Abstract
The postthrombotic syndrome (PTS) is a chronic complication of deep vein thrombosis (DVT) that imposes significant morbidity, reduces quality of life, and is costly. After DVT, 20% to 50% of patients will develop PTS, and up to 5% will develop severe PTS. The principal risk factors for PTS are anatomically extensive DVT, recurrent ipsilateral DVT, obesity, and older age. By preventing the initial DVT and DVT recurrence, primary and secondary prophylaxis of DVT will reduce occurrence of PTS. The effectiveness of elastic compression stockings (ECSs) for PTS prevention is controversial. Catheter-directed thrombolysis is not effective to prevent PTS overall but may prevent more severe forms of PTS and should be reserved for select patients with extensive thrombosis, recent symptoms onset, and low bleeding risk. For patients with established PTS, the cornerstone of management is ECS, exercise, and lifestyle modifications. Surgical or endovascular interventions may be considered in refractory cases. Because of a lack of effective therapies, new approaches to preventing and treating PTS are needed. This article uses a case-based approach to discuss risk factors for PTS after DVT, how to diagnose PTS, and available means to prevent and treat PTS, with a focus on new information in the field.
Introduction
The postthrombotic syndrome (PTS) is a form of chronic venous insufficiency (CVI) that develops in 20% to 50% of patients after deep vein thrombosis (DVT) and is severe in up to 5% of DVT cases.1 The clinical manifestations of PTS include a constellation of symptoms and signs, which vary from patient to patient2 (Table 1), and whose severity ranges from minimal discomfort to severe clinical manifestations such as chronic pain, intractable edema, and leg ulceration.1,3 The intensity of symptoms and signs increases over the course of the day and can wax and wane over time.
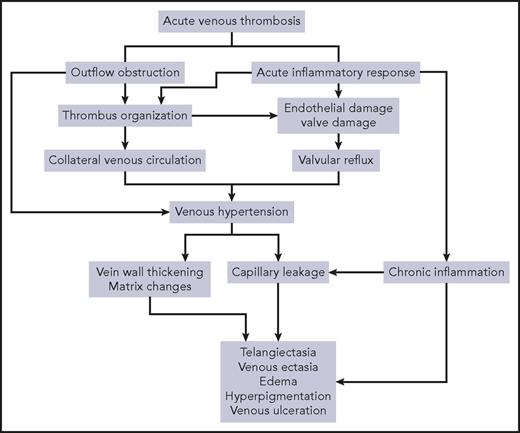
PTS is thought to develop after DVT because of the onset of ambulatory venous hypertension (Figure 1) that leads to reduced calf muscle perfusion and increased tissue permeability, causing chronic edema, tissue hypoxia, progressive calf pump dysfunction, subcutaneous fibrosis, and ultimately skin ulceration.4-9 DVT leads to chronic venous hypertension via 2 principal mechanisms: valvular reflux and residual venous obstruction (RVO). DVT also triggers inflammation-induced valvular damage in involved segments.7-9
PTS carries a significant economic and morbidity burden. Total treatment costs (including imaging studies, laboratory and pathology testing, pharmacy claims, and hospital admissions, which are the main cost driver) are significantly higher in DVT patients who have PTS as compared with DVT patients without PTS.10,11 PTS has also been shown to negatively impact health-related quality of life (QOL), with worsening scores as severity of PTS increases. Notably, PTS patients report QOL scores that are comparable to severe chronic medical conditions such as diabetes and congestive heart failure.12-14
The first “How I treat PTS” article was published in this journal in 2009.1 PTS is increasingly recognized as a frequent and important outcome of DVT. Recent studies have improved understanding of the epidemiology, risk factors, and prevention and treatment approaches to PTS. In 2014, the first evidence-based guidelines focused solely on PTS were published by the American Heart Association.15 This updated review will elaborate on recent advances in knowledge, focusing on PTS of the lower limbs in adults.
