 was detectable in 6 of 8 PEL effusions (range, 1390-66 630 pg/mL), it was not detectable in any of the control effusions. As expected, all PEL effusions contained human IL-6 (range, 957-37 494 pg/mL), and 7 of 8 contained detectable human IL-10 (range, 66-2,521,297 pg/mL). Human and vIL-6 have previously been shown to induce vascular endothelial growth factor, which in turn can increase vascular permeability. The results of the current study suggest that these cytokines play a central role in the pathogenesis and manifestations of PEL.
Introduction
Primary effusion lymphoma (PEL) is a peculiar and infrequent type of non-Hodgkin lymphoma that arises predominantly in patients with human immunodeficiency virus (HIV). PEL displays liquid growth in the serous cavities of the body, often in the absence of a clearly identifiable tumor mass.1 In most patients, PEL cells are dually infected with Epstein–Barr virus (EBV) and Kaposi sarcoma-associated herpesvirus (KSHV; also known as human herpesvirus 8),2,3 and they produce several cytokines, including a viral homologue of IL-6 (vIL-6).4-6 Human IL-6 (hIL-6), a multifunctional cytokine that acts on many cells, serves as a growth factor for myeloma and plasmacytoma cells and stimulates B-cell differentiation.7,8 vIL-6 supports the growth of IL-6–dependent cell lines in vitro4,5,9 and serves as an autocrine growth factor for PEL cell lines.10 When expressed in mice, recombinant vIL-6 accelerates the hematopoiesis of myeloid, erythroid, B-lymphoid, and megakaryocytic lineages and induces vascular endothelial growth factor (VEGF), which has been implicated in the pathogenesis of PEL.11-13
Although HIV-associated lymphomagenesis is poorly understood, in vitro experiments and transgenic models have shown that HIV-derived proteins can activate a number of cellular genes.14,15 The HIV transactivator protein Tat has been reported to promote the expression of hIL-6 and hIL-10 in lymphoid cells.15 Further, HIV infection and soluble factors released from HIV-infected cells can induce lytic replication of KSHV in a PEL cell line.16hIL-6 expression, which is constitutive in PEL cell lines, is down-regulated during KSHV lytic replication induced by phobor esters.17 By contrast, vIL-6 expression, low in PEL cell lines latently infected with KSHV, is markedly induced during KSHV lytic replication.18 Here we investigated potential relationships between HIV load and the induction of selected cellular and KSHV-derived cytokines. Using a newly developed vIL-6–specific enzyme-linked immunosorbent assay (ELISA), we measured vIL-6 in acquired immunodeficiency syndrome (AIDS)-PEL effusions that contain HIV RNA and cellular cytokines.
Study design
Patients
Body cavity effusions from 8 AIDS patients with PEL, 21 HIV-negative patients with malignancies or congestive heart failure, and 4 AIDS patients with inflammatory processes without PEL were obtained from the AIDS Malignancy Bank (National Cancer Institute, Bethesda, MD) and from our institutes. The diagnosis of PEL was based on clinical presentation, histology of the effusion cells, and the presence of KSHV in the lymphoma cells. HIV RNA load was measured by the Amplicor HIV-1 reverse transcription–polymerase chain reaction (RT-PCR) test (Roche Diagnostic Systems, Basel, Switzerland).
Enzyme-linked immunosorbent assays for vIL-6, hIL-6, and hIL-10
The ELISA for vIL-6 used mouse monoclonal and rabbit polyclonal antibodies raised against recombinant vIL-6.10,11,19Polystyrene plates (Immunol 1B; Dynex Technologies, Chantilly, VA) were coated with mouse monoclonal anti–vIL-6 antibody (v6m12.1.1; 4 μg/mL in carbonate buffer, pH 9) overnight at 4°C. After washing the plates with phosphate-buffered saline (PBS) containing 0.05% Tween 20 (PBS-T) and blocking with SuperBlock (Pierce, Rockford, IL), test samples were added in triplicate to the wells (initial dilution, 1:10 in PBS-T). Plates were incubated overnight at room temperature and washed with PBS-T. Rabbit polyclonal anti–vIL-6 antibody (0.5 μg/mL) was added to the wells in PBS-T containing 0.5% bovine serum albumin (PBS-T/BSA). Plates were incubated for 2 hours at room temperature and washed. Affinity-purified human serum protein-absorbed goat antirabbit IgG antibody conjugated to alkaline phosphatase (Sigma, St Louis, MO; 1:400 dilution in PBS-T/BSA) was added. Plates were incubated at room temperature for 1.5 hours and washed with PBS-T,p-nitrophenolphosphate substrate (Sigma) was added to the wells, and plates were read at 405 nm with λ correction at 595 nm. A purified fusion protein of maltose-binding protein (MBP; 42.7 kd) and amino acids 22 to 204 of vIL-6 (21.6 kd) was used as the standard.11 The concentration of vIL-6 was calculated from absorbance values in relation to the standard curve, correcting for the presence of the MBP fusion protein in the vIL-6 standard (vIL-6 corresponds to 33.6% of MBPvIL-6). hIL-6 and hIL-10 were measured by commercially available ELISA kits (R&D Systems, Minneapolis, MN).
