Background: Minimal Residual Disease (MRD) is a powerful predictor of event-free survival in acute lymphoblastic leukemia (ALL). However, as T-ALL is less common, MRD studies are limited, often with small cohorts, and even fewer have been done by flowcytometry-based MRD (FC-MRD). There have also been different time-points such as Post-Induction (PI-MRD), and late or Post-Consolidation (PC-MRD) that have shown significant correlation with overall, event, and relapse-free survival (OS, EFS & RFS). As the available literature is still not conclusive, we investigated the impact of FC-MRD on survival in childhood T-ALL at a large tertiary cancer care centre in India.
Methods: Children less than 15-years age diagnosed with T-ALL from Jan-2014 to May 2018 were treated uniformly on a modified MCP-841 protocol that included a 4-drug induction (vincristine, prednisolone, l-asparaginase, daunomycin), and consolidation with high-dose cytarabine (24gm/m2 in 3 equal legs for children below 3-years, and 16gm/m2 in two equal legs, for 3 or more years age). Post-consolidation therapy followed the pattern of Interim Maintenance, two Delayed Intensification cycles, and 18 months of Maintenance. Central Nervous System (CNS)-directed therapy consisted of intrathecal methotrexate in all cycles, and those with CNS involvement received additional Cranial Radiation of 18Gy. In early-thymic-precursor (ETP-ALL) immunophenotype patients, dexamethasone replaced prednisolone in Induction. The protocol did not include High-Dose Methotrexate. FC-MRD was estimated by 10-color FC-MRD assay on Navios flow-cytometer (Beckman Coulter, Inc.) at Post-Induction(day-35), and Post-Consolidation(day-78) for those PI-MRD positive(+ve). FC-MRD was analyzed on Kaluza® software v-1.3. Any detectable value was taken as positive. Statistical analysis was performed using MedCalc Statistical Software®.
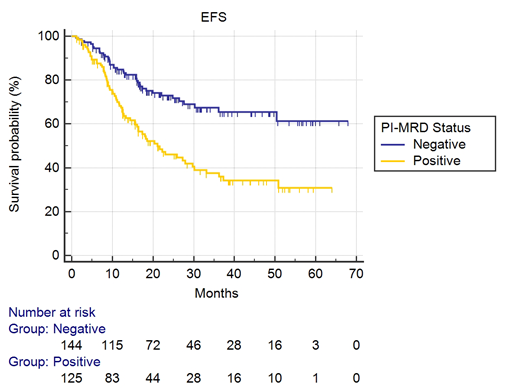
Results: Of 368 eligible patients diagnosed at our centre in the study period, 81 did not undergo PI-MRD (14- Induction deaths, 13- treatment abandonment, 54- referral to other institute/ time-point missed/ did not consent/ other reasons). Another 18 abandoned treatment within 100 days of diagnosis and were also excluded. In the remaining 269, median age was 10-years (range:1-15), M:F-3.8:1. Median presenting WBC was 96.7 x 103/cmm (range:1.14-849), and thirteen patients had ETP. PI-MRD was positive in 125(46%) patients (median MRD -0.3%, range:0.0007-43.6%) of which 58(46.4%) developed medullary relapse, compared to 17 of 144(11.6%) for PI-MRD negative(-ve) patients, with Hazard Ratio (HR) for risk of medullary-relapse for PI-MRD+ve being 5.02(95% CI:3.16-7.96; p<0.0001). Median RFS was 20.5 months (95% CI:16.2-34.7) for PI-MRD+ve patients, while median was not-reached for PI-MRD-ve. PI-MRD+ve patients were at high risk for all events (medullary relapse, extramedullary relapse and death) with an incidence of 53.6% versus 27.8%; p<0.0001, and HR of 2.36 (95% CI:1.6-3.47; p<0.0001). Probability of EFS at 30 months was 68.9% for PI-MRD+ve and 41.1% for PI-MRD-ve patients(Fig-1), while there was no significant difference in 30-month OS, which were 78.7% and 77.9% respectively. Most relapsed/ refractory patients were unable to undergo intensive salvage regimens and/ or hematopoietic stem cell transplants due to socio-economic constraints. When their disease progressed, they were mostly sent home on palliative care on an oral metronomic chemotherapy protocol, on which they survived for varying periods of times. PC-MRD was available in 90 PI-MRD+ patients, and was positive in 28(31%), with median MRD level of 0.055% (range:0.0008-27.6%). PC-MRD+ve patients had significantly shorter RFS (median-14.3 months, 95% CI:7.1-49.7 months), with risk of relapse HR of 2.36 (95% CI:1.6-3.47; p<0.0001). Univariate and multivariate analysis using Cox-hazard model for age, hyperleukocytosis and ETP-immunophenotype showed that PI-MRD was the most significant and an independent high-risk factor for relapse with HR for multivariate analysis being 5.5(95% CI:2.85-11.45; p<0.0001).
Conclusion: We conclude that 10-color FC-MRD done Post-Induction and Post-Consolidation detecting any residual disease reliably identifies those at highest risk of relapse and any other event. PI-MRD+ is an independent, and also the most important risk-factor for any event, and if PC-MRD is also positive, relapse occurs early.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.