Case presentation 1
A 46-year-old man presents to the Thrombosis Clinic 1 month after being diagnosed with a first unprovoked proximal DVT. He presented to the emergency room 1 month ago with a 24-hour history of acute left leg pain and swelling. On compression ultrasonography a left iliofemoral DVT was diagnosed. Anticoagulation with low-molecular-weight heparin (LMWH) was started in the emergency room, and he was transitioned to a vitamin K antagonist (VKA) by his primary care physician. The patient is obese (body mass index [BMI] 36), is a nonsmoker, and has no family history of venous thromboembolism (VTE). He denies any leg symptoms or signs prior to the acute DVT. He works as a chef and owns a restaurant, spending most of the workday standing. At his clinic visit, he complains that he still experiences left leg pain intermittently and that his leg is still swollen and turns red at the end of the day. He is still having trouble walking and cannot complete a full day at work. On examination, his left leg is swollen from the midthigh down, dilated superficial veins are seen, and no color changes are observed. The thigh and calf are warm and sensitive to palpation. Good peripheral pulses are palpated. On review of the patient's labs, his weekly international normalized ratios (INRs) have been consistently subtherapeutic, never reaching 2.0.
Can a diagnosis of PTS be established at this point?
There is no specific recommended time limit to diagnose PTS. However, in some patients, it can take a few months for the initial pain and swelling associated with acute DVT to resolve; thus a diagnosis of PTS should be deferred until after the acute phase (3-6 months).16
Can we predict the risk for PTS development in this patient?
Because risk factors for PTS are incompletely understood, it is difficult to predict, on an individual basis, which patients with DVT will develop PTS. In the past few years, however, new information has been gained about clinical and biologic factors that influence the risk of developing PTS. This information is summarized subsequently, grouped according to time points of follow-up after acute DVT.
Risk factors apparent at the time of DVT diagnosis
Risk of PTS is higher (two- to threefold) after proximal (especially with involvement of the iliac or common femoral vein) than distal (calf) DVT.17,18 Preexisting primary venous insufficiency increases the risk of PTS up to twofold.19-21 Elevated BMI (>30) more than doubles the risk of PTS.19,21-24 Older age increases the risk of PTS from 30% to threefold.21-23,25 Conversely, the following factors appear to have no or little effect on the risk of developing PTS: sex, whether DVT was provoked vs unprovoked, and inherited thrombophilia.15,19,21,24,26,27
Recently, our group derived a clinical prediction rule for PTS in patients with a first proximal DVT, using the SOX Trial cohort. High-risk predictors at the time of DVT diagnosis were the following: index DVT in iliac vein, BMI ≥35 kg/m2, and moderate-severe Villalta severity category (described subsequently) at DVT diagnosis as reflective of the severity of acute DVT symptoms and signs. Compared with patients with a score of 0, those with a score of ≥4 had an odds ratio of 5.9 (95% confidence interval [CI], 2.1-16.6) for developing PTS.28 Validation of the SOX-PTS index in a separate population of proximal DVT patients is currently underway.
Risk factors related to treatment of acute DVT
Insufficient (ie, subtherapeutic) anticoagulation with VKAs during the first 3 months of DVT treatment increases the risk of PTS approximately twofold.23,29 It has been suggested that LMWHs may be more effective than VKAs for PTS prevention.30 Whether treatment of DVT with direct oral anticoagulants (DOACs) is more effective than VKAs in preventing PTS is still an unanswered question. A post hoc analysis of a subpopulation of the Einstein study failed to demonstrate a statistically significant reduction in the risk for PTS in the rivaroxaban treatment group vs LMWH/VKA.31 In contrast, a recent small retrospective observational study suggested a lower incidence of PTS in patients treated with rivaroxaban compared with warfarin.32 Currently, possible better protection against PTS is not in itself a valid reason to choose one available parenteral or oral anticoagulant over another.
Risk factors apparent during follow-up after acute DVT
Ipsilateral DVT recurrence increases risk of PTS by four- to sixfold.22,23,26,33 Persistent venous symptoms and signs 1 month after acute DVT increases risk of subsequent PTS.23,34
Conflicting evidence exists regarding the role of RVO and/or valvular reflux on compression ultrasonography as predictors of PTS. RVO on ultrasound (eg, 3-6 months after acute DVT) was found to modestly (1.5- to twofold) increase the risk of PTS. The presence of reflux has also been suggested to be an independent predictor of PTS.35-42
Some inflammation markers, such as C-reactive protein (CRP); interleukin-6 (IL-6), IL-8, and IL-10; and intercellular adhesion molecule (ICAM)-1, and higher levels of matrix metalloproteinase (MMP)-1 and MMP-8, measured at varying time points after DVT diagnosis have been found to be associated with a higher risk of PTS.43-47 Whether d-dimer might be a useful marker to predict the development of PTS after DVT is not yet established.48
Returning to our patient, it is evident that he has at least 4 established risk factors for PTS: extensive proximal DVT, high BMI, poor early INR control, and persistent venous symptoms and signs 1 month after DVT. He should thus be considered to be at high risk for PTS development, and closer monitoring should be initiated, along with efforts aimed at PTS prevention.
