Background: Stroke is one of the most devastating complications of sickle cell anemia (SCA). In 1998, the Stroke Prevention Trial in Sickle Cell Anemia (STOP), demonstrated that a high-risk group of children with SCA could be identified using Transcranial Doppler ultrasound(TCD) and that chronic red cell transfusion therapy (CRCT) could reduce the risk of first ischemic stroke in this group by over 90% (Adams, et al NEJM 1998).At STOP studyenrollment, 9.7% of children with SCA were identified as having an abnormal TCD. Baby HUG, (NCT00006400), an NHLBI supported phase III trial showed that severe anemia in SCA was associated with elevated white blood cell (WBC) and higher TCD velocities (Lebensburger, et al Blood 2010 ). It is unclear if lower hemoglobin (Hb) and/or higher WBC are causative of elevated TCD velocities or correlative biomarkers. As new disease therapies become available, it is important to know the current rate of abnormal TCD and characteristics of those patients.
The DISPLACE (Dissemination and Implementation Looking at the Care Environment) project is a multicenter, NHLBI-funded study whose primary purpose is to identify barriers to implementation of stroke screening in SCA and test novel methods for improving outcomes. DISPLACE is a 3-part study: retrospective assessment of current practice, qualitative review of barriers and facilitators to screening and a cluster-randomized intervention implementation project to improve stroke screening. Part 1 of the study showedthat TCD screening rates varied widely among institutions ranging from 30-75.2% (mean 48.4%, median 47%). We are now reporting on the rate of abnormal TCD and the characteristics and outcomes of patients with abnormal TCD.
Methods: DISPLACE is a consortium of 28 US centers. Each site performed a rigorous retrospective chart review of children with SCA aged 2-16 years from 2012-2016. To be eligible for inclusion, children must have been seen at their institution at least 2x during the study period and have confirmation of SCA. A custom electronic data capture (EDC) system facilitated entry of de-identified data including demographics, TCD and MRI results, medications, transfusions, and laboratory values. For children with SCA who had TCD or central nervous system imaging prior to 2012, these results were also entered into the EDC. TCD results were recorded in the EDC as normal, conditional or abnormal based on their institutional interpretation. Labs and vitals were entered for each patient in closest proximity to each TCD. Confirmation and adjudication of each abnormal TCD and associated outcomes were performed. Stroke status was also recorded as well as presence or absence of CRCT.
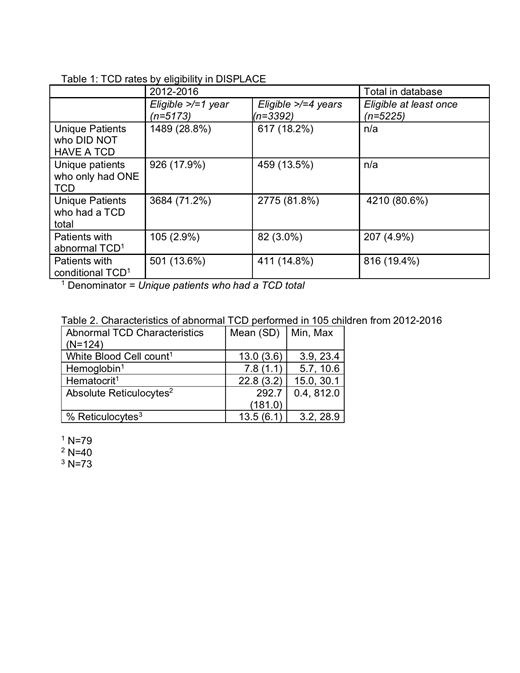
Results: In total, 5247 children with SCA are included in the database of whom 5225 should have received a TCD. Of this cohort, 4210 children (80.6%) had at least one TCD recorded in the database. Within this group, 207 (4.9%) of children had an abnormal TCD and 816 (19.4%) had a conditional TCD. For those children who underwent TCD during the study (2012-2016) period, there were 105 (2.9%) abnormal TCD and 501 (13.6%) conditional TCD (Table 1). The mean age of children at the time of abnormal TCD was 6.6 years (range 2-16 yr). The majority of children were <10 yr at first abnormal TCD. Over 30% of patients with an abnormal TCD were identified as receiving hydroxyurea.The mean Hb associated with an abnormal TCD was 7.8 +/- 1.1g/dl (range 5.7-10.6) and the mean WBC was 13 x109/L+/- 3.6 (range 3.9-23.4) (Table 2). Of the 105 patients with abn TCD during the study period, 18% had a stroke.
Of the total 5247 patients in the database, 3093 (59%) had been prescribed hydroxyurea (HU) and 999 (19%) were prescribed CRCT. CRCT was prescribed most often for abnormal TCD (37%) or secondary stroke prevention (31%).
Discussion: DISPLACE is the largest contemporary cohort of children with SCA. The incidence of abnormal TCD in the DISPLACE cohort is significantly lower than at randomization in the STOP study. The number of children receiving CRCT is higher than expected which may partly account for the decrease in frequency of abnormal TCD.
Many patients with abnormal TCD were receiving HU when their TCD was abnormal and were started on CRCT. Additionally, while the outcomes of children with conditional TCD are still being evaluated, many of those children reverted to normal TCD without intervention. These data may also help us redefine the use and interventions needed for abnormal TCD.
Kanter:NHLBI: Membership on an entity's Board of Directors or advisory committees; bluebird bio, Inc.: Consultancy; SCDAA: Membership on an entity's Board of Directors or advisory committees; Guidepoint Global: Consultancy; GLG: Consultancy; Sangamo: Consultancy, Honoraria; Modus: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Imara: Consultancy; Cowen: Consultancy; Jeffries: Consultancy; Medscape: Honoraria; Rockpointe: Honoraria; Peerview: Honoraria. Adams:GBT: Consultancy, Other: consultancy to companies GBT and Blueburd Bio; Bluebird: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.