Western blotting
Western blot analysis for vIL-6 and hIL-6 was performed as described previously.10 Rabbit polyclonal and a mouse monoclonal (v6m12.1.1) antibodies against vIL-6 and mouse monoclonal antibody against hIL-6 (mAb206; R&D Systems) were used as the primary antibodies. MBPvIL-6 was cleaved with factor Xa (New England BioLabs, Beverly, MA).
Statistical analysis
The nonparametric Spearman-Rho test was used to measure the significance of correlations between groups.
Results and discussion
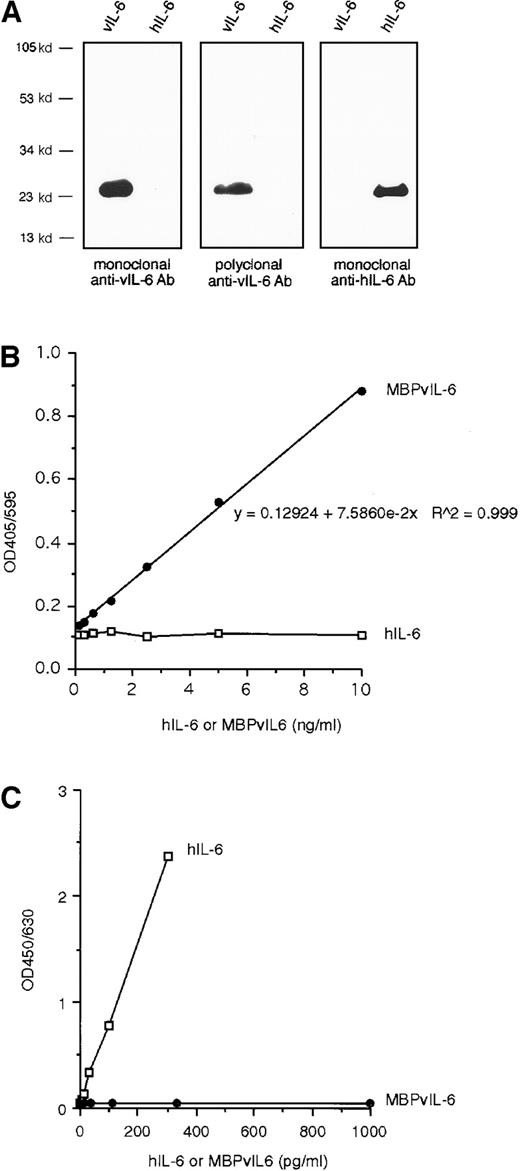
vIL-6 exhibits 24.7% amino acid identity to hIL-6.4Thus, an assay for vIL-6 must be able to distinguish it from hIL-6. As assessed by both immunoblotting (Figure1A) and direct ELISA (not shown), neither a rabbit polyclonal nor a mouse monoclonal antibody raised against recombinant vIL-6 recognized hIL-6 (Fig. 1A). Using these antibodies, we developed a vIL-6 ELISA. This assay displays a lower limit of sensitivity calculated at approximately 30 pg/mL of vIL-6 and is linear between 30 and 3360 pg/mL of vIL-6. This ELISA does not detect hIL-6 (Figure 1B), and a commercial hIL-6 ELISA kit (R&D systems) does not detect vIL-6 (Fig. 1C).
Antibody specificity for vIL-6 and establishment of a vIL-6 ELISA.
(A) By Western blotting, a rabbit polyclonal antibody and a mouse monoclonal antibody raised against recombinant vIL-6 recognized vIL-6 but not hIL-6; a mouse anti-hIL-6 monoclonal antibody recognized hIL-6 but not vIL-6. (B) Detection of vIL-6 by a solid-phase sandwich ELISA using an anti-vIL-6 mouse monoclonal and a rabbit polyclonal antibodies. The lower limit of sensitivity (the minimum amount of protein detected with 95% confidence) was calculated at 43.8 pg/mL MBP-vIL-6. The assay is linear (r = 0.999) between 30 and 3360 pg/mL of vIL-6. hIL-6 was not recognized in this vIL-6 ELISA. (C) Detection of hIL-6, but not vIL-6, by a hIL-6–specific ELISA.
