Background: Autologous CD19 CAR T cell therapies have demonstrated favorable clinical responses in relapsed or refractory (R/R) diffuse large B-cell lymphomas (DLBCL), but only a subset of patients (pts) experience durable remissions. We hypothesized that the redundancy of CD28 and CD3ζ signaling in a CAR design incorporating all 3 CD3ζ immunoreceptor tyrosine-based activation motifs (ITAMs) might negatively affect T cell differentiation and promote exhaustion. Therefore, we created a new CD19 CAR construct with calibrated CAR activation potential by mutating 2 of the 3 ITAMs, termed 1XX, and hypothesized that a 1XX CAR would afford durable responses at lower dose and fewer toxicities compared to CARs comprising 3 ITAMs. We previously presented the data from the dose-escalation portion of the phase I clinical trial of 19(T2)28z-1XX CAR T cells in DLBCL (Park J et al. ASH 2022). We have now completed accrual and report the updated results from both dose escalation and expansion portion of the study with a longer follow-up (NCT04464200).
Methods: This is a single-center, phase I, dose-escalation and expansion trial of 19(T2)28z1XX CAR T cells in adult pts with R/R DLBCL conducted at Memorial Sloan Kettering Cancer Center. Pts received fludarabine and cyclophosphamide lymphodepleting chemotherapy followed by a single infusion of CAR T cells. There were 4 dose levels in the dose escalation cohort: dose level (DL) 1 (25x10 6), DL2 (50x10 6), DL3 (100x10 6) and DL4 (200x10 6 CAR T cells). The primary objective of the trial was to evaluate safety and tolerability and determine the recommended phase 2 dose. Key secondary objectives include assessment of overall response and complete response rates.
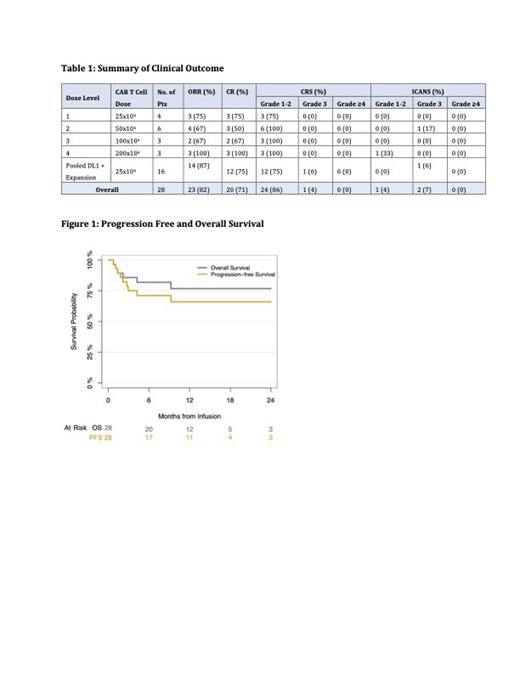
Results: 28 pts have been enrolled and treated; 16 pts on the dose escalation and 12 pts on the dose expansion phase of the study. Median age was 62 (range, 48-86). 20 pts (71%) had primary refractory disease, 3 pts (11%) had prior autologous HSCT, and 2 pts (7%) had prior autologous CD19 CAR T therapy. In the dose-escalation phase (n=16), 15 pts experienced grade 1-2 CRS (94%) and no pt experienced ≥grade 3 CRS. Two pts (13%) experienced ICANS: 1 pt with grade 1 and 1 pt with grade 3 (Table 1). Eight pts received tocilizumab and 5 pts received corticosteroid. Complete response (CR) was observed in 11 of 16 pts (69%) and partial remission (PR) in 1 pt (6%) with overall response rate (ORR) of 75%. Responses were seen across all dose levels (Table 1). The lowest dose (DL1: 25x10 6) was selected for dose-expansion based on exposure-response analysis and 12 additional pts were treated at that dose level. In a pooled analysis of 16 pts who received DL1 dose (4 in dose escalation and 12 in dose expansion), 12 pts and 1 pt experienced grade 1-2 (75%) and grade 3 CRS (6%), respectively. Only 1 pt experienced ICANS (6%) at grade 3 (same pt who had grade 3 CRS), which was reversible and transient (Table 1). 11 pts received tocilizumab and 9 pts received corticosteroids. Twelve pts achieved CR (75%) and 2 pts (12%) PR with the best ORR of 87% (Table 1). A lower metabolic tumor volume (MTV) at screening but not at post-bridging was associated with a higher likelihood of achieving CR (p=0.039). With a median follow-up of 345 days (range, 33-1024), 4 pts experienced relapse (1 CR and 3 PR pts) and 16 pts have ongoing CR > 6 months (Figure 1). While CAR T cell persistence analysis is ongoing, 5 pts have CAR T cells detected beyond one year in ongoing CR including a patient treated at DL1 with detectable CAR T cells at 2 years.
Conclusions: Treatment with 19(T2)28z1XX CAR T cells was shown to be safe with durable remissions with low rates of severe CRS (4%) and ICANS (7%). The overall CR rate of 71% is encouraging and appears durable with the majority of CR patients in ongoing remission > 6 months at a median follow-up of 345 days and with persisting CAR T cells. With more patients treated at DL1 with a longer follow-up, the study demonstrates a high efficacy of 19(T2)28z1XX CAR T cells at a dose significantly lower (25x10 6) than those of approved CD19 CAR T cells (100-300x10 6) and support that the 1XX single ITAM signaling domain may lead to enhanced efficacy of CD19 CARs and allow infusion of a lower T cell dose with favorable toxicity profiles.
OffLabel Disclosure:
Park:Autolus Therapeutics: Research Funding; Curocell: Consultancy; Affyimmune: Consultancy; Amgen: Consultancy; Genentech, Inc.: Research Funding; Artiva Biotherapeutics: Consultancy, Current holder of stock options in a privately-held company, Membership on an entity's Board of Directors or advisory committees; Bright Pharmacetuicals: Consultancy; Be Biopharma: Consultancy; BeiGene: Consultancy; Fate Therapeutics: Research Funding; Servier: Consultancy, Research Funding; Allogene: Consultancy, Membership on an entity's Board of Directors or advisory committees; Intella: Consultancy; Incyte: Research Funding; Takeda: Consultancy, Research Funding; GC Cell: Membership on an entity's Board of Directors or advisory committees; Sobi: Consultancy, Research Funding; Pfizer: Consultancy; Kite: Consultancy; Minerva Bio: Consultancy. Palomba:MustangBio: Honoraria; Seres Therapeutics: Honoraria, Patents & Royalties; Rheos: Honoraria; Novartis: Honoraria; Pluto Immunotherapeutics: Honoraria; Synthekine: Honoraria; GarudaTherapeutics: Honoraria; Smart Immune: Honoraria; Thymofox: Honoraria; Kite: Honoraria; Juno: Honoraria, Patents & Royalties; Ceramedix: Honoraria; Cellectar: Honoraria; BMS: Honoraria. Valtis:EastRx: Consultancy. Schoder:Aileron Therapeutics: Honoraria. Li:Takeda: Current Employment. Sellner:Takeda: Current Employment. Mansilla-Soto:Takeda: Patents & Royalties: Licensed patents. Riviere:Takeda Development Center Americas, Inc.: Current Employment, Current equity holder in publicly-traded company. Sadelain:Takeda: Research Funding; Minerva: Current equity holder in private company; Atara: Research Funding; Mnemo: Current equity holder in private company, Research Funding; Fate: Research Funding.
19(T2)28z-1XX CAR T cells