TO THE EDITOR:
Mediastinal gray zone lymphoma (MGZL) is a rare non-Hodgkin lymphoma occurring predominantly in young men.1 MGZL exhibits pathologic characteristics that are intermediate in nature between those of nodular-sclerosis classical Hodgkin lymphoma (NSCHL) and primary mediastinal large B-cell lymphoma (PMBL), and it is characteristically CD30+.2,3 MGZL tumors, as in NSCHL and PMBL, harbor frequent 9p24.1 copy-number alterations and expression of programmed death-1 (PD-1) ligands 1 and (less commonly) 2.4-7 In a small case series of relapsed/refractory (R/R) MGZL, the PD-1 inhibitor pembrolizumab induced a complete metabolic response in 2 patients.6 Gene expression profiling showed that MGZL clusters between NSCHL and PMBL; whole-exome sequencing supports a common cell of origin.8,9 The 5th-edition update of the World Health Organization and the International Consensus Classification exclude cases arising outside the anterior mediastinum, which harbor a different gene expression profile and DNA alterations.10,11 The optimal therapy of MGZL is unknown, and outcomes remain unsatisfactory, with a 2-year progression-free survival (PFS) of 46% and an overall survival (OS) of 92% in 1 multicenter study.12 In another study, patients with MGZL treated with dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab (DA-EPOCHR) had worse outcomes than patients with PMBL, with a 5-year event-free survival of 62% (PMBL, 93%) and an OS of 74% (PMBL, 97%).13
Nivolumab is a fully human immunoglobulin G4 anti–PD-1 immune checkpoint inhibitor monoclonal antibody that restores T-cell–mediated antitumor responses by interrupting PD-1 receptor–ligand interactions.14 The antibody–drug conjugate brentuximab vedotin (BV) consists of monomethyl auristatin E, protease-cleavable linker, and a CD30 antibody, and it induces apoptosis of CD30+ tumor cells.15 BV may also induce an immunogenic environment, contributing to depletion of T regulatory cells and potentiating the effect of PD-1 inhibition.16-19 Nivolumab plus BV has previously demonstrated a high objective response rate (ORR) of 85% as a second-line treatment of transplant-eligible R/R classical Hodgkin lymphoma.20 In Checkmate 436 (ClinicalTrials.gov identifier: NCT02581631), a phase 1/2 study evaluating nivolumab plus BV in R/R non-Hodgkin lymphomas (n = 30), ORR was 73% in patients with R/R PMBL.21 Previously, ORR with BV alone was only 13%.22 Simultaneous targeting of PD-1 and CD30 may be effective in MGZL. We report the efficacy and safety of use of nivolumab plus BV from the CheckMate 436 R/R MGZL expansion cohort.
Patients aged ≥18 years with Eastern Cooperative Oncology Group (ECOG) performance status scores of 0 to 1 and R/R MGZL after autologous hematopoietic stem cell transplantation (auto-HCT), or if transplant ineligible, following ≥2 multiagent chemotherapy regimens, were enrolled. CD30 expression on ≥1% of the tumor or tumor-infiltrating lymphocytes, per local immunohistochemistry on a relapsed specimen (if available), or primary diagnosis was required prior to the first treatment dose. Patients with active, known, or suspected autoimmune disease, a condition requiring systemic corticosteroid treatment (>10 mg daily prednisone equivalent) or other immunosuppressive medications within 14 days of the first dose, were excluded. Patients with previous treatment with BV, other anti-CD30 treatment, allogeneic hematopoietic stem cell transplantation (allo-HCT), radiation therapy within 3 weeks (or chest radiation within 12 weeks) of the first dose, or chemotherapy or therapeutic antibodies within 4 weeks of the first dose were also excluded.
