Abstract
Adhesion molecules borne by both endothelial cells and circulating leukocytes are in large measure responsible for guiding the process of extravasation. The selectin family has been primarily associated with the early stages of adhesion involving initial contact and rolling. A significant body of evidence has accumulated indicating a fundamental role for the endothelial members of this family, E- and P-selectin, in a variety of inflammatory states and models. Although originally identified as the lymph node-specific lymphocyte homing receptor, L-selectin has also been suggested to play an important role in leukocyte recruitment to sites of inflammation. We have recently demonstrated, using L-selectin–deficient mice, that defects in contact hypersensitivity (CHS) responses are in essence due to the inability of T cells to home to and be sensitized within peripheral lymph nodes, whereas nonspecific effector cells are fully capable of entry into sites of cutaneous inflammation (Catalina et al, J Exp Med184:2341, 1996). In the present study, we perform an analysis of adhesion molecule usage in two models of skin inflammation and show in both L-selectin–deficient as well as wild-type mice that a combination of P- and E-selectin is crucial for the development of both acute (croton oil) and chronic (contact hypersensitivity) inflammation at sites of the skin, whereas L-selectin does not appear to play a significant role. Moreover, 4 integrins are shown to be integral to a CHS but not an acute irritant response, whereas CD44 does not significantly contribute to either. These results provide a systematic examination in one study of major adhesion molecules that are critical in acute and chronic skin inflammation. They reinforce the essential role of the collaboration of E- and P-selectin in both specific and nonspecific skin inflammatory responses and the importance of 4 in the specific response only. In addition, they substantiate only a limited role, if any, for L-selectin in these cutaneous effector mechanisms and demonstrate the essential equivalence in this analysis of L-selectin–deficient mice compared with normal mice treated with blocking antibodies.
THE RECRUITMENT OF leukocytes to sites of inflammation is a critical component of the response to tissue injury; thus, the elucidation of molecules mediating the extravasation of leukocytes from the periphery into the inflamed tissue is central to the understanding of the complex regulation of the host response to inflammation. Several families of adhesion receptors are thought to be essential in the multistep model of extravasation for both nonspecific effector cells as well as antigen-specific lymphocytes.1,2The initial contact with and rolling on endothelium is mediated principally by the selectin family of molecules: L-selectin expressed on leukocytes and the endothelial P- and E-selectins.3 The endothelial selectins have clearly been shown in numerous model systems using gene-targeting approaches to participate in an essential fashion in the recruitment of leukocytes to sites of inflammation, including sites of a cutaneous delayed-type hypersensitivity (DTH) response.4-9
Although L-selectin was originally described as the lymph node-specific homing receptor,10-12 its role in the extravasation of leukocytes at sites of inflammation has also been extensively investigated. L-selectin expression on circulating nonspecific effector populations (ie, neutrophils and monocytes) has been suggested to be an important mediator of the primary adhesion of these cells at sites of inflammation.13-19 It has additionally been shown that, although independent ligands clearly exist,3 carbohydrates borne by L-selectin may function as ligands for neutrophils to bind to E- or P-selectin on endothelial cells in the human,20,21and it has been further suggested that L-selectin may exert its effect at inflammatory sites by mediating leukocyte-leukocyte interactions that facilitate the recruitment of neutrophils.22
We have previously generated L-selectin–deficient mice by targeted disruption and demonstrated a strikingly impaired contact hypersensitivity (CHS) response to reactive haptens,23 in agreement with others.24,25 However, our analysis indicated that T cells, as well as neutrophil and monocyte effector populations, are fully capable of entry into inflamed skin sites in the absence of L-selectin and that the defect in CHS resides primarily in the inability of antigen-specific T cells to home to and be activated within lymph nodes, ie, in antigen sensitization rather than leukocyte recruitment. Indeed, L-selectin–deficient mice mounted completely normal CHS responses when alternate routes of immunization were used. In support of this, an acute cutaneous inflammatory response to an irritant was also completely normal.23 These results argued against a role for L-selectin in leukocyte migration into such inflamed sites in these mutant mice, thus raising the issues of which adhesion receptors were indeed responsible for such localization and whether this is also true for normal mice. The degree to which L-selectin participates in such responses at sites of inflammation has not been fully resolved, and it has been suggested that L-selectin may be responsible for the residual CHS responses seen in P/E-selectin deficient animals.7
In these studies, using both wild-type and L-selectin–deficient mice we have investigated the use of adhesion molecules in models of both an acute nonspecific inflammatory response as well as an antigen-specific CHS response. We demonstrate that L-selectin does not significantly contribute either in wild-type mice using antibody blockade or in L-selectin–deficient mice to the recruitment of leukocytes at sites of cutaneous inflammation. In contrast, antibodies to P- and E-selectin together, but not singly, are necessary and sufficient to effectively block the recruitment of neutrophils in an acute nonspecific irritant response and to inhibit the ear swelling as well as the attendant leukocyte recruitment to an antigen-specific allergic contact dermatitis. The concordance of observations using these two approaches suggests that leukocyte recruitment to sites of cutaneous inflammation in L-selectin–deficient mice does not result from compensatory mechanisms and that ligands distinct from L-selectin are clearly operative in interactions with P- and E-selectin. Moreover, the results indicate that blocking antibody to VLA-4 is strikingly inhibitory in a CHS, but has no effect on the recruitment of neutrophils in acute nonspecific inflammation. Together, these data suggest that the mechanism for recruitment of nonspecific effector cells to the skin relies heavily on expression of P- and E-selectins and their ligands, additionally on VLA-4 for antigen-specific responses, but not on L-selectin for either acute or chronic inflammatory responses.
MATERIALS AND METHODS
Mice.
