Abstract
Recent studies have shown decreased megakaryocyte expression of the thrombopoietin receptor (c-mpl) in patients with polycythemia vera (PV) but not in those with reactive erythrocytosis. We examined the diagnostic utility of this observation in 22 patients with PV, 7 patients with secondary erythrocytosis (SE), and 10 normal controls. Commercial antibodies against c-mpl were used with standard immunoperoxidase methods. Megakaryocyte c-mpl staining intensity was uniformly moderate-to-strong in the healthy controls and in all the patients with SE. In contrast, staining intensity in 9 patients with PV (41%) was uniformly weak. Furthermore, in 12 of the remaining 13 patients with PV, the c-mpl staining pattern in each case was heterogeneous and was associated with weak staining intensity in more than 20% of the megakaryocyte population. These preliminary data suggest that c-mpl immunostains may complement bone marrow histopathology in distinguishing PV from nonclonal causes of erythrocytosis.
The use of disease-specific biologic assays has resulted in the identification of patients with polycythemia vera (PV) who do not strictly fulfill the Polycythemia Vera Study Group (PVSG) diagnostic criteria.1-3 In this regard, both serum erythropoietin and endogenous erythroid colony assays have been shown to be diagnostically useful in distinguishing PV from secondary erythrocytosis (SE).4,5 However, both of these assays have substantial limitations. For example, although a decreased or increased serum erythropoietin level is consistent with a diagnosis of PV and SE, respectively, a “normal” level does not exclude either diagnosis.6,7 Similarly, the diagnostic value of an endogenous erythroid colony growth assay is hampered by the lack of widespread expertise in performing the test and interpreting the results.5
Therefore, the development of additional biologic assays that are both practical and relatively specific may not only help in distinguishing between PV and SE but may also allow detection of cases of PV that do not manifest the full complement of the PVSG criteria. In a recent study, platelet expression of the thrombopoietin receptor (c-mpl) was shown to be reduced in all 34 patients with PV who were tested and in none of the 14 patients with SE.8Similarly, decreased megakaryocyte c-mpl expression was reported in 10 patients with PV. In the current study, we evaluated the diagnostic value of c-mpl–based bone marrow immunohistochemical stains in 22 patients with PV, 7 patients with SE, and 10 normal controls.
Study design
Conventional criteria were used to identify patients with PV.9 The comparative groups included both normal controls and patients with SE. Immunohistochemical staining of c-mpl, in paraffin-embedded bone marrow sections, was accomplished by an immunoperoxidase method using avidin-biotin complexes and a mouse monoclonal anti-human c-mpl antibody (Genzyme, Cambridge, MA). Bone marrow section slides were deparaffinized in xylene, hydrated in sequential gradients of ethanol, and pretreated with heated ethylenediamine tetraacetic acid (1 mmol/L, pH 8.0) for 30 minutes. This was followed by sequential incubation in 1:200 dilution of c-mpl antibody for 1 hour, biotinylated goat anti-mouse antibodies (Dako, Denmark) for 30 minutes, and avidin-biotin complex reagent (Vecta Stain, Vector Laboratories, Burlingame, CA) for 30 minutes. After induction of the color reaction with 3-amino-9-ethylcarbazole substrate solution (Sigma, St Louis, MO), the slides were counterstained with hematoxylin.
The staining intensity (weak vs moderate vs strong) and pattern (uniform vs heterogeneous) of megakaryocyte c-mpl expression were semiquantitatively and independently evaluated by all the authors. In addition, 2 of the authors (S.Y.Y. and C.Y.L.) were blinded to the clinical diagnosis during the interpretation of the immunostains. In an individual patient, the staining pattern was categorized as being uniform if more than 80% of the megakaryocytes displayed similar staining intensity. Otherwise, the staining pattern was classified as being heterogeneous and the associated staining intensity connotation was based on majority. The histologic assessment of megakaryocyte number and morphology was reviewed jointly by 2 of the authors (S.Y.Y. and C.Y.L.). Statistical calculations were performed by using StatView software (Version 5.0.1, SAS Institute, Cary, NC).
