INTRODUCTION
Hemophilia A and B are rare X-linked disorders that result in bleeding due to reduced activity of coagulation factor VIII and IX, respectively. With the availability of better medical care and prophylactic treatment modalities, the life expectancy of patients with hemophilia is approaching that of the general population. Patients with hemophilia were initially thought to be protected from cardiovascular disease (CVD) due to hypocoagulable state but this aging population is now known to be at risk for CVD. The primary objective of this study was to determine the incidence of CVD and associated mortality in hospitalized male patients with hemophilia.
METHOD:
We reviewed National Inpatient Sample (NIS) database from 01/2012 to 09/2015 for admissions due to CVD, defined as acute myocardial infraction (AMI) or ischemic cerebrovascular accident (CVA), as a primary diagnosis using International Classification of Diseases, 9th Revision, and Clinical Modification (ICD-9-CM) codes 410.XX for AMI and 433.XX-437.1 for CVA in males age ≥18 years. Hospitalizations with associated diagnosis of hemophilia A or B were identified using ICD-9CM codes 286.0 or 286.1, respectively. We calculated age-, race- and comorbidities- standardized incidence rate of CVD in hospitalizations with or without associated hemophilia using multivariate logistic regression analysis. Baseline clinical characteristics was also compared between the 2 groups in the overall NIS population. Pearson's Chi-square test and t-test was used to compare categorical and continuous variables, respectively. A propensity score match (PSM) analysis was performed to determine the effect of hemophilia on mortality rate in hospitalizations due to CVD. A trend analysis was done to determine the variation in incidence of CVD over the study period. A p-value ≤0.05 was considered significant.
RESULTS:
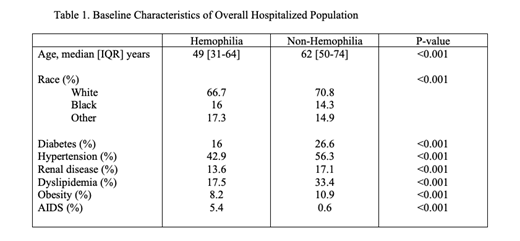
Approximately 50 million (weighted) hospitalizations during the study period were analyzed. A total of 20,845 (0.04%) hospitalizations had associated diagnosis of hemophilia. The baseline clinical characteristics of the overall population is described in table 1. The standardized incidence rate of CVD was significantly lower in hemophilia group 2.9% vs 5.5% (AMI 1.1% vs 2.8% and CVA 1.8% vs 2.7%) compared to non-hemophilia group (p<0.001 for all comparisons). The annual incidence of CVD did not change over the study period in the hemophilia group (trend p=0.906). On PSM analysis, the mortality rate in the CVD associated hospitalizations was not different between the hemophilia and non-hemophilia group, 3.3% vs 4% respectively (OR 0.81 95%CI 0.20-3.3, p=0.772).
CONCLUSION:
We present a large-scale analysis of CVD incidence and outcomes in hospitalized hemophilia (A or B) patients. Although, CVD and its risk factors are statistically less common in patients with hemophilia compared to general hospitalized population, the incidence is still clinically comparable. Moreover, the CVD associated mortality rate is similar. As patients with hemophilia are at higher risk of CVD treatment related adverse effects, further studies on optimal cardio- prevention and treatment strategies are warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.