L-selectin–deficient mice (−/−) were generated by targeted disruption of the L-selectin locus, as described.23 Two- to three-month-old 129Sv/C57Bl wild-type or L-selectin–deficient mice were used and were housed in the animal resource center of the University of Texas Southwest Medical Center (Dallas, TX).
Reagents and antibodies.
Croton oil, DNBS (2, 4-dinitrobenzene sulfonic acid), and DNFB (2, 4-dinitrofluorobenzene) were purchased from Sigma (St Louis, MO). The following antimouse monoclonal antibodies (MoAbs) were used for fluorescence-activated cell sorter (FACS) analysis and/or immunohistochemistry: anti-GR-1-biotin (granulocytes and neutrophils) and anti-Mac-1-biotin (CD11b; macrophages and neutrophils) (Pharmingen, San Diego, CA); anti-Thy1.2-biotin (Becton Dickinson, San Jose, CA); anti–L-selectin (MEL-14).10Streptavidin-phycoerythrin (PE; Caltag, San Francisco, CA) was used as a secondary reagent in FACS analyses. The following additional MoAbs were used in in vivo blocking studies: anti–E-selectin (9A9),26 blocking anti–P-selectin (anti-PB; 5H1),5 nonblocking anti–P-selectin (anti-PNB; 10A10),5 kindly provided by Dr B. Wolitzky, Hoffman-LaRoche, Inc, Nutley, NJ; anti–L-selectin (MEL-14),10 anti–VLA-4 (PS-227; kind gift of Dr P. Kincade, Oklahoma Medical Research Foundation, Oklahoma City, OK); anti-CD44 (KM81)28 and anti-CD45RB(MB23G2)29 were obtained from the American Type Culture Collection (Manassas, VA). Antibodies were affinity purified from culture supernatants using protein-G-Sepharose according to the manufacturer’s instructions (Sigma).
CHS and acute nonspecific irritant responses.
CHS responses were induced in wild-type mice using DNFB as previously described.30,31 Twenty-five microliters of 0.5% DNFB in 4:1 acetone:olive oil solution was painted on the shaved abdomens of mice on days 0 and 1. Mice were challenged on day 5 by topical application of 20 μL of 0.2% DNFB (10 μL per side of the pinna). CHS responses in L-selectin–deficient mice were induced using DNBS haptenated splenocytes, as described.23 Mice were immunized subcutaneously with 2 × 107 haptenated spleen cells at two sites on the dorsum and were challenged on day 5 as described above. For all CHS experiments, baseline ear thicknesses were determined with a Fowler caliper (Lux Scientific Instrument Corp, New York, NY) before sensitization. Ear swelling responses were measured at 24 hours after elicitation, and the change in ear thickness from baseline measurement was computed. Each ear was measured five times and the mean of these values was used. Statistical analysis was performed using the Student’s t-test for pairwise comparison between groups and P values less than .05 were considered to be statistically significant.
Croton oil was used to cause nonspecific inflammation, as described.23 32 Ten microliters of 0.8% croton oil in acetone was painted onto the pinna. The change in ear thickness from baseline was measured at the indicated times as described for CHS responses.
MoAbs were used to block nonspecific irritant and DNFB-induced CHS ear swelling responses. Purified MoAb was administered intraperitoneally in a single dose of 200 μg/mouse in 500 μL of RPMI immediately after challenge with either croton oil or DNFB. Ear swelling responses were determined as described above. In experiments using multiple antibodies, 200 μg of each MoAb was used.
Immunofluorescence analysis of peripheral blood granulocytes.
Twenty-five microliters of peripheral blood obtained by tail bleed at indicated time points was collected into Alsever’s solution (114 mmol/L dextrose, 27 mmol/L sodium citrate, 71 mmol/L NaCl, pH 6.1). Cells were incubated with saturating amounts of biotinylated anti–GR-1 MoAb in 50 μL phosphate-buffered saline (PBS)/5% fetal calf serum (FCS) for 20 minutes on ice and then washed with 3 mL of PBS/5% FCS. Streptavidin-PE was added for 20 minutes, cells were again washed, and red blood cells were lysed in NH4Cl lysis buffer (0.15 mmol/L NH4Cl, 1.0 mmol/L KHCO3, 0.1 mmol/L EDTA, pH 7.2). Data were collected on a FACScan analytical instrument (Becton Dickinson, San Jose, CA) and analyzed using CELLQuest software.
Immunohistochemistry.
Ears were severed from euthanized mice, embedded in OCT compound, and frozen. Serial cryostat sections were fixed in methanol and stained with biotinylated anti–GR-1, anti–Mac-1, or anti-Thy1.2 as described.23 Briefly, after incubation with antibody, sections were rinsed with PBS and Streptavidin-horseradish peroxidase was added. 1× DAB (0.5 μg/mL diaminobenzidene) and 0.03% H2O2 in 50 mmol/L TrisHCl were added for 10 minutes and slides were washed in PBS/0.5% CuSO4 and counterstained with methylene blue.
RESULTS
P- and E-selectin, but not L-selectin, are critical in a nonspecific irritant response.
