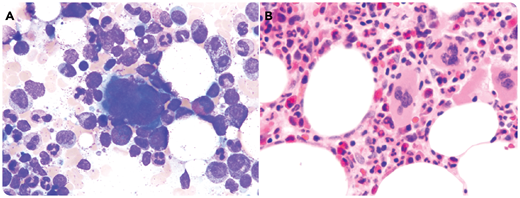
An 82-year-old woman with severe transfusion-dependent macrocytic anemia for 1.5 years was assessed for myelodysplastic syndrome (MDS). She had no radiation, chemotherapy, alcohol or drug usage, lymphadenopathy, or hepatosplenomegaly. Hypothyroidism and vitamin B12 and iron deficiency were ruled out. Her complete blood count showed the following: white blood cells, 5.5 × 109/L; hemoglobin, 76 g/L; mean corpuscular volume, 98.2 fL; reticulocytes, 3 × 109/L; platelets, 336 × 109/L; and neutrophils, 4.09 × 109/L. Blood smear was normal. Bone marrow (BM) aspirate illustrated normal megakaryopoeisis/granulopoiesis without dysplasia. Erythropoiesis was lacking with rare erythroprecursors (panel A; May-Grunwald-Giemsa stain, original magnification ×50). BM biopsy showed absence/markedly decreased erythropoiesis (panel B; hematoxylin and eosin stain, original magnification ×20) confirmed by E-cadherin/hemoglobin A staining. CD34/CD117/MPO/CD3/CD20/Parvo-B19 demonstrated no intrinsic marrow pathology. Flow cytometry demonstrated a mild reversed CD4/CD8 without clonality. T-cell receptor results were nonclonal. Karyotype analysis illustrated monosomy X in 10 out of 20 metaphases. Her history of several pregnancies rendered unrecognized Turner syndrome unlikely. This level of monosomy X (50%) is distinct from the sporadic low levels (<10%) routinely seen in peripheral blood lymphocytes. Monosomy X is reported in MDS/AML as a marker of clonal expansion in BM. Other congenital or secondary causes of pure red cell aplasia (PRCA) were ruled out. A diagnosis of myelodysplastic PRCA was suggested based on the clinical presentations/laboratory tests/BM/cytogenetics.
Myelodysplastic PRCA is an uncommon form of MDS and pathophysiologically distinct from the other types of PRCA.
An 82-year-old woman with severe transfusion-dependent macrocytic anemia for 1.5 years was assessed for myelodysplastic syndrome (MDS). She had no radiation, chemotherapy, alcohol or drug usage, lymphadenopathy, or hepatosplenomegaly. Hypothyroidism and vitamin B12 and iron deficiency were ruled out. Her complete blood count showed the following: white blood cells, 5.5 × 109/L; hemoglobin, 76 g/L; mean corpuscular volume, 98.2 fL; reticulocytes, 3 × 109/L; platelets, 336 × 109/L; and neutrophils, 4.09 × 109/L. Blood smear was normal. Bone marrow (BM) aspirate illustrated normal megakaryopoeisis/granulopoiesis without dysplasia. Erythropoiesis was lacking with rare erythroprecursors (panel A; May-Grunwald-Giemsa stain, original magnification ×50). BM biopsy showed absence/markedly decreased erythropoiesis (panel B; hematoxylin and eosin stain, original magnification ×20) confirmed by E-cadherin/hemoglobin A staining. CD34/CD117/MPO/CD3/CD20/Parvo-B19 demonstrated no intrinsic marrow pathology. Flow cytometry demonstrated a mild reversed CD4/CD8 without clonality. T-cell receptor results were nonclonal. Karyotype analysis illustrated monosomy X in 10 out of 20 metaphases. Her history of several pregnancies rendered unrecognized Turner syndrome unlikely. This level of monosomy X (50%) is distinct from the sporadic low levels (<10%) routinely seen in peripheral blood lymphocytes. Monosomy X is reported in MDS/AML as a marker of clonal expansion in BM. Other congenital or secondary causes of pure red cell aplasia (PRCA) were ruled out. A diagnosis of myelodysplastic PRCA was suggested based on the clinical presentations/laboratory tests/BM/cytogenetics.
Myelodysplastic PRCA is an uncommon form of MDS and pathophysiologically distinct from the other types of PRCA.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org