Patients received nivolumab 240 mg and BV 1.8 mg/kg intravenously every 3 weeks until the occurrence of disease progression or unacceptable toxicity. For cycle 1, BV was administered on day 1 and nivolumab on day 8. For cycle 2 and beyond, both were administered on day 1. Primary endpoints were investigator-assessed ORR and safety. Response was assessed according to the Lugano Classification 2014, using positron emission tomography–computed tomography (PET-CT) at weeks 6 and 12, and then at every 9 weeks for the subsequent 4 assessments, and at every 12 weeks after the first year. With an assumed ORR of 50%, the 2-sided 80% confidence interval (CI) was 11.6%-55.2%; the lower bound of the 80% CI excluded 10%, which was the null-hypothesis ORR. Secondary endpoints included complete remission (CR) rate, overall survival (OS), progression free survival (PFS), and duration of response. For OS, patients who were alive or had unknown vital status were censored at the last date they were known to be alive. For other secondary outcomes, patients who received subsequent therapy before documented progression, including auto-HCT or allo-HCT, were censored on the last tumor assessment date before subsequent therapy. All patients provided written informed consent. At each site, approval from the appropriate institutional review board and independent ethics committee was obtained.
The 10 patients in the MGZL cohort were comprised of 6 men and 4 women. The median age was 35 years (range: 25-72; Table 1). Seven had refractory disease (absence of CR after frontline therapy or absence of CR/partial remission with any salvage therapy) at study entry; 1 each had relapsed disease after frontline or salvage therapy; and disease status for the remaining patient was not reported. In addition to CD30, 8 cases were also positive for CD15 and CD20; 2 were negative for both. Patients received a median of 2 (range: 1-3) prior lines of systemic cancer therapy; none included auto-HCT.
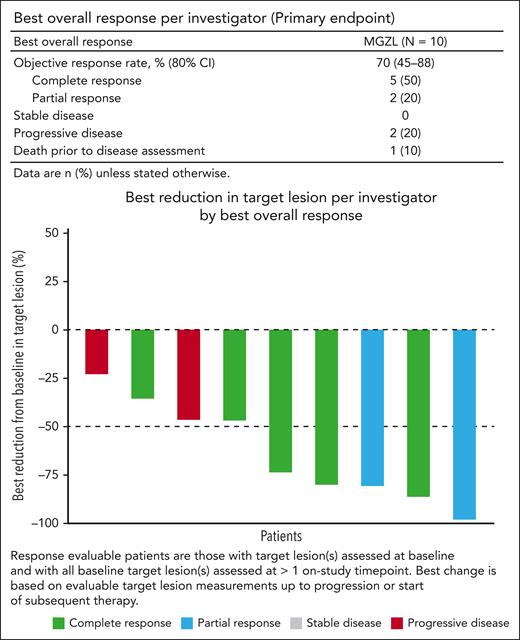
Patients received a median of 7 doses each of nivolumab (range: 5-26) and BV (range: 1-29). At database lock (DBL; February 28, 2020), all had discontinued treatment due to disease progression (n = 5), allo-HCT (n = 4), or auto-HCT (n = 1). One was not evaluable for response because they died before receiving nivolumab (received 1 BV dose); this patient was included in the ORR calculation. At a median follow-up of 12.4 months (range: 0.1-25.5) ORR per investigator was 70% (80% CI, 45%-88%), with 5 achieving CR, 2 achieving partial remission, and 2 exhibiting progressive disease (Figure 1; Supplemental Figure 1). Among those who achieved CR, time to CR ranged from 1.2 to 4.8 months, and duration of CR ranged from 1.5 to 3.2 months. All patients who discontinued treatment due to reaching maximum clinical benefit achieved CR and were censored, as they subsequently received allo-HCT (n = 4) or auto-HCT (n = 1), and all were alive at DBL. Median duration of response, therefore, could not be assessed.
Best overall response and tumor reduction. CI, confidence interval; MGZL, mediastinal gray zone lymphoma.
Best overall response and tumor reduction. CI, confidence interval; MGZL, mediastinal gray zone lymphoma.
At DBL, the median PFS was 21.9 months (95% CI, 0.07-21.9), with 5 patients experiencing events (4 progressive disease, and 1 death from disease progression after 1 cycle of BV; Supplemental Figure 2). The 6-month OS rate was 80.0% (95% CI, 40.9-94.6). The median OS was not reached.
Treatment-related adverse events (TRAEs) occurred in 9 patients, with 3 exhibiting grade 3 TRAEs (1 each of neutropenia, febrile neutropenia, and thrombocytopenia; Supplemental Table 1). TRAEs in ≥2 patients were neutropenia (n = 3), peripheral sensory neuropathy (n = 3), paresthesia (n = 2), thrombocytopenia (n = 2), and anemia (n = 2). Grade 3 febrile neutropenia was the only serious TRAE (n = 1). One patient each experienced an infusion-related reaction (grade 1) and an immune-mediated adverse event (grade 2 maculo-papular rash, resolved without systemic steroids). All 3 deaths were from disease progression.