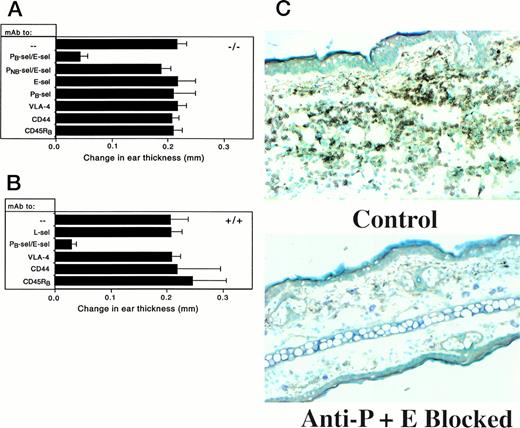
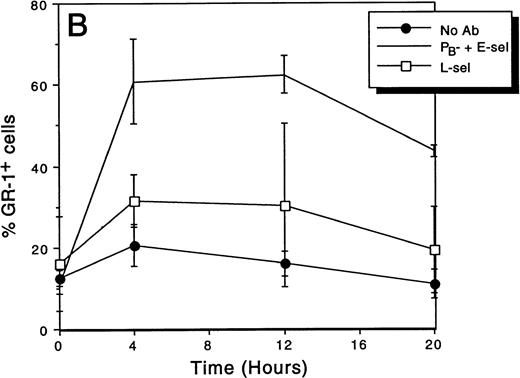
The role of key adhesion molecules in a croton oil-induced irritant inflammatory response was investigated by examining the inhibition of neutrophil migration in both L-selectin–deficient and wild-type mice. In the background of L-selectin–deficient mice (−/−), no defect in responsiveness was previously noted,23 and neither a blocking anti–P-selectin nor a blocking anti–E-selectin MoAb alone was able to significantly block ear swelling (Fig 1). In addition, a combination of a nonblocking anti–P-selectin with a blocking E-selectin antibody also had no significant effect. However, the combination of blocking anti–P-selectin plus anti–E-selectin was able to inhibit ear swelling from 80% to 90% in both wild-type and L-selectin–deficient mice, indicating the very strong dependence of leukocyte recruitment on a combination of these adhesion molecules. Additionally, MoAbs to VLA-4, a molecule generally involved in secondary adhesion, or to CD44, previously reported to be involved in an antigen-specific contact hypersensitivity response,33 were also ineffective in inhibiting ear swelling, as was also true of the additional isotype control anti-CD45RB. In wild-type mice (+/+), it is additionally notable that anti–L-selectin had no effect on croton oil induced ear swelling, consistent with the normal ear swelling response seen in the knockout mice. Together, the data strongly suggest that L-selectin is not critical to a nonspecific irritant response and that results in L-selectin–deficient mice do not result from the supervention of compensatory adhesion mechanisms. Thus, among the adhesion molecules tested, only a combination of P- and E-selectin appears to be involved in this acute inflammatory ear swelling response.
Change in ear swelling induced in L-selectin–deficient (A) and wild-type (B) mice by the nonspecific irritant croton oil. Sixteen hours after croton oil application, the combination of blocking anti–P-selectin (PB) plus anti–E-selectin was able to significantly reduce ear swelling in both strains of animals (P< .001 compared with no antibody). Nonblocking anti–P-selectin (PNB) in combination with anti–E-selectin had no effect. L-selectin–deficient mice had ear swelling comparable to that of wild-type animals and anti–L-selectin treatment had no effect on ear swelling in +/+ mice. Each treatment group contained ≥5 animals. (C) Neutrophil infiltrate into croton oil-treated ears is blocked by anti–P-plus anti–E-selectin. Sixteen hours after the application of croton oil to ears of wild-type mice, immunohistochemical staining of ear sections with anti–GR-1 was performed. Cells stained brown are positive for the marker (original magnification × 400). Combined anti-endothelial selectin antibodies show a substantial diminution of both GR-1 staining and ear swelling. L-selectin–deficient mice treated in the same manner showed identical staining patterns (data not shown).
Change in ear swelling induced in L-selectin–deficient (A) and wild-type (B) mice by the nonspecific irritant croton oil. Sixteen hours after croton oil application, the combination of blocking anti–P-selectin (PB) plus anti–E-selectin was able to significantly reduce ear swelling in both strains of animals (P< .001 compared with no antibody). Nonblocking anti–P-selectin (PNB) in combination with anti–E-selectin had no effect. L-selectin–deficient mice had ear swelling comparable to that of wild-type animals and anti–L-selectin treatment had no effect on ear swelling in +/+ mice. Each treatment group contained ≥5 animals. (C) Neutrophil infiltrate into croton oil-treated ears is blocked by anti–P-plus anti–E-selectin. Sixteen hours after the application of croton oil to ears of wild-type mice, immunohistochemical staining of ear sections with anti–GR-1 was performed. Cells stained brown are positive for the marker (original magnification × 400). Combined anti-endothelial selectin antibodies show a substantial diminution of both GR-1 staining and ear swelling. L-selectin–deficient mice treated in the same manner showed identical staining patterns (data not shown).
Immunohistochemical staining of ear sections from mice treated with croton oil show predominantly infiltrates of neutrophils.23As with ear swelling, only the combination of blocking antibodies to P- and E-selectin was able to significantly diminish the number of infiltrating cells (Fig 1C and Table 1). The dramatic inhibition of infiltrating cells with combined anti-endothelial selectin antibodies also suggests that the slight residual swelling after such treatment may not be due to inflammatory cell emigration, but rather to edema more directly caused by the irritant chemical. These data thus demonstrate that both P- and E-selectin are essential for the recruitment of neutrophils in an irritant response and that L-selectin does not significantly contribute, when assessed either by antibody blockade in normal mice or in knockout mice.
Ear swelling response in L-selectin–deficient mice is not temporally altered from wild-type and is blocked throughout by combined P- and E-selectin MoAbs.
