Abstract
Introduction:U2AF1 mutations (m) are associated with abnormal splicing of genes involved in functionally important pathways, such as cell cycle progression and RNA processing. The U2AF1 gene has specific hotspots for mutations primarily involving the S34F and Q157P residues within the ZnF1 and ZnF2 causing mis-splicing of genes critical for hematopoiesis. Most recently in European Leukemia Net 2022 guidelines, U2AF1m is categorized as high-risk disease with inferior survival. We analyze outcome of U2AF1m in myeloid neoplasms and co-mutation patterns in large cohort of patients treated at Mayo Clinic.
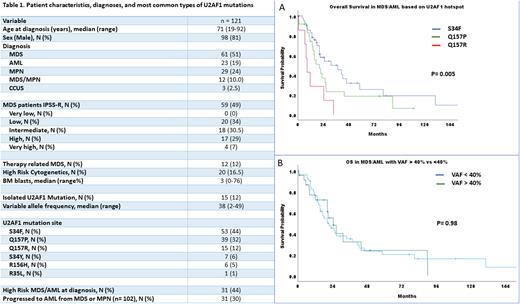
Methods: We reviewed our myeloid neoplasms patients (pts) database who underwent NGS (MC OncoHeme 42 genes panel) testing between October 2015 and August 2021. We identified 121 myeloid neoplasm pts with U2AF1m, and these were analyzed for clinical characteristics, co-mutational patterns, and outcomes using SPSS statistical software. An appropriate IRB approved was obtained.
Results: The median age at diagnosis was 71 years (range [R], 19-92) (Table 1). Sixty-one (51%) pts were diagnosed with MDS, 29 (24%) pts with myeloproliferative neoplasms (MPN), 23 (19%) pts with acute myeloid leukemia (AML), 12 (10%) pts with MDS/MPN overlap and 3 (2.5%) pts with clonal cytopenia of unknown significance (CCUS). Out of 61 pts diagnosed with MDS, 59 pts had risk stratification information based on the revised international prognostic scoring system (IPSS-R): 20 (33.9%), 18 (30.5%), 17 (28.8%) and 4 (6.8%) patients were stratified into low, intermediate, high, and very high risk, respectively. Thirty-one out of 102 (30%) pts with MDS/MPN/MDS-MPN overlap progressed to AML with median time to AML progression 14.6 months (R, 1-118).
Forty-four percent and 32% of pts had mutations involving the S34F and Q157P hotspots respectively, while the remaining had Q157R (12%), S34Y (6%), R156H (5%) and R35L (1%). The median variable allele frequency (VAF) was 38% (R, 2-49). Isolated U2AF1m was seen in 15 (12.4%) patients, 9 of these patients were diagnosed as MDS. The rest of the patients (87.6%) had at least 1 co-mutation, the most common ones being ASLX1 (46%), JAK2 (19%), TET2 (17.5%), RUNX1 (14%), DNMT3A (14%) and BCOR (14%).
We did sub-group analysis for overall survival (OS) in advanced MDS and AML patients harboring most frequent U2AF1 mutations (S34F, Q157P and Q157R). The mOS was 31.3, 20.5 and 8.8 months (mo) in MDS/AML pts with S34F, Q157P and Q157R mutations, respectively (p= 0.005, Figure 1A). While VAF <40% (OS 21.5 mo) vs VAF >40% (OS 24.5 mo) had no differential impact on OS (p= 0.98, Figure 1B).
Conclusion: In this study, we have demonstrated that U2AF1 gene with S34F hotspot have better OS, while Q157R had significantly inferior OS in pts with MDS/AML. Contrary to earlier reports we did not observe significant survival difference in MDS/AML patients with VAF cutoff of 40%.
Disclosures
Al-Kali:Astex: Other: research support to institution. He:Kura Oncology, Inc: Consultancy. Patnaik:Kura Oncology, Stem Line Pharmaceuticals: Research Funding. Shah:Astellas: Research Funding; Celgene: Research Funding; Marker Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.