Antibody specificity for vIL-6 and establishment of a vIL-6 ELISA.
(A) By Western blotting, a rabbit polyclonal antibody and a mouse monoclonal antibody raised against recombinant vIL-6 recognized vIL-6 but not hIL-6; a mouse anti-hIL-6 monoclonal antibody recognized hIL-6 but not vIL-6. (B) Detection of vIL-6 by a solid-phase sandwich ELISA using an anti-vIL-6 mouse monoclonal and a rabbit polyclonal antibodies. The lower limit of sensitivity (the minimum amount of protein detected with 95% confidence) was calculated at 43.8 pg/mL MBP-vIL-6. The assay is linear (r = 0.999) between 30 and 3360 pg/mL of vIL-6. hIL-6 was not recognized in this vIL-6 ELISA. (C) Detection of hIL-6, but not vIL-6, by a hIL-6–specific ELISA.
PEL cell cultures consist largely of cells latently infected with KSHV, with a minority of cells undergoing lytic KSHV replication.20 Treatment with the phorbol ester 12-O-tetradecanoylphorbol-13-acetate (TPA) rapidly induces lytic KSHV replication. The KSHV-positive PEL cell lines BC-1, BCP-1, and BCBL-1 were found to release vIL-6 into the supernatant, as did the vIL-6–transfected NIH3T3 v6O cells (Table1).11 The addition of TPA to PEL cells enhanced vIL-6 release in the culture supernatants. No vIL-6 was detected in the supernatants from the KSHV-negative Burkitt lymphoma cell line Daudi or the EBV-immortalized VDS-O1 cell line, which is transfected with an hIL-6 expression vector.21
vIL-6 was detected in 6 of 8 PEL effusions (mean, 13,884 pg/mL) but was undetectable in the 21 control benign or malignant effusions from HIV-negative patients (not shown; P < .0001,Fisher exact test). vIL-6 was also undetectable in 4 nonmalignant effusions from patients with AIDS (not shown). HIV RNA was examined in 8 malignant lymphomatous effusions (Table2). Except for one sample in which test results could not be evaluated because of an inhibitor, HIV RNA was detected in all PEL effusions (mean, 562,967 copies/mL). hIL-6 was detected in all AIDS-PEL effusions (mean, 12,010 pg/mL) and in all control HIV-negative effusions (mean, 41 737 pg/mL; range, 127-624,870 pg/mL). No significant correlation was observed between vIL-6 and hIL-6 levels in PEL effusion (r = −0.2275;P = .5878). hIL-10 was detected in 7 of 8 PEL effusions (mean, 536,762 pg/mL). A statistically significant association was observed between HIV load and hIL-10 levels (r = 0.7857;P = .0362). However, no significant association was noted between HIV load and vIL-6 (r = −0.1622;P = .7283) and hIL-6 levels (r = −0.6786;P = .0938).
We conclude that PEL effusions generally contain vIL-6, hIL-6, hIL-10, and HIV RNA. Recently, we reported that these PEL effusions contain high levels of VEGF (mean, 3977 pg/mL; range 1133-11,417 pg/mL).13 PEL cells are a likely source of vIL-6, hIL-6, hIL-10, and VEGF detected in the lymphomatous effusions because PEL cell lines can express all these proteins in culture.10,12VEGF, which stimulates vascular permeability and may facilitate the accumulation of PEL effusions in vivo, was required for a PEL cell line to form effusion lymphomas in mice.12 hIL-6 and vIL-6, individually, can stimulate the expression of VEGF in tissues. In vitro, hIL-10 and vIL-6 serve as autocrine growth factors for PEL cell lines10 and may promote PEL cell growth in the body cavities. The observation that PEL effusions generally contain vIL-6, which can stimulate PEL cell growth and further promote the accumulation of effusions, suggests that this viral cytokine plays a critical role in PEL pathogenesis.
Acknowledgments
We thank Drs Yoshihiro Nambu, Chip Petricoin, Patty Fetsch, and Keith Brosky for providing control malignant effusions and Dr Timothy Alcorn, Laboratory Corporation of America (Research Triangle Park, NC) for quantitative PCR test for HIV. We also thank Dr Ghanshyam Gupta for statistical analyses and Drs Yuan Chang and Patrick S. Moore for critical reading of the manuscript.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Yoshiyasu Aoki, Medicine Branch, National Cancer Institute, National Institutes of Health, Building 10, Room 12C207, 8800 Rockville Pike, Bethesda, MD 20892; e-mail: aokiy@mail.nih.gov.