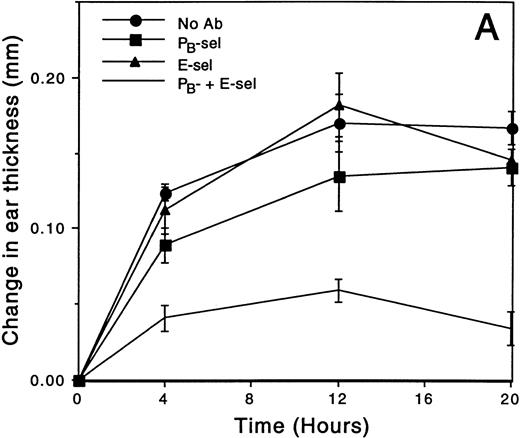
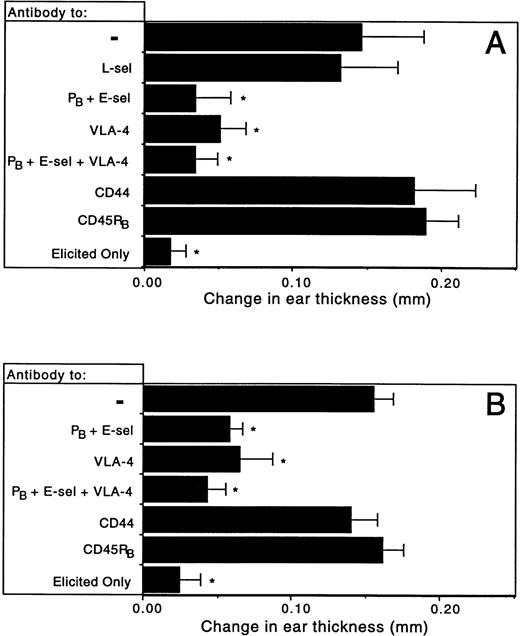
Some adhesion molecules, such as P-selectin, can be rapidly mobilizable on endothelium upon stimulation and may serve as the initial ligand for infiltrating cells during tissue damage and inflammation.3In contrast, E-selectin is upregulated more gradually and also serves as a ligand for emigrating leukocytes.3,34 35 Because the upregulation of adhesion molecule expression on endothelium may be sequential and could be additionally altered in L-selectin–deficient mice, it was possible that animals treated with MoAb would show differential ear swelling at different time points during the course of the response. At all time points, the decrease in ear swelling with combined anti-endothelial selectin MoAbs was dramatic in both −/− and +/+ mice (Fig 2). Although treatment with anti–P-selectin alone resulted in slight inhibition in mutant mice, only the 12-hour time point showed ear swelling that was significantly less than that of untreated animals or those treated with anti–E-selectin (P = .023; Fig 2A). Anti–L-selectin treatment of wild-type mice had no effect in reducing ear swelling at any time point (Fig 2B). Thus, although E-selectin appears to have no independent role in ear swelling, P-selectin alone may make a small contribution. However, E- and P-selectin clearly act synergistically in ablating the formation of the ear swelling response and together appear to be involved in neutrophil recruitment, even at early time points.
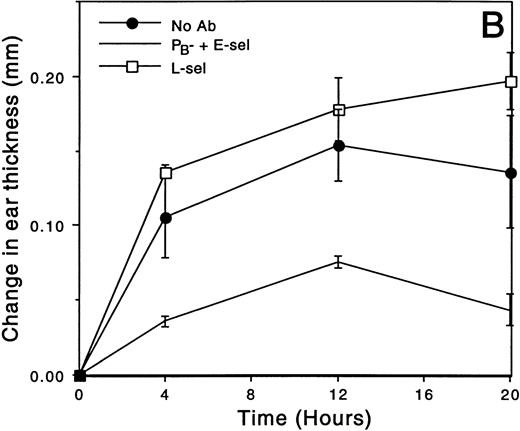
The effect of MoAb treatment on croton oil-induced ear swelling throughout the response. (A) The change in ear swelling of L-selectin–deficient mice. At each time point, mice treated with combined anti-PB plus anti–E-selectin are significantly different from each of the other treatment groups (all pairwise comparisons P < .001). (B) The change in ear swelling of wild-type mice. Anti-PB- plus anti–E-selectin inhibits ear swelling at each time point (P < .005 compared with no antibody control), whereas anti–L-selectin has no effect. Data are from a representative experiment (n ≥ 3 mice/time point).
The effect of MoAb treatment on croton oil-induced ear swelling throughout the response. (A) The change in ear swelling of L-selectin–deficient mice. At each time point, mice treated with combined anti-PB plus anti–E-selectin are significantly different from each of the other treatment groups (all pairwise comparisons P < .001). (B) The change in ear swelling of wild-type mice. Anti-PB- plus anti–E-selectin inhibits ear swelling at each time point (P < .005 compared with no antibody control), whereas anti–L-selectin has no effect. Data are from a representative experiment (n ≥ 3 mice/time point).
Inflammatory response correlates with elevated granulocytes in peripheral blood.