Can PTS be prevented in this patient?
Rigorous INR monitoring is recommended, particularly during the first 3 months of VKA treatment.16 Because recurrent ipsilateral DVT is an important risk factor for PTS, preventing recurrent DVT by providing optimal anticoagulation of appropriate duration for the initial DVT is an important goal.49 Data are insufficient to make specific recommendations regarding choice of anticoagulant (ie, VKA vs DOAC vs LMWH monotherapy) on the outcome of developing PTS.
Elastic compression stockings (ECSs), by reducing edema and venous hypertension, could plausibly play a role in preventing PTS. However, there are conflicting data on this topic. Two small, randomized, open label trials reported that wearing 30 to 40 mm Hg knee-high ECSs for at least 2 years after proximal DVT was effective in preventing PTS.26,50 Subsequently, a large, multicenter, randomized, placebo controlled trial showed no benefit of active ECSs, worn for 2 years after proximal DVT, to prevent PTS: rates of PTS, recurrent VTE, and QOL scores were similar in the active and placebo stockings groups.51 This is the largest and only placebo controlled study to date to directly assess the effectiveness of ECSs for prevention of PTS; however, self-reported daily adherence with ECSs was less than that reported in earlier trials that showed a benefit.52 In the OCTAVIA study, a multicenter, single blind, noninferiority, randomized trial, a 12-month period of ECSs use was not noninferior to 24 months in decreasing PTS risk,53 suggesting that longer periods of ECS use after DVT may still have a role in PTS prevention. Recently, the IDEAL DVT trial, a multicenter, randomized, single blind, noninferiority trial comparing the effectiveness of individualized duration of ECSs (based on an algorithm that took into account the Villalta score at 3, 6, or 12 months) with standard duration (24 months) of ECSs for the prevention of PTS, concluded that shortened ECS therapy was noninferior to 2 years of therapy.54 The authors propose that the seemingly conflicting outcomes of the OCTAVIA and IDEAL-DVT trials stem from the fact that the treatment effect of longer duration ECSs in the OCTAVIA trial might be directed at mild PTS. However, as both of these trials lacked a no ECS arm, it needs to be acknowledged that uncertainty remains as to whether ECSs have an effect on PTS prevention. A recent Cochrane systematic review concluded that low-quality evidence suggests that ECSs may reduce the occurrence of PTS after DVT.55 Pooled analysis of 5 studies including 1393 patients found that use of ECSs led to a reduction in the incidence of PTS (risk ratio [RR], 0.62; 95% CI, 0.38-1.01). In light of the current state of evidence, and consistent with international consensus guidelines,15,49 we do not routinely prescribe ECS to all DVT patients. Our approach is to prescribe a trial of 20 to 30 mm Hg or 30 to 40 mm Hg below-knee ECSs to patients who have residual leg swelling or discomfort after proximal or distal DVT, such as in our patient, monitor the patient’s symptoms, and continue ECSs for as long as the patient derives symptomatic benefit or is able to tolerate them. Contraindications to ECSs include severe symptomatic peripheral arterial disease and allergy to stocking material. Patients should be educated on how to apply and use ECSs and on the importance of compliance to maximize their benefit.
In light of the role of inflammation in PTS development, drugs with anti-inflammatory properties could have a preventive effect on PTS, but this requires investigation in well-designed randomized controlled trials (RCTs). The presumed anti-inflammatory properties of LMWH make this anticoagulant an option for further study; however, other candidate drugs are emerging. A randomized study of 234 patients with acute DVT reported that addition of a statin (rosuvastatin) to LMWH monotherapy was associated with a significantly lower risk of PTS at 3 months than LMWH monotherapy alone (38.3% vs 48.5%).56 In that study, significantly lower levels of CRP in the rosuvastatin group after 3 months of treatment point to a possible protective effect through reduced inflammation. This protective effect was also suggested in a murine venous stasis model, where a 25% reduction of thrombus burden was reported in mice treated with statins.57 The ongoing SAVER trial (#NCT02679664) will provide important data on the impact of statins to prevent PTS.