Results and discussion
Bone marrow c-mpl studies were performed on bone marrow trephine biopsy specimens of 22 patients with PV, 7 with SE, and 10 normal controls. In the patients with PV, the immunohistochemical studies were performed either at diagnosis (9 patients) or later in the course of the disease. At the time of the study, 15 patients were chemotherapy naı̈ve, 9 had a history of thrombosis, and 6 were showing early signs of transformation of their disease into myelofibrosis with myeloid metaplasia. The causes of SE were central hypoxia (3 cases), central hypoxia and diabetes insipidus (1 case), high-oxygen–affinity hemoglobinopathy (1 case), and apparent erythrocytosis (2 cases). The median hemoglobin value in patients with SE was 18.7 g/dL. As outlined in Table 1, and consistent with previous studies,10 bone marrow histopathologic differences between PV and SE were readily apparent.
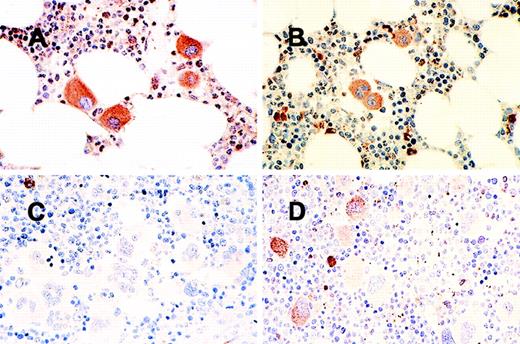
In general, staining intensity of megakaryocyte c-mpl was uniformly moderate to strong in both normal controls and all the patients with SE (Figure 1A and B, Table2). In contrast, weak staining intensity was demonstrated in at least 20% of the megakaryocyte population in 21 of the 22 patients with PV. In 9 of these 22 patients (41%), more than 80% of the megakaryocytes displayed weak staining intensity (Figure1C, Table 2). In 12 of the 13 remaining patients with PV, the staining pattern was heterogeneous (Figure 1D, Table 2). One patient with PV showed moderate staining intensity in a uniform fashion. These variations in staining intensity and pattern did not correlate with the duration or stage of the disease and were also not influenced by the presence of chemotherapy (data not shown).
Bone marrow immunohistochemical stains for megakaryocytec-mpl.
(A) Uniformly strong staining in secondary erythrocytosis; (B) uniformly moderate staining in a normal control; (C) uniformly weak staining in a patient with polycythemia vera; (D) heterogeneous staining in another patient with polycythemia vera.
Bone marrow immunohistochemical stains for megakaryocytec-mpl.
(A) Uniformly strong staining in secondary erythrocytosis; (B) uniformly moderate staining in a normal control; (C) uniformly weak staining in a patient with polycythemia vera; (D) heterogeneous staining in another patient with polycythemia vera.
These observations are mostly consistent with a recent study that demonstrated reduced c-mpl expression by platelets and megakaryocytes in patients with PV, but not in those with SE.8 However, this study suggests that megakaryocytec-mpl expression, both in a particular patient and between patients, may show substantial heterogeneity. The differences between the 2 studies may be due to differences in antibody preparations, although the mouse monoclonal antibody we used is also directed against the extracellular domain of the c-mpl protein.11 On the other hand, the observed interpatient and intrapatient variations in staining intensity may be related to differences in the content of an underglycosylated c-mpl isoform that has been reported to exist in patients with PV.11 Interpatient variability in platelet c-mpl expression has previously been reported in patients with ET.12
It should be recognized that the majority of patients with PV present with clinically evident disease and the diagnosis may not require the use of sophisticated tests. In cases that are difficult to diagnose, however, bone marrow immunohistochemical staining for c-mpl may complement the diagnostic value of bone marrow histopathology and obviate in vitro endogenous erythroid colony assays.
Reprints:Ayalew Tefferi, Division of Hematology and Internal Medicine, Mayo Clinic, 200 First St SW, Rochester, MN 55905.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.