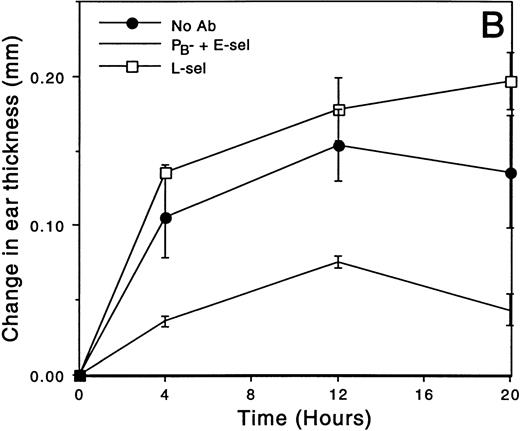
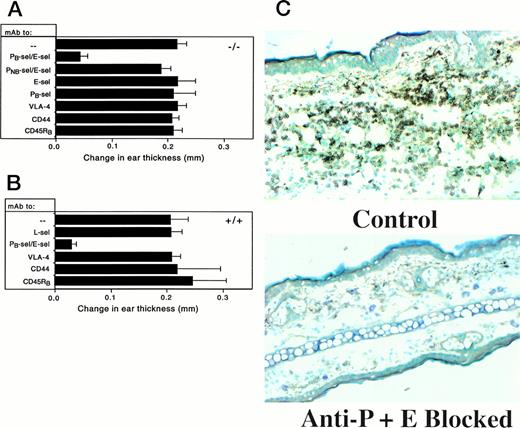
Elevated neutrophil counts have been shown to be characteristic of P- and P/E-selectin–deficient mice.4 36 We therefore examined whether the inhibition of neutrophil migration into an inflamed site correlated with the accumulation of GR-1 positive cells in the peripheral blood of mice treated with MoAb during their response to croton oil. Figure 3 demonstrates the percentages of GR-1+ cells in peripheral blood for each MoAb-treated group of mice over a 20-hour time course. For both −/− and +/+ mice, the percentage of granulocytes in the peripheral blood increased in the initial 4 hours and then gradually decreased during the remainder of the course of the response, generally inversely related to what was observed in the amount of ear swelling seen at each time point. Combined anti-endothelial selectin antibodies increased the level of circulating GR-1+ cells in L-selectin–deficient animals to an average of 69% by 12 hours posttreatment, consistent with the inability of circulating leukocytes to marginate and enter the site, compared with 15% in animals treated with croton oil but not antibody (Fig 3A). Likewise, by the 12-hour time point, wild-type animals treated with P- plus E-selectin antibodies showed a fourfold increase in the percentage of circulating GR-1+ cells, compared with animals not receiving antibody (P < .001; Fig 3B). Combined anti-endothelial selectins also had a greater effect on numbers of circulating granulocytes than either anti–P-selectin or anti–E-selectin treatment alone in −/− mice (Fig 3A). However, anti–P-selectin alone also has a moderate but significant effect compared with croton oil only treated animals (P < .03 at each time point), consistent with ear swelling data, whereas anti–E-selectin only treatment did not. The striking increase in the percentage of circulating granulocytes in anti–P- plus anti–E-selectin treated mice further suggests that these antibodies indeed act through blocking of extravasation is entirely consistent with elevated circulating leukocytes in P/E-selectin–deficient mice and further demonstrates the cooperative effect of these molecules in the recruitment of cells into an inflamed site.
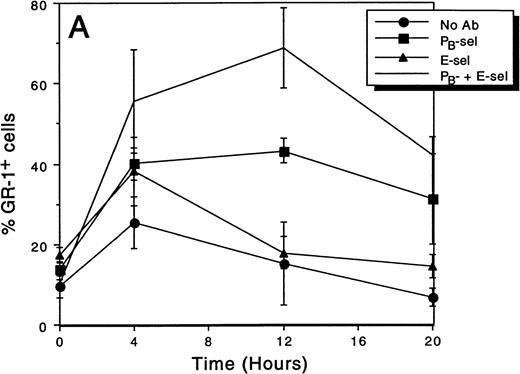
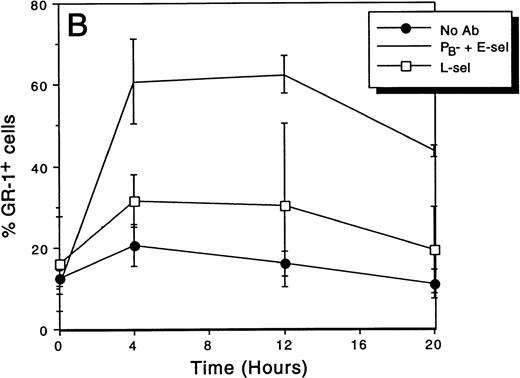
The effect of MoAb treatment on the percentage of granulocytes in peripheral blood after croton oil application to the ears. Blood for FACS analysis was collected at indicated time points after the application of croton oil and injection of antibody. (A) L-selectin–deficient mice: Mice treated with combined endothelial selectin antibodies have significantly increased neutrophils at each posttreatment time point (P < .03 compared with control). By 20 hours, the percentage of circulating neutrophils is decreasing in all animals. (B) Wild-type mice: combined anti-endothelial selectin antibody increases the percentage of circulating granulocytes at each time point (P < .005 compared with control). Anti–L-selectin treatment does not significantly affect circulating granulocyte percentages.
The effect of MoAb treatment on the percentage of granulocytes in peripheral blood after croton oil application to the ears. Blood for FACS analysis was collected at indicated time points after the application of croton oil and injection of antibody. (A) L-selectin–deficient mice: Mice treated with combined endothelial selectin antibodies have significantly increased neutrophils at each posttreatment time point (P < .03 compared with control). By 20 hours, the percentage of circulating neutrophils is decreasing in all animals. (B) Wild-type mice: combined anti-endothelial selectin antibody increases the percentage of circulating granulocytes at each time point (P < .005 compared with control). Anti–L-selectin treatment does not significantly affect circulating granulocyte percentages.
Analysis of adhesion molecules required for a DTH response.