Patients with iliofemoral DVT have an increased risk of PTS (2-year PTS rates of 50% or greater)17,18 and are also more likely to develop severe PTS manifestations such as venous claudication and venous ulcers.24,58 Therefore, such patients may require more aggressive initial DVT treatment to reduce the risk of PTS. In addition to optimal anticoagulation, various options for early clot removal can be considered. The use of systemic thrombolytic therapy to treat acute proximal DVT is not recommended because of 3 to 4 times increased rates of major bleeding over anticoagulation alone.59-61 Catheter-directed thrombolysis (CDT) or pharmacomechanical CDT (PCDT; CDT plus mechanical disruption of thrombus) are safer than systemic thrombolytic therapy and have been studied for PTS prevention after extensive proximal DVT. In a multicenter RCT (CaVenT study), the use of additional CDT in anticoagulated patients with acute iliofemoral DVT was associated with a statistically significant (P = .047) 26% relative reduction (14% absolute reduction) in risk of PTS at 2 years, at the cost of an additional 3% rate of major bleeding. The absolute risk reduction increased to 28% after 5 years, and the number needed to treat decreased from 7 to 4. However, 41% of CDT patients still developed PTS, indicating that CDT does not eliminate the risk of PTS, and CDT did not result in improved QOL at 2 or 5 years’ follow-up.62-64 A recent systematic review found that adding thrombolysis (systemic, locoregional, or catheter-directed) to anticoagulation increased vein patency and reduced the incidence of PTS after DVT by approximately one-third, at the cost of a more than twofold higher risk for bleeding and no differences in QOL.65 Very recently, results of the ATTRACT study were published. In this multicenter trial of PCDT plus standard anticoagulation vs standard anticoagulation alone to prevent PTS, the addition of PCDT did not prevent PTS (47% of PCDT group vs 48% of no PCDT group after 2 years of follow-up; RR, 0.96; 95% CI, 0.82-1.11) but did increase bleeding (major bleeding within 10 days occurred in 1.7% vs 0.3%; P = .049). Although PCDT did reduce the severity of PTS (moderate-to-severe PTS [Villalta score ≥10] occurred in 18% vs 24% [RR, 0.73; 95% CI, 0.54-0.98]), change in QOL did not differ between the treatment groups.66 Current guidelines (published prior to the results of the ATTRACT study) suggest that in select patients with extensive acute proximal DVT who have good functional status and a low risk of bleeding, CDT or PCDT followed by standard anticoagulant therapy may be considered, providing that appropriate expertise and resources are available.49 In view of the results of the ATTRACT trial, because of insufficient evidence for long-term efficacy and potential to cause bleeding, CDT is not recommended for most patients with proximal DVT. However, it may be considered in patients with very severe DVT in which the arterial circulation is compromised (phlegmasia cerulea dolens), because CDT is likely to be associated with a lower risk of major bleeding than systemic thrombolysis. CDT could also be considered on a case by case basis in patients <65 years old with extensive (eg, iliofemoral or iliac vein) acute proximal DVT who have good functional status and a low risk of bleeding.
Case presentation 2
A 60-year-old woman known for hypothyroidism and obesity (BMI 35) was diagnosed with an unprovoked first episode of left proximal DVT 7 months ago. She is an elementary schoolteacher. After DVT diagnosis, treatment with rivaroxaban was started, and she has been compliant with therapy. She is referred to the thrombosis clinic for consultation regarding continued leg symptoms. She still has not been able to return to working full time and spends many hours sitting or lying down at home because of continued leg pain and leg heaviness while walking. She has gained 6 pounds because of her sedentary lifestyle. She reports itching and cramping in her left leg and swelling and redness of her entire lower leg especially at the end of the day, and she recently noticed an area of skin breakdown on the inner part of her left shin. On examination, edema, redness, and hyperpigmentation of the left lower extremity are seen, as well as a small venous ulcer in the medial left perimalleolar area.
How is PTS diagnosed?
