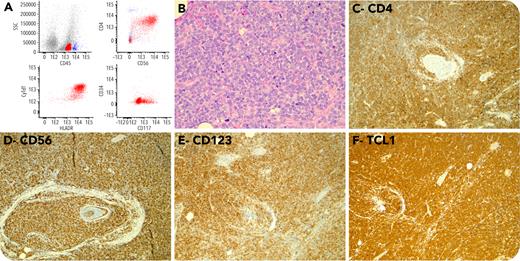
An 87-year-old female presented with small, progressive, red lesion on her thigh (10 × 10 mm) and a slow-growing mass on medial aspect of her left eye (25 × 2 mm). The lesions were not associated with pain or B-symptoms. She had no hepatosplenomegaly or lymphadenopathy and had normal blood counts. Flow cytometry of conjunctival lesion revealed a population of CD45low and low side-scatter cells expressing CD4, CD56, HLADR, and TdT but negative for CD19, CD3, and MPO (panel A). Her conjunctiva biopsy showed diffuse infiltration of tissue with medium-sized blasts (panel B; ×400 magnification). Blasts had dispersed chromatin, small conspicuous nucleoli, and scant cytoplasm with the following immunophenotype: CD2−, CD3−, CD4+, CD10−, CD20−, CD30−, CD43+, CD45+, CD56+, CD123+, CD138−, TCL1+, PAX5−, BCL2+, and EBER-ISH−. Proliferation index by Ki67 was >90%. These findings were consistent with the diagnosis of blastic plasmacytoid dendritic cell neoplasm (panels C-F; ×100 magnification).
Blastic plasmacytoid dendritic cell neoplasm is an aggressive neoplasm with precursor plasmacytoid dendritic cell origin. Skin manifestation is very common and central nervous system involvement is reported in 20% of patients during the course of the disease; however, early manifestation of disease in ocular adnexa is rare.