Abstract
Tissue factor (TF), an integral membrane protein, binds factor VIIa (FVIIa) and the FVIIa/TF catalytic complex is responsible for the initiation of coagulation and enhances the inflammatory response by inducing cell signaling through protease activated receptor-2. Tissue Factor Pathway Inhibitor (TFPI) is an important endogenous regulator that produces FXa-dependent feedback inhibition of the FVIIa/TF complex and directly inhibits FXa. Through alternative mRNA splicing, TFPI is expressed in several isoforms, which possess unique functional properties and are present at different locations. TFPIα contains three Kunitz-type protease inhibitory domains (K1, K2, K3) and a basic C-terminus. It is a soluble form that produces FVIIa/TF inhibition (through K1) and whose inhibition of FXa (through K2) is dramatically enhanced by protein S (PS, through K3 binding). TFPIβ is a GPI-anchored cell surface form (containing K1 and K2) that inhibits FVIIa/TF and inhibits FXa well in the absence of PS. TFPIγ is a soluble two Kunitz domain (K1, K2) form that inhibits FVIIa/TF, but inhibits FXa weakly. It is expressed in the mouse, but not in man.
Our initial TFPI gene-disruption in mice targeted the K1 domain in all expressed TFPI isoforms. Due to alternative mRNA splicing, this disrupted gene continues to express forms of TFPI (at ~50% the normal plasma level) that lack the K1 domain (TFPIΔK1) and thus do not inhibit FVIIa/TF. TFPIK1(-/-) gene-disrupted mice die in utero of intravascular coagulation and a consumptive coagulopathy. We have rescued TFPIK1(-/-) mice using a Tie2-hTFPIα transgene that directs endothelial cell and hematopoietic cell expression of hTFPIα . Rescued mice reproduce and appear healthy. The level of hTFPIα in the plasma and blood platelets (at 7.5 x 108/mL) of Tie2-hTFPIαtransgene rescued TFPIK1(-/-) mice is 15.3 + 4.4 and 24.7 + 3.6 pM (at 7.5x108/mL platelets). These values are 1/4 and 1/3 the levels of mTFPIα in normal animals, respectively. Further, hTFPIα is at least 3-fold less active than mTFPIα in mouse plasma thrombin generation assays induced with mouse thromboplastin or mouse FXa. Therefore, we refer to these Tie2-hTFPIαtransgene rescued TFPIK1(-/-) mice as "Low TFPI mice." All mice used in the studies below were in the C57Bl/6 (B6) genetic background.
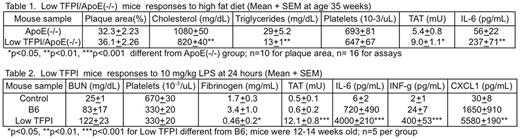
An earlier study had noted a modest, localized increase in atherosclerosis in 34 week old TFPIK1(+/-)/ApoE(-/-) mice fed a normal diet. For the study reported herein, Low TFPI/ApoE(-/-) and ApoE(-/-) mice were fed a high fat (25.2% by weight) diet from weaning. At 35 weeks of age, compared to the ApoE(-/-) mice the Low TFPI/ApoE(-/-) mice had developed significantly increased thrombin-antithrombin (TAT) and interleukin-6 (IL6) levels, but, surprisingly, reduced cholesterol and triglyceride levels, and no significant difference in atherosclerotic plaque area (see Table 1 below). Thrombi were not detected in tissues, including the innominate artery in either mouse strain.
Injection of lipopolysaccharide (LPS) in mice has been used extensively in investigations of the innate immune response and of the role of coagulation-related proteins in acute endotoxemia. Low TFPI and control B6 mice respond similarly to a low, sub-lethal 2.5 mg/kg (IP) LPS challenge. Studies with increasing doses of LPS show Low TFPI mice are ~5 times more sensitive to LPS with respect to mortality (LD50 ~4 vs. 20 LPS mg/kg). At a 10 mg/kg LPS challenge, Low TFPI mice have significantly increased TAT, IL6 and INF-γ, and CXCL1 levels compared to B6 mice at 24 hours (see Table 2 below).
I n summary, concomitant Low TFPI in fat-fed ApoE(-/-) mice was associated with increased procoagulant (TAT) and cytokine (IL-6) biomarkers, but no increase in atherosclerosis. The latter result was potentially confounded by reductions in cholesterol and triglycerides in the Low TFPI/ApoE(-/-) mice. Low TFPI mice show similar cytokine responses as WT mice to a low-dose, sub-lethal endotoxin challenge, but are markedly more sensitive to high-dose endotoxin challenge.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.