There is no objective diagnostic test for PTS, which is primarily diagnosed on clinical grounds in a patient with manifestations of CVI and a previous episode of DVT at least 3 months previously. A number of clinical scales have been used to help diagnose and define PTS. Of these, 3 were developed specifically for PTS: the Villalta scale,67 Ginsberg measure, and Brandjes scale. The others, developed for chronic venous disease, include the clinical, etiological, anatomic, pathophysiological classification; Venous Clinical Severity Score; and Widmer scale.15 Most scales have not been formally validated and are not able to differentiate PTS from other causes of CVI. The reported prevalence of PTS can vary widely from one study to another according to the diagnostic tool used to assess PTS.
To facilitate cross-study comparisons, guidelines from the International Society on Thrombosis and Haemostasis recommend using the Villalta scale to diagnose PTS and grade its severity68 (Table 2). Two different methods for PTS assessment with the Villalta scale are currently used: in the first, a single Villalta score assessment >4 is sufficient to make the diagnosis, whereas in the second, to take into account that PTS signs and symptoms can wax and wane over time and to better capture clinically persistent PTS, 2 consecutive scores >4 measured 3 months apart are used to make the diagnosis.69 The Villalta PTS scale has been shown to be valid, reproducible, and responsive to clinical change and shows good correlation with generic and disease-specific QOL scores,10,70 as well as anatomic and physiological markers of PTS.35
Our case 2 patient has a Villalta score of 15 and a venous ulcer and thus qualifies for the diagnosis of severe PTS.
Treatment of established PTS
As few treatment strategies for established PTS have been studied in well-designed clinical trials, there is a lack of evidence-based management options.
Should anticoagulation be continued solely because of the presence of PTS?
Although it is common clinical practice to prolong anticoagulation in patients with (severe) PTS, it is uncertain whether having PTS increases the risk of ipsilateral recurrent VTE after stopping anticoagulation. A prospective study that addressed this question found a 2.6 (95% CI, 1.2-5.9) times increased risk of recurrent VTE in patients with PTS compared with those without PTS.24 However, in a recent cohort study of 869 consecutive patients with proximal DVT, although patients with PTS had longer durations of anticoagulation, they were not found to have an increased risk of recurrent VTE, adjusted for duration of anticoagulation (hazard ratio of recurrent VTE in patients with vs without PTS was 1.14 [95% CI, 0.81-2.36]).71 Providing anticoagulation of appropriate duration for treatment of the initial DVT is recommended as a means of reducing the risk of recurrent ipsilateral DVT and consequent PTS.15 There is no consensus on the value of extending anticoagulation in patients with established PTS beyond the durations recommended for the treatment of DVT.49
Exercise and lifestyle
Two small trials suggest that exercise training may benefit patients with PTS. In a study of 30 patients with CVI (half had prior DVT), a 6-month leg muscle strengthening exercise program led to improved calf muscle function and calf muscle strength.72 In a randomized pilot trial, a 6-month program of exercises to increase leg strength, leg flexibility, and overall cardiovascular fitness improved PTS severity, QOL, leg strength, and leg flexibility, with no adverse events.73
Additional lifestyle advice to patients with PTS includes promoting venous return by avoiding a sedentary lifestyle, elevating the legs when seated or in bed when lying down, avoiding prolonged exposure to heat, maintaining a nonobese body weight, and using a moisturizing cream to avoid skin dryness and subsequent skin breakdown.