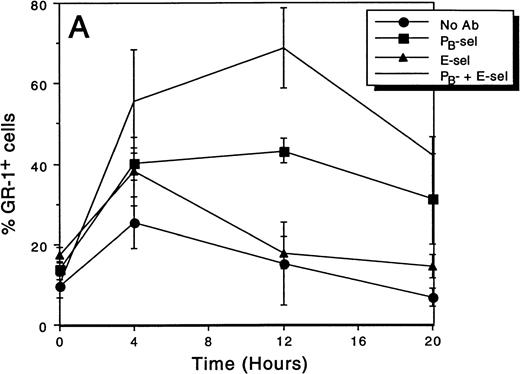
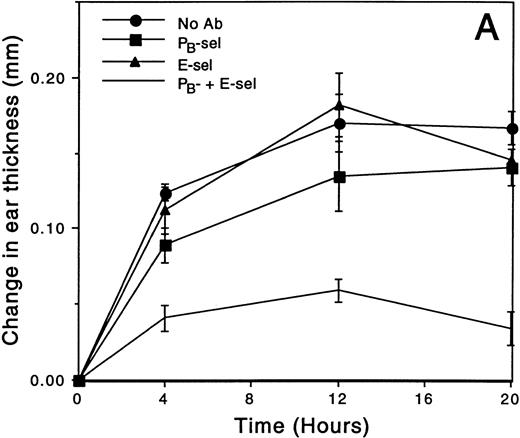
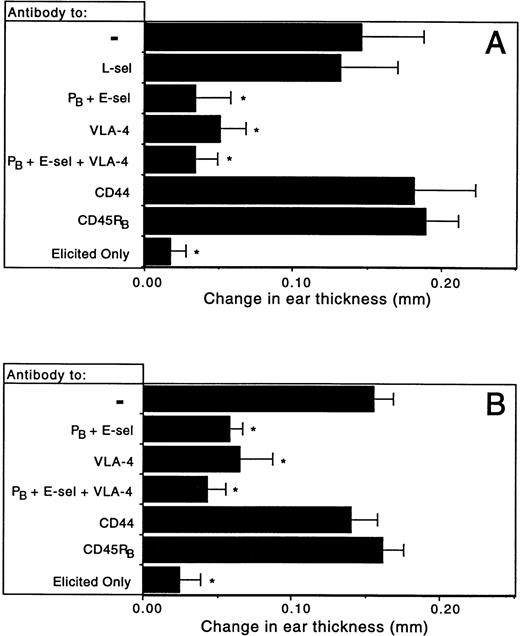
To examine leukocyte recruitment into a site of antigen-specific dermatitis, DTH was induced using DNFB. Because L-selectin–deficient mice cannot be sensitized via topical immunization, they were sensitized subcutaneously with DNBS haptenized spleen cells, which results in DTH swelling and cellular infiltrates indistinguishable from those of wild-type mice sensitized in the same way or via topical sensitization with hapten.23 The amount of ear swelling in response to cutaneous challenge with DNFB was determined with or without MoAb treatment administered at the time of challenge on the ear, ie, during the effector arm. As with the acute irritant response, antibodies to the endothelial selectins in combination most dramatically inhibited the ear swelling associated with contact dermatitis (Fig 4). Combined anti-endothelial selectin treatment resulted in a 75% to 90% decrease compared with untreated and antibody control animals in both wild-type and knockout mice over elicitation alone. However, in contrast to the results obtained with the croton oil response, antibody to VLA-4 resulted in a decrease in the CHS response comparable to blocking endothelial selectins, indicating a role for α4 integrins in the extravasation pathway in an antigen-specific response. When antibodies to both endothelial selectins were combined with anti–VLA-4, no significant additional inhibition of ear swelling was seen over selectin antibodies alone in either type of animal. Although the effects of antibody treatment in L-selectin–deficient and wild-type mice were generally similar, the inhibitory effects by antibodies in L-selectin–deficient animals appear slightly blunted compared with wild-type, although this is not statistically significant. The results nonetheless suggest that E- and P-selectin together play a vital role in the mounting of a contact hypersensitivity response in normal mice and, in contrast to ear swelling induced by an irritant, VLA-4 appears to have an equally important role in an antigen-specific response. Antibody to L-selectin had no effect in this system; anti-CD44 also had no effect in either knockout or wild-type animals, although it has been reported by others to have an inhibitory effect in a CHS response.33
Antibody blocking of a CHS ear swelling response to DNFB. Mice were treated as described and ears were measured 24 hours after elicitation. (A) Wild-type mice: combined anti-endothelial selectin antibody significantly reduces antigen-specific ear swelling compared with both untreated and anti-CD45RB control treated animals. Antibody to VLA-4 is equally effective, whereas neither anti–L-selectin nor anti-CD44 treatment has any effect. (B) L-selectin–deficient mice: treatment with combined anti-endothelial selectin or anti–VLA-4 significantly reduces ear swelling. Anti-CD44 and control anti-CD45RB have no effect. n ≥ 4 for each treatment group. *P < .001 compared with both untreated and anti-CD45RB control treated animals.
Antibody blocking of a CHS ear swelling response to DNFB. Mice were treated as described and ears were measured 24 hours after elicitation. (A) Wild-type mice: combined anti-endothelial selectin antibody significantly reduces antigen-specific ear swelling compared with both untreated and anti-CD45RB control treated animals. Antibody to VLA-4 is equally effective, whereas neither anti–L-selectin nor anti-CD44 treatment has any effect. (B) L-selectin–deficient mice: treatment with combined anti-endothelial selectin or anti–VLA-4 significantly reduces ear swelling. Anti-CD44 and control anti-CD45RB have no effect. n ≥ 4 for each treatment group. *P < .001 compared with both untreated and anti-CD45RB control treated animals.
During a CHS response, it is believed that antigen-specific T cells are first recruited into the site in response to antigen and that their recruitment causes the release of additional cytokines and activators that mediate the subsequent recruitment of nonspecific effector cells such as monocytes and granulocytes.37 38 To characterize the cells recruited after topical challenge with DNFB, serial sections of elicited ears from animals treated with antiadhesion receptor MoAbs were examined to determine the composition and extent of the infiltrates. Table 2 shows that, in wild-type mice treated with either combined anti-endothelial selectins or with anti–VLA-4, there is a severe reduction in the number of both GR-1+ and Mac-1+ cells, as well as those expressing Thy1.2. Moreover, mice treated with either anti–VLA-4 or the anti-endothelial selectins in combination were essentially indistinguishable from each other with respect to the extent and composition of the infiltrate. Nonblocking anti–P-selectin in combination with anti–E-selectin had no effect on the extent or type of infiltrate; anti–L-selectin or anti-CD44 also had no effect. It is therefore apparent that the effect of adhesion blockade is both on the swelling response as well as on both early (T) and late (monocyte and granulocyte) inflammatory cell recruitment.
