Background:
Advancements in treatment have significantly improved therapeutic outcomes for pediatric acute lymphoblastic leukemia (ALL) and relapsed ALL. However, there remains a need for therapies that minimize relapse in high-risk groups and avoid long-term complications. To address this gap. we conducted the nationwide clinical trial ALL-B12, aimed at newly diagnosed B-precursor ALL aged 1-18 years.
Methods:
ALL-B12 enrolled participants from November 2012 to November 2017. Patients were stratified based on the NCI classification (age and WBC count at diagnosis). Those with NCI-SR and NCI-HR were assigned to the standard risk group (SR) and the intermediate group (IR), respectively. Poor steroid responders and those with high-risk genomic abnormalities were assigned to the high risk group (HR). A treatment regimen, including 4-drug remission induction, early consolidation, HD-MTX-containing intensification, re-induction, and maintenance, was implemented. Anthracycline dose in the induction therapy was reduced in SR patients. In contrast, early consolidation was intensified with L-ASP for a part (randomized) of the IR and the entire HR. Patients classified as CNS3 were treated as high risk, receiving 12 Gy cranial irradiation; prophylactic cranial irradiation was avoided in non-CNS3 groups. Allogeneic hematopoietic cell transplantation (allo-HCT) during the first remission was restricted to those in the very high-risk group with specific genomic abnormalities (e.g., hypodiploid <44 and TCF3-HLF) and residual MRD above 10^-3 at the end of early consolidation. A randomized comparison was carried out within each risk group to identify the optimal treatment. We assessed the effectiveness of intensification with VCR/DEX pulses for the SR, the impact of L-ASP intensification for the IR, and compared block-type treatment and HD-MTX intensified with VCR and L-ASP (HD-MTX/VL) for the HR. The primary outcome measure was the 5-year event-free survival (EFS) rate.
Results:
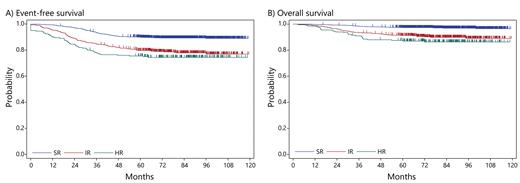
In total, 1,936 patients were enrolled, with 1,804 patients receiving protocol treatment after excluding ineligible patients such as those with BCR-ABL1 positivity. The percentage of patients achieving remission at the end of early consolidation was 98.9%. The overall 5-year EFS and OS probability were 85.2% (95%CI 83.5-86.8%) and 94.3% (95%CI 93.1-95.3%), respectively. Only 1.7% of patients underwent allo-HCT during the first remission. The mortality rate during induction was just 0.6%, with non-relapse mortality (NRM) after remission at 0.6%. The overall relapse incidence was 13.2%, and the overall CNS relapse rate was 1.9%. Among patients assigned to risk groups, 1,107 (62.7%) were assigned to the SR, 459 (26.0%) to the IR, and 200 (11.3%) to the HR. The 5yEFS for the SR was 89.9%. The post-randomization EFS rates for those with and without VCR/DEX intensification were 90.7% and 90.1%, respectively, indicating nearly identical survival curves (p = 0.73). The EFS for the IR was 79.7%, but L-ASP intensification was expected to be effective, the EFS for groups with and without ASP intensification was 82.1% and 77.9%, respectively, failing to reach statistical significance (p = 0.31). The EFS for the HR was 75.5%, with overlapping survival curves for block treatment (75.7%) and HD-MTX/VL (74.2%) (p = 0.92). MRD dynamics were associated with prognosis, and early consolidation therapy enhanced by ASP resulted in better MRD clearance. MRD of 10^-4 was associated with poor prognosis at both the end of induction and the end of early consolidation.
Conclusion:
In our multi-center clinical trial, we observed excellent outcomes in a diverse group of patients nationwide. Using the NCI criteria for stratification, a significant number of patients were categorized into the SR. Additionally, introducing L-ASP during early consolidation decreased the number of MRD-positive patients, which subsequently reduced the subset needing allo-HCT. This strategic adjustment in treatment intensity resulted in both high EFS rates and low NRM. Given the rise of immunotherapy and its promising results for recovery even post-relapse, there's a pressing need to enhance overall outcomes while minimizing non-relapse mortality. We anticipate refining our stratification further and integrating immunotherapy and other innovative treatments into our approach.
Disclosures
Kato:Chugai: Honoraria; Amgen: Honoraria; Novartis: Honoraria. Sato:Chugai: Honoraria. Imai:Juno Therapeutics: Patents & Royalties; CURED Inc: Consultancy, Patents & Royalties, Research Funding. Horibe:Kyowa Kirin: Consultancy; Amgen: Consultancy, Speakers Bureau; NIPPON SHINYAKU: Consultancy; Pfizer Japan: Consultancy; Astellas Pharma: Speakers Bureau; Chugai Pharmaceutical: Speakers Bureau; Novartis Pharma: Speakers Bureau.