Compression therapy
In contrast to the uncertainty surrounding their use for PTS prevention, ECSs play a role in PTS treatment, although their use is based primarily on extrapolation from patients with primary CVI, the low risk of harm and the possibility of benefit to at least some PTS patients. ECSs have been reported to reduce symptoms of CVI such as limb swelling and contribute to functional improvement.74 An initial therapeutic trial of 20 to 30 mm Hg knee-length ECSs can be followed by stronger pressure (30-40 or 40-50 mm Hg) stockings if lower pressure stockings are ineffective.15
Medications
Venoactive drugs that have been considered for the treatment of PTS include rutosides (thought to reduce capillary filtration and microvascular permeability), defibrotide (downregulates plasminogen activator inhibitor-1 release and upregulates prostacyclin, prostaglandin E2, and thrombomodulin), and hidrosmin (mechanism of action unknown). A systematic review and metaanalysis of 4 randomized trials that evaluated the effectiveness of these drugs for PTS found low-quality evidence to support their use, as studies were limited by a high degree of inconsistency and imprecision. Furthermore, drug treatment was usually of short duration (eg, 8 weeks to a few months), and potential long-term side effects are unknown.77 A more recent systematic review concluded that there was no evidence that rutosides were superior to the use of placebo or ECSs.78 Currently, there is limited and low- or very low-quality evidence that venoactive medications reduce symptoms of PTS. Further, there is no evidence that use of diuretics is effective for the treatment of PTS-related edema.15
Venous ulcer management
Five percent to 10% of DVT patients will develop severe PTS, which can include venous leg ulcers.15 Venous ulcers significantly impair patients’ QOL79 and impose a marked economic burden on society. They account for ∼2 million lost workdays annually in the United States.80 The average annual cost of treatment of a single venous ulcer is estimated at $10 000.81 Patients with postthrombotic ulcers should be managed by a multidisciplinary team approach that ideally includes an internist, dermatologist, vascular surgeon, and wound care nurse.15 Postthrombotic venous ulcers are treated with compression therapy,74 leg elevation, topical dressings, and pentoxifylline, a pharmacologic agent considered to improve tissue blood flow and oxygen delivery,82 and may require weeks to months to heal. Ulcers can be refractory to therapy and often recur. Surgery or endovascular procedures may be advocated in selected patients with venous ulcers refractory to conservative management.15
Endovascular and surgical options
Although the pathogenesis of PTS is complex and some venous changes are irreversible, 2 elements may be amenable to endovascular correction: (1) stent placement for chronic iliac vein obstruction, which can enhance outflow and thereby reduce venous pressures. A meta-analysis of nonrandomized studies and case series found that stent placement in PTS patients (n = 1118) with chronically occluded iliac veins was associated with resolution of pain, swelling, and ulcer in two-thirds of stented patients83 ; and (2) saphenous vein reflux, which is amenable to endovenous thermal (radiofrequency or laser) ablation,84 foam sclerotherapy, and venous stripping of the refluxing saphenous vein.85 Depending on DVT location, venous bypass surgery could be promising, but there are no RCTs comparing the effectiveness and safety of operative vs conservative treatment.86,87
Overall, in selected patients with severe PTS, endovascular or surgical treatments can be considered for symptom relief if conservative management fails and if appropriate expertise is available; however, the lack of good-quality evidence prevents robust recommendations regarding these procedures. The Chronic Venous Thrombosis: Relief With Adjunctive Catheter-Directed Therapy (C-TRACT) Trial (#NCT03250247) is an ongoing RCT aimed to determine if the use of endovascular therapy is an effective strategy to reduce PTS severity and improve QOL in patients with iliac-obstructive PTS.
In our patient, 20 to 30 mm Hg knee-length ECSs were prescribed at the clinic visit. She was also enrolled in an exercise and weight loss program 3 times a week. Using a multidisciplinary approach, she was referred to a dermatologist and a vascular surgeon for assessment and treatment of her venous ulcer. In accordance with current guidelines42 and after discussion with the patient, anticoagulation was continued because of the unprovoked nature of her DVT and perceived low risk of bleeding. On a repeat visit to our clinic 2 months later, she reported wearing ECSs almost daily, and she lost 4 pounds and felt better overall. She was still experiencing intermittent leg pain; however, it was milder and she was able to spend more time at work. Her venous ulcer was smaller in size and healing. She continues follow-up in our clinic to monitor her progress.
Conclusions and research needs
PTS is a frequent complication of DVT that has the potential to reduce QOL, leads to chronic functional disability, and poses difficult management challenges. PTS-related research needs are substantial. Important subjects for future research are summarized in Table 3.
Acknowledgments
S.R.K. is supported by a Tier 1 Canada Research Chair and is an investigator of the CanVECTOR (Canadian Venous Thromboembolism Clinical Trials and Outcomes Research) Network, which receives funding from the Canadian Institutes of Health Research.
Authorship
Contribution: A.R. and S.R.K. conceived this article; A.R. performed the literature review and wrote the manuscript; and A.R. and S.R.K. reviewed and edited the final manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Anat Rabinovich, Hematology Department, Soroka University Medical Center, POB 151, Beer-Sheva 84101, Israel; e-mail: drrabino@bgu.ac.il.