DISCUSSION
The involvement of L-selectin in the trafficking of leukocytes to sites of antigen-specific and nonspecific inflammation is complicated in part by the contribution and overlapping functions of the endothelial selectins. It has nonetheless been shown in vitro and in vivo within venules, particularly after cytokine activation, that neutrophil and monocyte rolling can be L-selectin–dependent.16,39-42 A role for L-selectin in inflammation is further supported by a number of studies that have reported that leukocyte recruitment into various inflammatory sites, including lung,43 skin,44and peritoneum,13,17,45 can be lessened by treatment with anti–L-selectin antibodies. In addition, L-selectin–deficient mice have been reported to exhibit defects in recruitment to a site of peritoneal inflammation19 and to sites of DTH, including a CHS response.23-25 Because of the conflicting reports on the requirements for L-selectin during inflammation and because our evidence in L-selectin–deficient mice indicated that effector mechanisms were completely intact in CHS and skin irritant responses, we sought to examine in detail which are the relevant adhesion molecules in these models and also to explore whether other mechanisms may compensate for L-selectin in our mutant animals compared with normal mice. The evidence presented here indicates that both wild-type mice treated with anti–L-selectin antibodies and L-selectin–deficient mice show no substantial differences in effector mechanisms and in the recruitment of leukocytes into the skin in either an acute or chronic inflammatory model. This evidence is consistent with an intravital study showing a lack of L-selectin involvement in recruitment to noninflamed dermal vessels.46 The concordance of the neutralizing antibody and mouse mutant studies indicate that L-selectin does not play a significant role in the recruitment of nonspecific effector elements in the models of skin inflammation studied.
In both of these inflammatory models, antibodies to P- and E-selectin were required in combination to optimally block the ear swelling response and recruitment of inflammatory cells, consistent with the known cooperativity and overlapping functions of these molecules. Thus, in an acute irritant response, these antibodies in combination inhibited virtually all of the predominantly granulocytic infiltrate, as well as the more heterogeneous infiltrate in a CHS response. These neutralizing antibody studies are fully confirmatory of gene targeting methods, which have indicated a requirement for both P- and E-selectin in a CHS response.7 In mutant mice, sensitization and effector phases are not separable; therefore, studies in them do not distinguish the stage at which the molecules are required. In these studies, neutralizing antibodies were administered only during the effector phase of the response, giving a more direct demonstration of the impact of the loss of P- and E-selectin function on effector cells and mechanisms. These studies further reinforce the preeminent roles of P- and E-selectin at this inflammatory site.
One interpretive concern in P/E-selectin double mutants was that the L-selectin surface density on all leukocytes was markedly diminished, which is thought to be due to cell activation, and that this could have significantly contributed to defects in inflammatory cell recruitment.8 Moreover, residual ear swelling found in these mutants,7 as well as in E-selectin–deficient mice,5 had been suggested to derive from the participation of L-selectin. Although L-selectin has been demonstrated to serve as a major ligand on neutrophils for E-selectin in the human,20,21 this has recently been demonstrated not to be the case in mice,21 consistent with our results showing no impact of the loss of L-selectin in these murine models. However, because LADII patients have been reported to mount antigen-specific T-cell recruitment to the skin comparable to normal individuals,47 it is clear that the situation is more complex in the human and that other adhesion pathways not involving selectins or their traditional ligands may be used. L-selectin has further been shown to potentially contribute to and augment inflammatory cell recruitment via neutrophil/neutrophil interactions,22 but again, such augmentation does not appear necessary under the conditions used here. Thus, our evidence alleviates the concerns about L-selectin in the previous studies of selectin knockout mice and suggests that L-selectin does not represent a significant contributor to the observations in CHS responses using such mice.
To assess whether selectins contributed differentially over time during the course of a response, we examined the effect of antibody treatment on an acute irritant response at intervals over its course. E-selectin expression on human umbilical vein endothelial cells (HUVEC) has been shown to peak between 3 to 6 hours after stimulation with tumor necrosis factor α.35 P-selectin is also induced by proinflammatory stimuli and is thought to be important at later as well as very early time points of cell recruitment.48,49 Therefore, defects in trafficking might be more apparent at different times when inhibiting these various adhesion molecules. However, anti–E-selectin had no significant effect at any interval in an acute irritant response, and the modest effect of anti–P-selectin did not appear accentuated at any point. P-selectin–deficient mice have previously been shown to demonstrate only slight effects on ear swelling (diminished, but not significantly so) with a significant inhibition of inflammatory cell recruitment.6 Our results similarly showed a modest decrease in ear swelling with anti–P-selectin, and at the 12-hour point the differences were statistically significant (Fig 2). In any case, even at the earliest time point of 4 hours, the synergistic effect of both anti–E- and anti–P-selectin is evidenced by the marked decrease in ear swelling (Fig 2) as well as the increase in the percentage of circulating granulocytes when compared with anti–P-selectin treated or control mice (Fig 3). Thus, it appears that the coordinated function of P- and E-selectin in an acute irritant response has its onset early and continues throughout the response.