The high investigator-assessed ORR and CR rate are consistent with those reported with nivolumab plus BV in PMBL (73% ORR; 37% CR) and classical Hodgkin lymphoma as first salvage (85% ORR; 67% CR).20,21 The tolerable safety profile is generally consistent with those established for nivolumab plus BV.18,21 Based on the favorable efficacy and safety profile, this regimen may represent a salvage option for transplant-eligible patients with R/R MGZL.
Acknowledgments
The authors thank the patients and families who made this study possible and the clinical study teams who participated in the trial. The authors also thank Mariana Sacchi, funded by Bristol Myers Squibb, for participating in the data review process.
This study was supported by Bristol Myers Squibb and Seagen. Professional medical writing support for this article was provided by Richard Sora of Caudex, funded by Bristol Myers Squibb.
Authorship
Contribution: A.S., J.L., S.F., and K.J.S. conceived and designed the study; A.S., A.J.M., S.F., C.C.-S., and K.J.S. performed the data acquisition; A.S., A.J.M., S.F., C.C.-S., J.L., S.F., R.W., A.A., and K.J.S. performed the data analysis and interpretation; and all authors contributed to the writing of the article.
Conflicts-of-interest disclosure: A.S. serves on the advisory board for Bayer, Bristol Myers Squibb, Eisai, Gilead Science Inc, Merck Sharp & Dohme, Pfizer, and Servier; is a consultant or serves in an advisory role for Arqule, Incyte, and Sanofi; is a member of a speaker’s bureau for AbbVie, Amgen, Arqule, AstraZeneca, Bayer, Bristol Myers Squibb, Celgene, a Bristol-Myers Squibb Company, Eisai, Eli Lilly, Gilead, Merck Sharp & Dohme, Novartis, Pfizer, Roche, Sandoz, Servier, and Takeda. A.J.M. is a consultant or serves in an advisory role and receives honoraria for/from Affirmed, Imbrium Therapeutics, Janpix Ltd, L.P./Purdue, Merck, Seagen, and Takeda; received research support and/or funding from ADC Therapeutics, BeiGene, Bristol Myers Squibb, Incyte, Merck, Miragen, Seagen, and SecuraBio. S.A.B. is a member of Lymphoma Hub Scientific Review Committee, and Gilead Science Inc. C.C.-S. is a consultant or serves in an advisory role for ADC Therapeutics, Celgene, a Bristol-Myers Squibb Company, Genenta Science, Karyopharm Therapeutics, Roche, and Sanofi; has received honoraria from ADC Therapeutics, AstraZeneca, Bristol Myers Squibb, Incyte, Janssen Oncology, Merck Sharp & Dohme, Novartis, and Takeda; and received research support/funding from ADC Therapeutics, Roche, and Sanofi. J.L. is an employee of and has equity ownership via stock in Seagen. S.F. is an employee of and has stock ownership in Bristol Myers Squibb. R.W. is an employee of and has stock ownership in Bristol Myers Squibb. A.A. is an employee of and has stock ownership in Bristol Myers Squibb. K.J.S. serves on the data and safety monitoring committee for Regeneron; received honoraria from or provided consulting for AbbVie, Bristol Myers Squibb, Janssen, Kyowa, Merck, and Seagen; received research support or funding from Bristol Myers Squibb and Roche; and serves on the steering committee for Beigene. S.F. declares no competing financial interests.
Correspondence: Kerry J. Savage, 600 W 10th Ave, Vancouver, BC V5Z 4E6, Canada; e-mail: ksavage@bccancer.ba.ca.
References
Author notes
Bristol Myers Squibb policy on data sharing may be found at https://www.bms.com/researchers-and-partners/clinical-trials-and-research/disclosure-commitment.html. Seagen policy on data sharing may be found at https://www.seagen.com/healthcare-professionals/clinical-data-requests.
The online version of this article contains a data supplement.
There is a Blood Commentary on this article in this issue.