Integrins containing the α4 chain have been shown to be quite versatile with respect to the adhesion cascade and are able to mediate tethering and rolling50-52 as well as firm arrest.53 VLA-4 is expressed on T cells, monocytes, eosinophils, and, in some studies, neutrophils and has been shown to have a role in many inflammatory models involving all of these cell types.54-60 In these studies, a blocking anti-α4 antibody was able to inhibit the preponderance of an antigen-specific response (Fig 4A and B), but had no effect on an acute response at the same site (Fig 1). Despite potential expression on numerous inflammatory cell types, our evidence for a role for this molecule at a single anatomic site, cutaneously on the ear, in an antigen-specific response only is highly suggestive that the inhibition in these studies operates at the level of effector T cells. Furthermore, analysis of the infiltrate present after a CHS response in the ears of antibody-treated mice demonstrated that T cells as well as the nonspecific effector elements are dramatically reduced with anti–VLA-4 treatment (Table 2), further supporting this interpretation. However, we cannot formally rule out that the activation state of α4 on monocytes and/or neutrophils differs between these cutaneous models or that different subpopulations of these cells could be involved under the two circumstances. Our analysis agrees with previous use of VLA-4 antibodies in CHS studies using oxazolone or DNFB in Balb/c mice,61,62 and the major cell surface VLA-4 ligand VCAM-1 has been implicated in DTH in a primate model.63 In a rat model of skin DTH, although significant inhibition was seen with anti–VLA-4 MoAbs, both anti–VLA-4 and LFA-1 were required to maximally block in vivo.64 It should be cautioned that in addition to direct ligand blocking, anti–VLA-4 can also have intracellular signaling effects,65-68 and such secondary effects in these studies cannot be ruled out. The extent of the effect both on ear swelling and cellular infiltration with anti-α4 that we saw was similar to that using both endothelial selectin antibodies, and the use of both the endothelial selectin antibodies plus anti-α4 did not result in a significantly greater decrease in ear swelling or infiltrates, suggesting again that these antibodies do not act in independent pathways. Thus, whereas anti–VLA-4 treatment appears to have no effect on the recruitment of neutrophils into an antigen-independent site of acute inflammation, it does inhibit the majority of an antigen-specific DTH response, supporting the contention that anti–VLA-4 blocks the entry of T cells, which are in turn necessary for the recruitment of nonspecific effector cells.
We have recently demonstrated that CD44 can mediate the primary adhesion of T lymphocytes to endothelium expressing its principal ligand hyaluronate (HA),69 that the activation of CD44 to bind HA is induced via TCR signaling,70 and that extravasation of such activated T cells in an in vivo model of peritoneal inflammation is critically dependent on T-cell CD44 interactions with HA.71 It is therefore of particular interest that use of the HA-blocking anti-CD44 MoAb, KM81, results in no decrease or delay in either the acute irritant or the CHS response when used either alone (Figs 1 and 4) or in conjunction with other antibodies (data not shown). This is in contrast to previous reports in which an inhibitory effect on CHS responses to DNFB was found.33 It is possible that the antibodies used in those studies may have had additional significant cell surface modulating and/or signaling effects on those cells. Such modulation in our experience is considerably reduced with KM81. Furthermore, it has recently been reported that mice in which CD44 has been disrupted by gene targeting show no defect in CHS responses,72consistent with our results. Thus, although it is clear that the CD44/HA interaction can be important for aspects of effector T-cell extravasation, this may not be the case at the particular site of the skin in mice. Because Th1 helper cells entering the skin are in fact dependent on P- and E-selectin,73 additional primary adhesion mechanisms may not be required at this site.
It has become clear that caution must be exercised in interpreting phenotypes of mice with disrupted adhesion molecule genes. Whereas E-selectin knockouts displayed a relatively mild phenotype,5 the importance of this molecule and its close cooperativity with P-selectin was made apparent after using P-selectin blocking MoAbs in these mice, and particularly after the development of P/E-selectin double knockout mice.4,8 It is further possible that compensatory mechanisms may supersede under circumstances of genetically deficient animals, and discrepancies have been noted between antibody blocking studies and observations in knockout mice. For instance, in models of acute lung injury, analysis of mice deficient in ICAM-1, P-selectin, or both led to significantly different conclusions than using blocking antibodies to these molecules in both a cobra venom factor-induced lung injury model and Pseudomonas infection.74 75 Thus, the use of both approaches can be quite informative. In using a combination of L-selectin–deficient mice and blocking MoAb in wild-type mice, we found complete concordance of results between our own or previous knockout mouse studies and the use of blocking MoAbs in two standard models of skin inflammation, further underscoring the necessity for examined such issues on a case by case basis.
In summary, these studies examine within a single system the major adhesion molecules contributing to an acute irritant as well as a CHS response using a combination of mice genetically deficient in L-selectin and antibody blockade. The evidence emphasizes (1) the crucial importance of the P- and E-selectin collaboration to these responses, (2) that L-selectin does not contribute to the effector phase of either of these responses in a significant way by either antibody blockade or knockout approaches, (3) that VLA-4 appears central to an antigen-specific but not acute irritant response at skin sites, and (4) that, although caution must be used in using knockout models, antibody blockade and knockout approaches gave quite similar results in these studies.
ACKNOWLEDGMENT
The authors thank Dr Barry Wolitzky (Hoffman-LaRoche, Inc, Nutley, NJ) for kindly providing anti–P- and anti–E-selectin reagents and Helen Arizpe for technical assistance.
Supported by grants from the National Institutes of Health (Grants No. CA57571 and HL56746), the Welch Foundation (I-227), the Arthritis Foundation, and the Texas Higher Education Coordinating Board (003660-076). M.H.S. is an Established Investigator of the American Heart Association. M.D.C. was a student in the Graduate Program of Immunology in the Graduate School of Biomedical Sciences, UTSWMCD.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Mark Siegelman, MD, PhD, Department of Pathology, University of Texas Southwestern Medical Center at Dallas, 5323 Harry Hines Blvd, Dallas, TX 75235-9072; e-mail:siegelman@utsw.swmed.edu.